Patient will present with → a 55-year-old man with a history of gastroesophageal reflux disease (GERD) presents with progressive difficulty swallowing solid foods over the past 6 months. He denies any weight loss, night sweats, or hematemesis. Upper endoscopy reveals a benign-appearing esophageal stricture. Biopsies are taken and confirm the benign nature of the stricture.
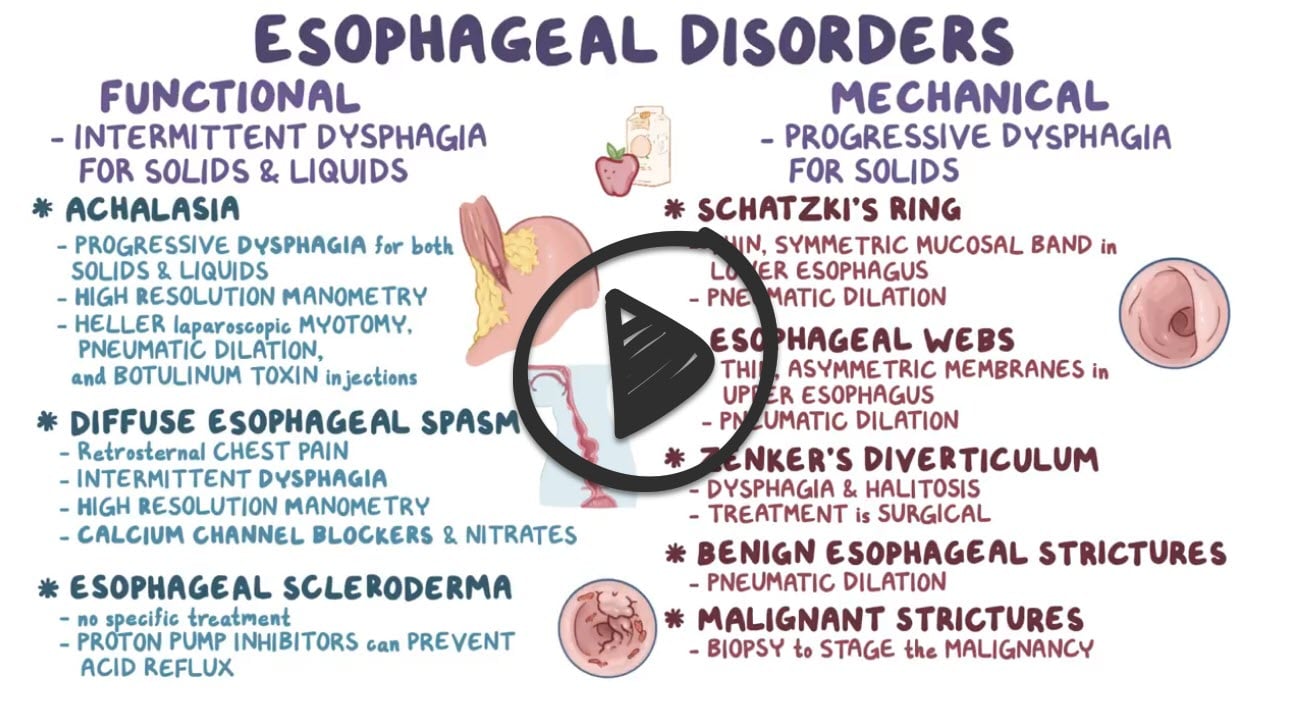
An esophageal stricture is an abnormal tightening or narrowing of the esophagus making it more difficult for food to travel down the tube. People with esophageal strictures may have pain or difficulty swallowing
- It can be caused by or associated with gastroesophageal reflux disease, esophagitis, a dysfunctional lower esophageal sphincter, disordered motility, or a hiatal hernia
- Strictures can form after esophageal surgery and other treatments such as laser therapy or photodynamic therapy
- Dysphagia to solids that is only gradually progressive is suggestive of an esophageal stricture
- The majority of esophageal strictures result from benign peptic strictures from long-standing gastroesophageal reflux disease (GERD), which accounts for 70 to 80% of adult cases
An esophageal web is a thin mucosal membrane that grows across the lumen in the mid-upper esophagus and may cause dysphagia. It may be congenital or acquired
- Plummer–Vinson syndrome is a rare disease characterized by difficulty swallowing, iron-deficiency anemia, glossitis, cheilosis, and esophageal webs
A lower esophageal ring (also called a Schatzki ring) is a 2- to 4-mm mucosal stricture that causes a ringlike narrowing of the distal esophagus at the squamocolumnar junction that often causes dysphagia.
- Most patients have intermittent, gradually progressive dysphagia for solid food that occurs while consuming a heavy meal with meat that was “wolfed down,” hence the pseudonym the “steakhouse syndrome”
Esophageal tumors (benign esophageal tumors or esophageal cancer) can also cause dyspagia
Diagnosed by upper endoscopy to determine the underlying cause, exclude malignancy, and perform therapy (dilation) if needed
- Barium contrast esophagram (barium swallow) can be used as the initial test (prior to upper endoscopy) in patients with clinical features of proximal esophageal lesion or known complex (tortuous) stricture
Endoscopy and dilatation - rarely patients will need surgery
- It can sometimes be treated with other medications. For example, an H2 antagonist or a proton-pump inhibitor (e.g. omeprazole) can treat underlying acid reflux disease
Question 1 |
Corrosive ingestion Hint: Corrosive strictures account for less than 5% of all cases of esophageal stricture. | |
Gastroesophageal reflux disease (GERD) | |
Postoperative scarring Hint: Postoperative scarring account for about 10% of all cases of esophageal stricture | |
Esophageal cancer Hint: Esophageal cancer is not the most common cause of esophageal stricture. |
Question 2 |
GERD | |
Adenocarcinoma | |
Scleroderma | |
Infectious esophagitis |
Question 3 |
Achalasia Hint: Achalasia is a possible cause, but the history of GERD makes strictures the most likely diagnosis. | |
Diffuse esophageal spasm (DES) Hint: DES is also a possible cause, but the history of GERD makes strictures the most possible cause. | |
Pyloric stenosis Hint: Pyloric stenosis occurs in neonates/infants. | |
Esophageal stricture |
Question 4 |
Proton Pump Inhibitor Hint: is used in the initial treatment of esophageal stricture | |
Endoscopic dilatation Hint: is a definitive treatment | |
Endoscopic intralesional steroid Hint: commonly used for refractory strictures. | |
Endoscopic sclerotherapy |
Question 5 |
solids | |
liquids | |
both solids and liquids |
Question 6 |
Esophageal webs | |
Mallory-Weiss tear | |
Barrett's Esophagus | |
Varices | |
A solid tumor |
|
List |
References: Merck Manual · UpToDate


 Osmosis
Osmosis