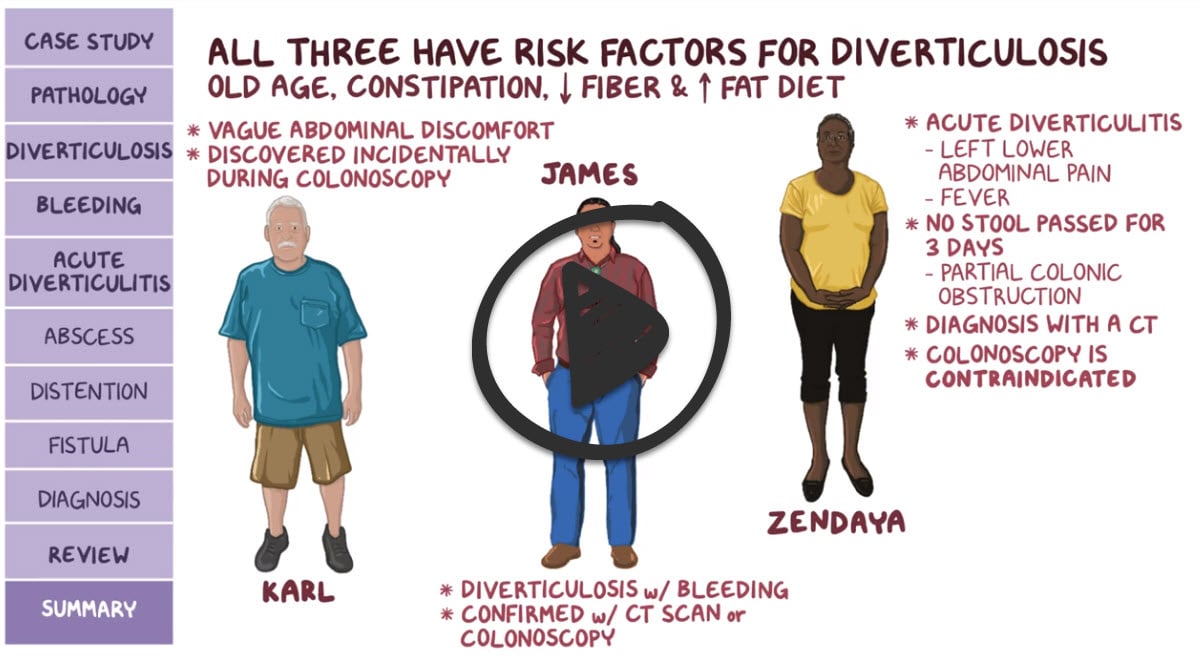
Diverticulitis will present as → a 67-year-old man with a long history of constipation presents with steady left lower quadrant pain. Physical exam reveals low-grade fever, mid-abdominal distention, and lower left quadrant tenderness. Stool guaiac is negative. An absolute neutrophilic leukocytosis and a shift to the left are noted on the CBC.
Diverticulosis will present as → a 63-year-old male who is being evaluated in the emergency department for an episode of painless, bright red blood per rectum for two hours.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Diverticulosis is defined as large outpouchings of the mucosa in the colon
- Presents with painless rectal bleeding, particularly in an elderly patient
- Seeds and nuts — Nut, corn, and popcorn consumption are not associated with an increase in risk of diverticulosis, diverticulitis or diverticular bleeding
Diverticulitis is defined as inflammation of the diverticula caused by obstructing matter
- Infection and macroperforation. Presents with constipation. LLQ pain, fever, ↑ WBC, ↑ CRP, and may bleed
A Dutch research group created a clinical prediction rule for acute diverticulitis that includes three indicators: The presence of all three indicators had a specificity of 98% and a positive predictive value of 97%
The presence of all three of the following indicators is considered a positive result
- Absence of vomiting
- C-reactive protein level > 5 mg per dL (50 mg per L)
- Tenderness is limited to the left lower quadrant
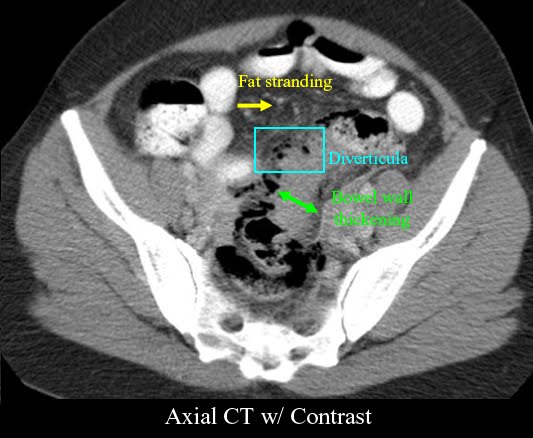
Diagnose with a CT scan with oral and intravenous (IV) contrast
- CT will demonstrate fat stranding and bowel wall thickening.
- Occult blood in the stool and mild to moderate leukocytosis may occur with diverticulitis.
- Plain-film radiography should be done to rule out free air under the diaphragm indicative of a rupture.
- DO NOT perform a colonoscopy in an acute setting, as this can perforate the colon.
The outpatient treatment of acute colonic diverticulitis typically consists of pain control and a liquid diet without antibiotics
- Clinicians may choose to use antibiotics for outpatients who may be at higher risk for poor outcomes (comorbidities, immunocompromised, or signs of systemic disturbance)
- Limit patients to a liquid diet until they can be reassessed in two to three days, after which their diet can be liberalized to soft or regular if they demonstrate clinical improvement
"Seeds, corn, and nuts – Patients with diverticular disease have historically been advised to avoid consuming seeds, corn, and nuts out of concern that undigested fragments of such food items could become lodged within a diverticulum and incite diverticulitis. However, this theory is completely unproven. Thus, we do not counsel patients with a history of diverticulitis against consuming seeds, corn, and nuts."
- Hospitalization for IV administration of antibiotics, bowel rest, and analgesics is often required. A nasogastric tube is inserted if ileus develops.
- Surgical management may be necessary in severe cases, including peritonitis, large abscesses, fistulae, or obstruction.
- Patients with diverticulosis should maintain a high-fiber diet to prevent diverticulitis. Evidence has negated the need to recommend avoidance of nuts, seeds, and popcorn.
 Osmosis Osmosis |
|
 |
A patient with diverticula, outpouchings found in the descending, sigmoid colon, is said to have diverticulosis. Diverticula are common in the older adult and may never produce symptoms or complications. However, when the outpouchings become inflamed, the condition is called diverticulitis. If left untreated, diverticulitis can lead to perforation of the intestine and can cause peritonitis. Clinical manifestations of diverticulitis include lower left-side abdominal pain, abdominal distention, flatulence, fever, rectal bleeding, and constipation or diarrhea.
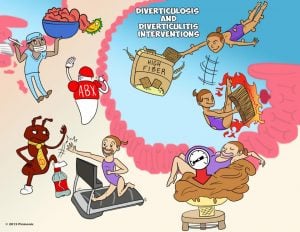
Play Video + QuizDiverticulosis and diverticulitis interventions
When a patient is diagnosed with diverticular disease, diet, and lifestyle modifications must be made to prevent recurrence and/or exacerbations of the disease. Interventions include eating a diet high in fiber, taking products to soften the stool, reducing intra-abdominal pressure, and exercising. In severe instances, bowel resection may be necessary to remove the affected portion of the intestine.
Question 1 |
Fistula Hint: See answer D for explanation | |
Colonic stricture Hint: See answer D for explanation | |
Abscess Hint: See answer D for explanation | |
Colon cancer |
Question 2 |
Celiac disease Hint: Symptoms usually occur following ingestion of gluten containing food. Also has extraintestinal manifestations. | |
Crohn disease Hint: Abdominal pain commonly occurs at the right lower quadrant or periumbilical region. Also has extraintestinal manifestations. | |
Ulcerative colitis Hint: Presents as bloody diarrhea. Also has extraintestinal manifestations. | |
Diverticulitis |
Question 3 |
Acute diverticulitis most commonly affects the ascending colon. | |
Patients with Ehlers-Danlos syndrome are disposed to development of diverticulosis. Hint: A group of inherited disorders that mostly affect the skin, joints, and blood vessels. Patients with Ehlers-Danlos syndrome are disposed to development of diverticulosis. | |
Diverticular disease is asymptomatic in 95% of cases. Hint: See A for explanation. | |
Mild attacks can be treated on an outpatient basis using oral antibiotics such as ciprofloxacin and metronidazole. Hint: See A for explanation. |
Question 4 |
Barium enema Hint: Barium enema is contraindicated during the initial stages of an acute attack because of the risk of free perforation. | |
Endoscopy Hint: Endoscopy is contraindicated during the initial stages of an acute attack because of the risk of free perforation. | |
CT scan | |
Ultrasound Hint: Ultrasound examination is often more readily available and is cheaper. It can demonstrate thickened bowel and large pericolic collections, but is less sensitive than CT. |
Question 5 |
Escherichia coli | |
Bacteroides fragilis | |
Streptococcus pneumoniae | |
a and b |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture