Patient with ulcerative colitis will present as → a 32-year-old woman comes to your office with a 6-month history of loose bowel movements, approximately eight per day. Blood has been present in many of them. She has lost 30 pounds. For the past 6 weeks, she has had intermittent fever. She has had no previous gastrointestinal (GI) problems, and there is no family history of GI problems. On examination, the patient looks ill. Her blood pressure is 130/ 70 mm Hg. Her pulse is 108 beats/ minute and regular. There is generalized abdominal tenderness with no rebound. A sigmoidoscopy reveals a friable rectal mucosa with multiple bleeding points.
Patient with Crohn's disease will present as → a 25-year-old man with an 18-month history of chronic abdominal pain. The patient has seen several physicians and has been diagnosed as having a “nervous stomach,” irritable bowel syndrome, and “depression.” Associated with this abdominal pain for the past 3 months have been nonbloody diarrhea, anorexia, and a weight loss of 20 pounds. He has developed a painful area around the anus. On examination, the patient has diffuse abdominal tenderness. He looks thin and unwell. He has a tender, erythematous area in the right perirectal area.
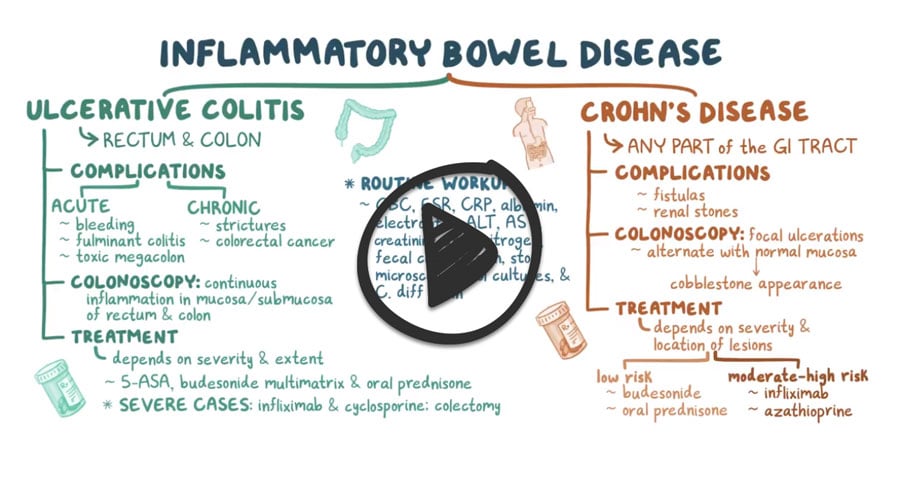
Ulcerative Colitis (“colitis” = confined to the colon)
- Presents with bloody puss-filled diarrhea, rectal/lower quadrant pain, fever, and urgency
- Inflammation isolated to the colon and confined to mucosa and submucosa (unlike Crohn's, not transmural)
- The most common site is the rectum!
- Ulcerative colitis affects the colon in an ascending fashion starting from the rectum up to the ascending colon - remember, ulcerative moves UP from the rectum to the ascending colon!
- Bimodal distribution of peak onset: age 15-25 and age 55-65
- Labs: ↑ WBC, ESR, and anemia
- Diagnosis by barium enema lead pipe appearance and colonoscopy with biopsy both show continuous ulceration starting from the rectum and extending proximally with loss of haustral markings and lumen narrowing
- Complications: Toxic megacolon, colorectal cancer
- Antibody test: Antineutrophil cytoplasmic antibodies (p-ANCA)
Crohn's Disease
- Presents with abdominal pain, weight loss, diarrhea (non-bloody), and oral mucosal aphthous ulcers. Longer-standing disease may have severe anemia, polyarthralgia, and fatigue.
- The most common site is the terminal ileum
- Distribution from mouth to anus and will commonly present with thickened bowel wall, cobblestoning, and “skip” lesions
- Linear fissures and cobblestone appearance. Tends to be transmural vs. UC is limited to the mucosa and submucosa
- Complications include strictures identified by a string sign on barium study
- Presents with abdominal pain, weight loss, diarrhea, and oral mucosal aphthous ulcers
- Obstruction, abscess, fistula, and sinus tracts are common
- 1-3% cancer risk (low)
- Antibody test: +Anti-Saccharomyces cerevisiae antibodies (ASCA)
The routine workup for inflammatory bowel diseases consists of a CBC, ESR, CRP, albumin, electrolytes, ALT, AST, creatinine, urea nitrogen, fecal calprotectin, stool microscopy, and stool cultures, along with testing for C.diff toxin.
Colonoscopy:
- In ulcerative colitis, colonoscopy shows continuous inflammation only in the mucosa and submucosa of the rectum and colon
- In Crohn’s disease, the colonoscopy shows focal ulcerations that alternate with normal mucosa, giving a cobblestone appearance
Crohn's disease
The diagnosis of Crohn's disease can sometimes be challenging, and several tests are often required to assist in making the diagnosis. Even with a full battery of tests, it may not be possible to diagnose Crohn's with complete certainty
- Rectal exam, stool exam, and culture, CBC, electrolytes, TSH, CT-abdomen
- Upper GI series with small bowel follow-through
- ⇒ ↑ ESR, anemia, nutritional and electrolyte imbalance during exacerbation
- Colonoscopy is the most valuable tool for establishing the diagnosis, determining the extent, and guiding treatment
- ⇒ colonoscopy is approximately 70% effective in diagnosing the disease, with further tests being less effective
- A biopsy will show involvement of the entire bowel wall; granulomas are frequent
- + Anti-saccharomyces cerevisiae antibodies (ASCA) and perinuclear antineutrophil cytoplasmic antibodies may distinguish Crohn's and UC
Ulcerative Colitis:
Diagnosis of ulcerative colitis typically requires colonoscopy to see the ulcers and take a biopsy
- Show continuous inflammation starting from the rectum and extending proximally with loss of haustral markings and lumen narrowing
- May elect to limit the extent of the exam (flex sigmoidoscopy) if severe colitis is encountered to minimize the risk of perforation of the colon
In addition, radiological imaging may be done with the help of a CT scan, MRI, a barium enema
- Barium enema: Lead pipe appearance (loss of haustral markings) ⇒ may cause toxic megacolon
- A radiograph may show colonic dilation
- Laboratory tests should be done to screen for anemia, decreased albumin, and electrolyte abnormalities
- Antibody test: Antineutrophil cytoplasmic antibodies (p-ANCA)
- Labs: ↑ WBC, ↑ ESR, ↑ CRP, and anemia
- Liver function tests ⇒ elevated alkaline phosphatase and γ–glutamyl transpeptidase levels in patients with major colonic involvement suggest possible primary sclerosing cholangitis
- To detect nutritional deficiencies, levels of vitamin D and B12 should be checked every 1 to 2 yr
Treatment for UC and Crohn's disease are the same
- Sulfasalazine
- This is useful if the colon is involved. 5-ASA (mesalamine) is the active compound and is released in the colon—it is more useful in UC than in Crohn's disease.
- 5-ASA compounds block prostaglandin release and serve to reduce inflammation.
- There are preparations of 5-ASA that are more useful in distal small bowel disease.
- Metronidazole—if no response to 5-ASA
- Systemic corticosteroids (prednisone/budesonide)—for acute exacerbations and if no response to metronidazole
- Immunosuppressants (azathioprine, 6-mercaptopurine)—in conjunction with steroids if the patient does not respond to the above agents
- Bile acid sequestrants (cholestyramine or colestipol)—for patients with terminal ileal disease who cannot absorb bile acids
- Antidiarrheal agents are generally not a good choice (may cause ileus)
- Nutritional supplementation and support—parenteral nutrition is sometimes necessary
- Surgical UC — is often curative (unlike Crohn's disease) and involves total colectomy.
- Surgical Crohn's (eventually required in most patients) - Involves segmental resection of involved bowel. Disease recurrence after surgery is high—up to 50% of patients experience disease recurrence at 10 years postoperatively
 Osmosis Osmosis |
|
 |
Crohn’s disease is an inflammatory bowel disorder that can involve any segment of the GI tract from the mouth to the anus but preferentially is found in the terminal ileum. The disease is characterized by periodic remissions and exacerbations.
| Crohn’s Disease Assessment | Play Video + Quiz |
| Crohn’s Symptoms and Associations | Play Video + Quiz |
| Crohn’s Disease Characteristics | Play Video + Quiz |
Ulcerative colitis
 Ulcerative colitis is characterized by severe ulcerating inflammation of the mucosal and submucosal layers that is limited to the colon and rectum. In contrast, Crohn’s disease may involve any area of the GI tract and can extend into all layers of the GI wall. Although ulcerative colitis is not considered an autoimmune disease, there are associations with autoimmunity and thought to result from a mixture of defects in host interactions with intestinal microbiota, epithelial dysfunction, and aberrant mucosal immune responses. Grossly, ulcerative colitis always involves the rectum and expands proximally in a stepwise fashion to involve all or a part of the colon. Affected areas can demonstrate broad-based ulcers and regions of regenerating mucosa can bulge into the lumen creating pseudopolyps. Histologic features include inflammatory infiltrates and crypt abscesses. Chronic inflammation can cause the colon to become thickened and stiff and can lead to shortening of the colon with atrophic mucosa and loss of haustral folds. This can give the appearance of a lead pipe in the descending and sigmoid colon when visualized with barium study. The most common symptoms include relapsing attacks of bloody diarrhea with mucous and pus and cramping lower abdominal pain. Chronic disease can lead to anorexia, weight loss, and even growth retardation.
Ulcerative colitis is characterized by severe ulcerating inflammation of the mucosal and submucosal layers that is limited to the colon and rectum. In contrast, Crohn’s disease may involve any area of the GI tract and can extend into all layers of the GI wall. Although ulcerative colitis is not considered an autoimmune disease, there are associations with autoimmunity and thought to result from a mixture of defects in host interactions with intestinal microbiota, epithelial dysfunction, and aberrant mucosal immune responses. Grossly, ulcerative colitis always involves the rectum and expands proximally in a stepwise fashion to involve all or a part of the colon. Affected areas can demonstrate broad-based ulcers and regions of regenerating mucosa can bulge into the lumen creating pseudopolyps. Histologic features include inflammatory infiltrates and crypt abscesses. Chronic inflammation can cause the colon to become thickened and stiff and can lead to shortening of the colon with atrophic mucosa and loss of haustral folds. This can give the appearance of a lead pipe in the descending and sigmoid colon when visualized with barium study. The most common symptoms include relapsing attacks of bloody diarrhea with mucous and pus and cramping lower abdominal pain. Chronic disease can lead to anorexia, weight loss, and even growth retardation.
| Ulcerative Colitis Characteristics | Play Video + Quiz |
| Ulcerative Colitis Associations | Play Video + Quiz |
Question 1 |
Prednisone Hint: Glucocorticoids are used in moderate to severe inflammatory bowel disease. | |
Sulfasalazine | |
Metronidazole Hint: Metronidazole may have a role in Crohn's disease after ileal resection but has no role in the treatment of mild to moderate disease. | |
Azathioprine (Imuran) Hint: Azathioprine is used in severe, glucocorticoid-dependent inflammatory bowel disease. |
Question 2 |
Uveitis Hint: See D for explanation | |
Erythema nodosum Hint: See D for explanation | |
Arthritis Hint: See D for explanation | |
Dermatitis herpetiformis |
Question 3 |
Ulcerative colitis is more common in non-smokers and ex-smokers. Hint: Smoking is protective in UC, with a lower incidence of disease in smokers and current smoking protects against UC and, after onset of the disease, improves its course, reducing the need for colectomy. | |
Appendectomy protects against ulcerative colitis. Hint: Appendectomy is a protective factor against UC. | |
Crohn disease causes segmental transmural inflammation of the bowel. Hint: Distribution from mouth to anus and will commonly present with thickened bowel wall, segmental transmural inflammation of the bowel, cobblestoning and “skip” lesions. | |
Ulcerative colitis affects the colon in a descending fashion. |
Question 4 |
Infliximab Hint: An anti-TNF antibodies. Suppress inflammation and induce apoptosis of inflammatory cells. | |
Budesonide Hint: Budesonide is a potent corticosteroid and has an anti-inflammatory effect. | |
Mercaptopurine Hint: Mercaptopurine is a Thiopurine. It is an immunomodulator which acts by inducing T-cell apoptosis. | |
Cisapride |
Question 5 |
Inflammation limited to the superficial layer of the bowel wall Hint: Crohn’s disease is characterized by a transmural inflammation of the GI tract. | |
The affinity to involve the rectosigmoid junction Hint: It may affect any part of the GI tract but is usually associated with the terminal ileum, the colon, or both. | |
Decreased risk of colon cancer Hint: There is also an increased risk— five times the average— for bowel cancer. | |
Continuous mucosal areas of ulceration that affect the anus Hint: This is the description of ulcerative colitis | |
Fistula formation |
|
List |
References: Merck Manual · UpToDate