Patient will present as → a 40-year-old woman who comes to your office with a several-year history of lower abdominal pain associated with constipation (one hard bowel movement every 3 days) and frequent mucous discharge. She states that her abdominal pain is better after a bowel movement. She has never passed blood per rectum. She describes no fever, chills, weight loss or gain, jaundice, or any other symptoms. There is no relationship between the abdominal pain and specific food intake. On physical examination, the abdomen is scaphoid, and no hepatosplenomegaly or masses are palpated. There is a mild generalized abdominal tenderness, but it does not localize.
The Rome criteria are standardized symptom-based criteria for diagnosing IBS
The Rome criteria require the presence of abdominal pain or discomfort for at least 3 days/mo in the last 3 mo along with ≥ 2 of the following:
- Improvement with defecation
- Onset (of each episode of discomfort) associated with a change in frequency of defecation
- Change in consistency of stool
IBS subtypes are defined for clinical practice as follows:
- IBS with predominant constipation: Patient reports that abnormal bowel movements are usually constipation
- IBS with diarrhea: Patient reports that abnormal bowel movements are usually diarrhea
- Mixed IBS: Patient reports that abnormal bowel movements are usually both constipation and diarrhea (more than one-fourth of all the abnormal bowel movements were constipation and more than one-fourth were diarrhea)
- Unclassified IBS: Patients who meet diagnostic criteria for IBS but cannot be accurately categorized into one of the other three subtypes
The cause is unknown, and the pathophysiology is incompletely understood
- Bloating and N/V are common
- Pain often relieved by defecation
- BM's are irregular and vary from constipation to diarrhea
The diagnosis of IBS can reasonably be made using the Rome criteria as long as patients have no red flag findings, such as rectal bleeding, weight loss, and fever, or other findings that might suggest another etiology.
- Patients with one of these red flag findings require further imaging studies and/or colonoscopy
- Routine laboratory studies (complete blood count, chemistries) are normal in IBS
Treatment is symptomatic, consisting of dietary management and drugs, including anticholinergics and agents active at serotonin receptors.
- Increased fiber, decrease dietary fat, drug therapy
- Drug therapy is directed toward the dominant symptoms. Anticholinergic drugs (eg, hyoscyamine 0.125 mg po 30 to 60 min before meals) may be used for their antispasmodic effects.
 Osmosis Osmosis |
|
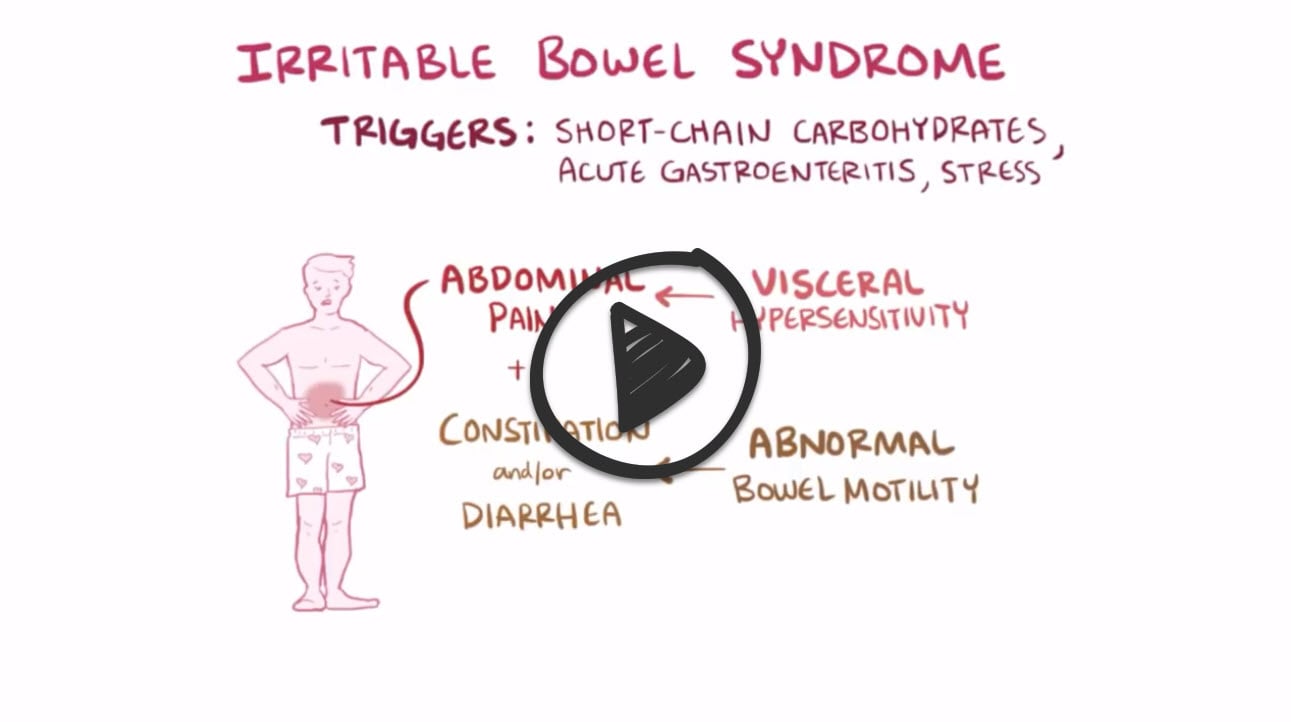 |
Irritable bowel syndrome (IBS) is characterized as a chronic gastrointestinal disorder that includes symptoms of abdominal pain, alterations in bowel patterns, excessive flatulence, and fatigue. However, these symptoms are widely individualized, which makes IBS difficult to diagnose. Symptoms may be exacerbated by psychosocial stressors and certain foods. This condition is more commonly diagnosed in women. Although there is no specific test to identify IBS, diagnostic tests for other health conditions are performed to rule them out.
Play Video + QuizIrritable Bowel Syndrome (IBS) Interventions
The goal of IBS treatment includes decreasing symptoms by increasing dietary fiber and administering medications such as anticholinergics, loperamide, tricyclic antidepressants, and linaclotide. Medications specific to women include lubiprostone, tegaserod, and alosetron. Identifying and reducing risk factors that exacerbate IBS is critical to help avoid exacerbations of the condition.
Question 1 |
Steroid enemas Hint: See C for explanation | |
Mesalamine enemas Hint: See C for explanation | |
Peppermint oil | |
Metoclopramide Hint: See C for explanation | |
None of the above |
Question 2 |
It is a diagnosis of exclusion Hint: See B for explanation | |
It is an organic disorder | |
Young women are affected 2–3 times more often than men Hint: See B for explanation | |
May occur following an episode of gastroenteritis Hint: See B for explanation |
Question 3 |
Irritable bowel syndrome | |
Lactase deficiency Hint: Presents as diarrhea and flatulence following ingestion of milk. | |
Ulcerative colitis Hint: Presents as bloody diarrhea | |
Crohn disease Hint: Physical examination would reveal a mass at the right lower quadrant. |
Question 4 |
Colonoscopy Hint: See D for explanation | |
Barium enema Hint: See D for explanation | |
Abdominal radiograph Hint: See D for explanation | |
None of the above |
Question 5 |
Alvarado score Hint: Is used in making a diagnosis of acute appendicitis. | |
Ranson criteria Hint: Is used in assessing the severity of acute pancreatitis. | |
Rome criteria | |
Revised Jones criteria Hint: Is used in diagnosing rheumatic fever. |
Question 6 |
Giardia lamblia | |
Escherichia coli | |
Shigella | |
Salmonella |
Question 7 |
Painless diarrhea | |
Fever | |
Postprandial urgency | |
Steatorrhea |
Question 8 |
Altered stool frequency | |
Mucorrhea | |
Abdominal bloating or subjective distention | |
Frequent nausea |
Question 9 |
Iron deficiency anemia | |
Abdominal pain | |
Amenorrhea | |
Hypokalemia |
|
List |
References: Merck Manual · UpToDate




