Patient will present as → a 71-year-old male with a history of atrial fibrillation with a sudden onset of severe abdominal pain occurring 10 minutes after eating. Physical exam findings are relatively benign, and the patient has only minimal pain with palpation of the abdomen. Stool guaiac is positive, and blood tests reveal leukocytosis with an elevated lactate, amylase, and LDH.
Ischemic bowel disease occurs when an artery that supplies blood becomes blocked or narrowed. This can affect the small bowel or the large bowl.
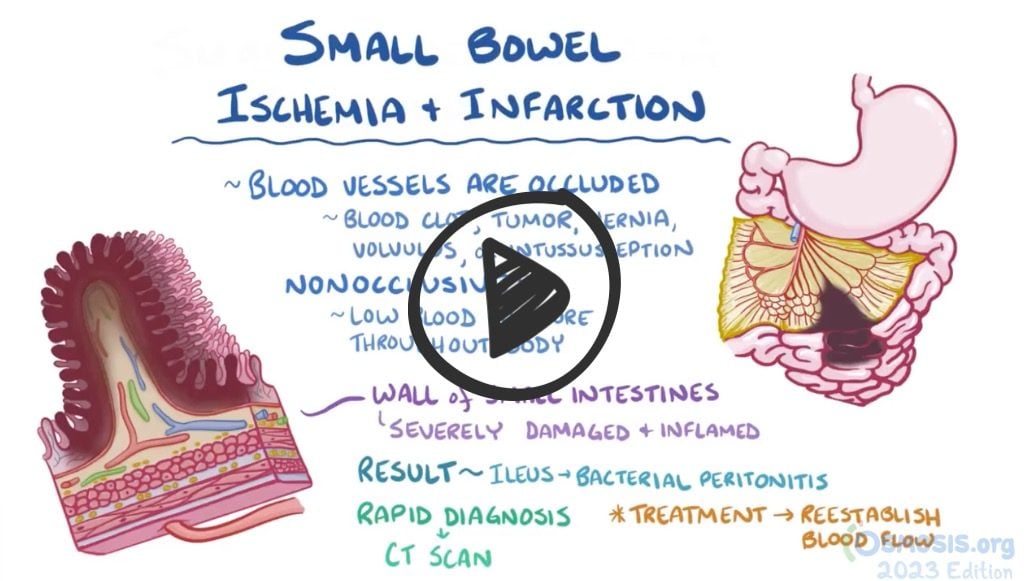
- There are several possible causes of ischemic bowel disease, including blockage in the arteries due to a tumor or blood clot, narrowing of the arteries supplying blood to the bowel from atherosclerosis, hernia, volvulus, and intussusception. It can also occur due to a nonocclusive event like low blood pressure throughout the body (shock).
Types of intestinal ischemia
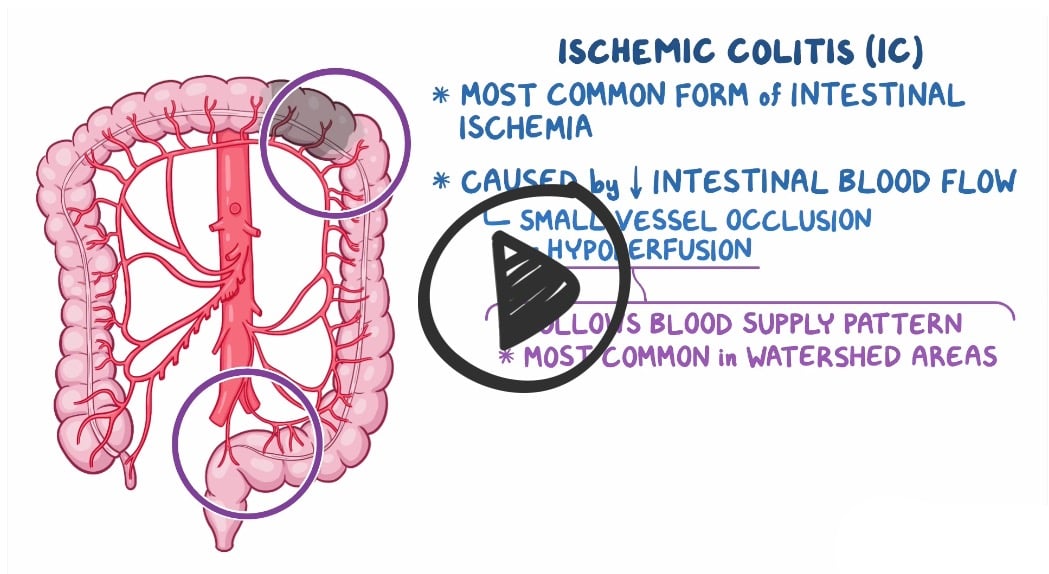
- Ischemic colitis (ischemia of the colon): hypoperfusion of the large bowel
- Acute mesenteric ischemia: acute loss of blood flow to the small intestine
- Chronic mesenteric ischemia: constant or episodic hypoperfusion of the small intestine
Ischemic colitis (ischemia of the colon)
|
Acute mesenteric ischemia (ischemia of the small intestine)
|
Chronic mesenteric ischemia (ischemia of the small intestine)
|
Diagnosis is made by CT or colonoscopy, angiography, or magnetic resonance angiography
- Mesenteric angiography is considered the (gold standard)
- Abdominal X-ray shows “thumb-printing” of small bowel or right colon due to submucosal bleeding
Treatment for both acute and chronic mesenteric ischemia is revascularization
 Osmosis Osmosis |
|
 |
|
 |
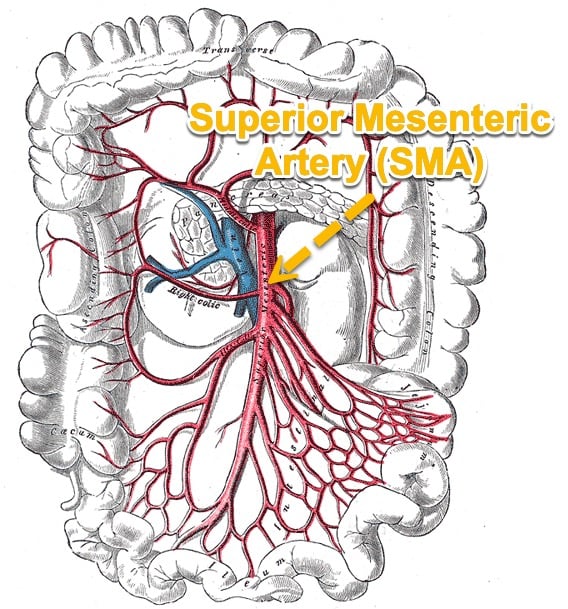
Mesenteric ischemia is a condition caused by insufficient blood flow to the small intestine. Poor blood flow is caused by thrombotic or embolic occlusion of the arteries that feed the small intestine, most commonly the proximal superior mesenteric artery (SMA). This lack of perfusion causes bowel ischemia, and subsequent necrosis if left untreated. Hallmark findings are severe abdominal pain that is out of proportion to their physical examination, nausea, vomiting, and bloody stools. Laboratory testing shows metabolic acidosis with elevated lactate, and abdominal x-ray and CT angiography may show bowel wall thickening or edema, signs of obstruction, or air within the bowel wall. Treatment includes fluids, broad spectrum antibiotics, anticoagulation, and emergent surgical exploration in severe cases.
Play Video + QuizQuestion 1 |
Crohn disease Hint: See C for explanation | |
Ulcerative colitis Hint: See C for explanation | |
Appendicitis | |
Ischemic colitis Hint: See C for explanation |
Question 2 |
Acute mesenteric ischemia | |
Diverticulitis Hint: Physical examination would reveal a palpable mass at the left lower quadrant of the abdomen. | |
Ulcerative colitis Hint: Symptoms onset is typically insidious. There are also extraintestinal manifestations. Abdominal pain doesn’t typically occur following feeding. Cardiac disease is not a risk factor. | |
Crohn disease Hint: Abdominal pain doesn’t typically occur following feeding. There are extraintestinal manifestations, and a mass may be felt at the right lower quadrant. |
Question 3 |
Acute mesenteric ischemia Hint: presents as sudden onset abdominal pain with rectal bleeding. Presentation is usually acute. | |
Peptic ulcer disease Hint: Presents as periodic epigastric pain. Pain may be made worse by certain types of food. | |
Chronic mesenteric ischemia | |
Gastric cancer Hint: Epigastric pain is not associated with feeding |
Question 4 |
Papaverine Hint: Intra-arterial infusion of papaverine through the angiography catheter at the affected vessel is useful for all arterial forms of AMI. | |
Urokinase Hint: A thrombolytic, infused through the angiography catheter can be live saving for selected patient with acute mesenteric arterial embolism. | |
Heparin Hint: Heparin anticoagulation is the main therapy for mesenteric venous thrombosis. | |
Prednisolone |
Question 5 |
Angioplasty with stenting Hint: See D for explanation | |
Angioplasty without stenting Hint: See D for explanation | |
Revascularization Hint: See D for explanation | |
All of the above are appropriate surgical management options |
|
List |
References: Merck Manual · UpToDate