| Thyroid test | What it measures | Normal range | Associated thyroid condition(s) | How levels are affected |
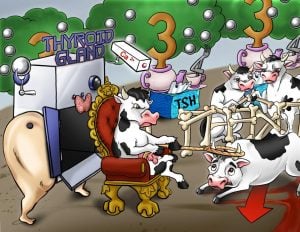
| Thyroid-stimulating hormone (TSH) | The amount of TSH in the blood | 0.3-4.0 mIU/L | Hypothyroidism, hyperthyroidism | High TSH levels indicate hypothyroidism, while low TSH levels indicate hyperthyroidism. |
| Free thyroxine (T4) | The amount of free T4 in the blood | 0.8-1.8 ng/dL | Hypothyroidism, hyperthyroidism | Low T4 levels indicate hypothyroidism, while high T4 levels indicate hyperthyroidism. |
| Free triiodothyronine (T3) | The amount of free T3 in the blood | 2.3-4.2 pg/mL | Hypothyroidism, hyperthyroidism | Low T3 levels indicate hypothyroidism, while high T3 levels indicate hyperthyroidism. |
| Thyroid peroxidase antibodies (TPOAb) | The presence of antibodies to thyroid peroxidase | <1.0 IU/mL | Hashimoto's thyroiditis, Graves' disease | High TPOAb levels can be present in people with Hashimoto's thyroiditis and Graves' disease. |
| Thyroglobulin antibodies (TgAb) | The presence of antibodies to thyroglobulin | <0.4 kIU/L | Hashimoto's thyroiditis, Graves' disease | High TgAb levels can be present in people with Hashimoto's thyroiditis and Graves' disease. |
| Thyroglobulin (Tg) | The amount of Tg in the blood | 3-40 ng/mL | Thyroid cancer | High Tg levels may be present in people with thyroid cancer. |
| Anti-thyrotropin antibodies (TSHR-Ab) | The presence of antibodies to the thyrotropin receptor | Negative | Graves' disease | High TSHR-Ab levels are present in people with Graves' disease. |
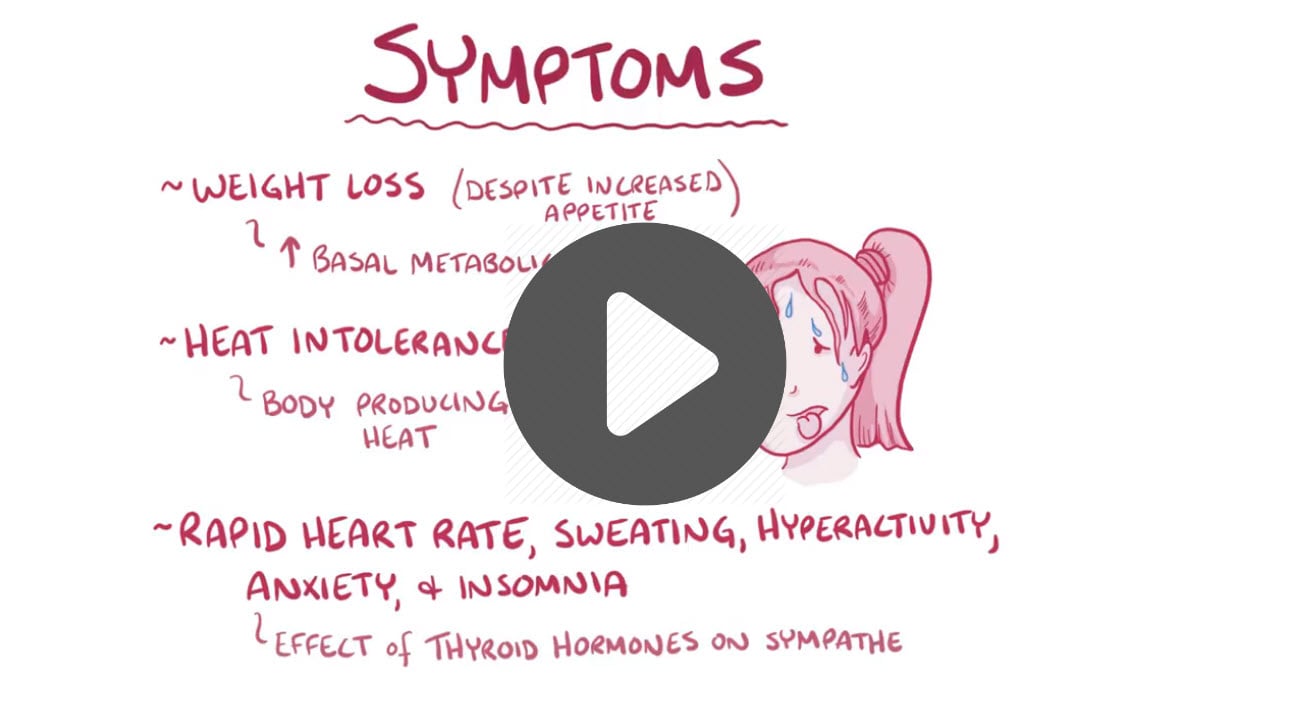
ReelDx Virtual Rounds (Hyperthyroidism)
Hyperthyroidism is the production of too much thyroxine hormone. It can increase metabolism and accelerate the body's metabolism, causing unintentional weight loss and a rapid or irregular heartbeat
Etiology: Grave’s disease (autoimmune). Toxic adenoma, thyroiditis, pregnancy, amiodarone
Presentation: Heat intolerance, palpitations, sweating, weight loss, tremor, anxiety, tachycardia
- Graves - Diffuse goiter with a bruit, exophthalmos, pretibial myxedema
- Thyroid storm - Fever, tachycardia, delirium
Diagnosis:
- TSH (best test): Decreased in primary disease (↓ TSH and ↑ Free T4), elevated in secondary disease (↑ TSH and ↑ Free T4)
- T4 ⇒ elevated although may be normal
- Thyroid radioactive iodine uptake:
- Graves: diffusely high uptake
- Toxic multinodular: discrete areas of high uptake
Antibodies:
- Graves: Anti-thyrotropin antibodies (TSHR-Ab) - can be measured by either a TSI or TBII
- Other antithyroid antibodies, such as antithyroid peroxidase (anti-TPO) and antithyroglobulin (anti-Tg) antibodies are also present in Graves disease but ⇒ levels tend to be even more elevated in autoimmune thyroiditis.
Treatment:
- Beta-blockers (symptomatic), methimazole/propylthiouracil, radioactive iodine, thyroidectomy
- Thyroid storm- prompt beta-blockers, hydrocortisone, methimazole/propylthiouracil, iodine
- Thyroidectomy- most likely complication is an injury to the recurrent laryngeal nerve (hoarseness)
Antithyroid drugs during pregnancy — Propylthiouracil used to be the drug of choice during pregnancy because it causes less severe birth defects than methimazole. But experts now recommend that propylthiouracil be given during the first trimester only. This is because there have been rare cases of liver damage in people taking propylthiouracil. After the first trimester, women should switch to methimazole for the rest of the pregnancy.
- For women who are nursing, methimazole is probably a better choice than propylthiouracil (to avoid liver side effects)
Etiology: Hashimoto’s (chronic lymphocytic/autoimmune), previous thyroidectomy/iodine ablation, congenital
Presentation:
- Cold intolerance, fatigue, constipation, depression, weight gain, bradycardia
- Congenital: round face, large tongue, hernia, delayed milestones, poor feeding
Diagnosis:
Labs: TSH- elevated in primary disease. Low T4 (↑ TSH and ↓ Free T4)
- Hashimoto’s: antibodies to thyroid peroxidase (anti-TPO autoantibodies) and antithyroglobulin antibodies (anti-Tg)
Treatment: Levothyroxine. Follow up with serial TSH monitoring
Thyroiditis is a general term that refers to “inflammation of the thyroid gland”. Thyroiditis includes a group of individual disorders causing thyroidal inflammation but presenting in different ways.
- Painful vs. Painless may be hypo or hyperthyroid
Hashimoto’s thyroiditis:
- Diffusely enlarged, painless, nodular goiter
Subacute thyroiditis (Quervain's thyroiditis):
- Young women, after a viral infection
- Painful enlarged thyroid with dysphagia, mild fever, neck pain
- DX: ↑ T4 and T3 and ↓ TSH concentrations. ↑ ESR, ↑ CRP. Radioiodine or technetium imaging study will show low uptake
- TX: Aspirin or NSAIDs, propranolol
- Thyroid function tests should be monitored every two to eight weeks to confirm the resolution of hyperthyroidism, detection of hypothyroidism, and subsequent normalization of function
Postpartum thyroiditis:
- 1-2 months of hyperthyroidism after delivery
- TX: Completely resolves, give propranolol for cardiac symptoms
Drug-induced: Thyroiditis can also be seen in patients taking certain drugs
- Antithyroid medications: methimazole and propylthiouracil
- Lithium - bipolar disorder
- Amiodarone - antiarrhythmic
- Interferon alpha
- Tyrosine Kinase Inhibitors (e.g. Sunitinib) - anti-cancer
- Checkpoint inhibitors (e.g. Nivolumab, Pembrolizumab)
- DX: TSH should be checked every 6-12 months
- TX: T4 therapy given right away
Infectious (suppurative) bacterial thyroiditis (rare) is often due to the hematogenous spread of staph or strep
- Its signs are the classic ones of inflammation: fever, heat, pain, redness, and swelling
- DX: ↑ WBC
- TX: Antibiotic/surgical drainage
Summary of thyroiditis:
| Type | Cause | Features | Diagnosis | Duration and resolution |
| Hashimoto’s thyroiditis | Anti-thyroid antibodies, autoimmune disease | Hypothyroidism, rare cases of transient thyrotoxicosis | Thyroid function tests, thyroid antibody tests | Hypothyroidism is usually permanent |
| Subacute thyroiditis (de Quervain’s thyroiditis) | Possible viral cause | Painful thyroid, thyrotoxicosis followed by hypothyroidism | Thyroid function tests, sedimentation rate, radioactive iodine uptake | Resolves to normal thyroid function within 12-18 months, 5% possibility of permanent hypothyroidism. |
| Silent thyroiditis, Painless thyroiditis | Anti-thyroid antibodies, autoimmune disease | Thyrotoxicosis followed by hypothyroidism. | Thyroid function tests, thyroid antibody tests, radioactive iodine uptake | Resolves to normal thyroid function within 12-18 months, 20% possibility of permanent hypothyroidism. |
| Postpartum thyroiditis | Anti-thyroid antibodies, autoimmune disease | Thyrotoxicosis followed by hypothyroidism | Thyroid function tests, thyroid antibody tests, radioactive iodine uptake (contraindicated if the hypothyroid woman is breastfeeding) | Resolves to normal thyroid function within 12-18 months, 20% possibility of permanent hypothyroidism |
| Drug-induced | Drugs include amiodarone, lithium, interferons, cytokines | Either thyrotoxicosis or hypothyroidism. | Thyroid function tests, thyroid antibody tests | Often continues as long as the drug is taken |
| Radiation-induced | Follows treatment with radioactive iodine for hyperthyroidism or external beam radiation therapy for certain cancers. | Occasionally thyrotoxicosis, more frequently hypothyroidism | Thyroid function tests | Thyrotoxicosis is transient, hypothyroidism is usually permanent |
| Acute thyroiditis, Suppurative thyroiditis | Bacteria mainly, but any infectious organism | Occasionally painful thyroid, generalized illness, occasional mild hypothyroidism | Thyroid function tests, radioactive iodine uptake, fine-needle aspiration biopsy | Resolves after treatment of infectious cause, may cause severe illness |
 Osmosis Osmosis |
|
 |
The thyroid gland is a large endocrine gland that is located in the neck. It releases T3 and T4 hormones, which help the body regulate metabolism. T3 and T4 stand for triiodothyronine (T3) and thyroxine, which can sometimes be referred to as tetraiodothyronine (T4). In addition, the thyroid gland has a blood calcium sensor that helps it detect when blood calcium levels are elevated, to which it responds. The thyroid gland releases calcitonin, which builds bone, resulting in an absorption of calcium from the bloodstream. Osteoblasts are the cells responsible for bone formation.
Play Video + QuizThyroid Function Screening Tests

When a patient is suspected of having an underlying thyroid condition, there is a stepwise approach to ordering thyroid function tests. The initial screening test of choice is the measurement of thyroid stimulating hormone or TSH. Depending on the value determined, measurements of thyroid hormones (serum free T3 and free T4) may be taken, with the addition of a total T4 measurement to provide further evidence towards the underlying cause. Regardless of etiology, screening tests are not always reliable in a severely ill inpatient population, and special circumstances, like pregnancy, may alter the measured value of these tests.




