Patellar soft tissue injuries
Prepatellar Bursitis (Housemaid's Knee)Patient will present as → a 40-year-old female who comes to the clinic with a complaint of swelling and pain at the front of her left knee. She reports that the symptoms began a few days ago and have progressively worsened. She recalls kneeling for an extended period while gardening over the weekend. She denies any recent trauma, fever, or other joint issues. On physical examination, there is pronounced, tender swelling over the prepatellar area without overlying redness or warmth. The range of motion is intact, but pain is elicited with direct pressure over the swollen area. There is no evidence of joint instability, and ligamentous examination is unremarkable. Aspiration of the bursa yields a clear, viscous fluid, and subsequent analysis shows no crystals or signs of infection. The patient is diagnosed with prepatellar bursitis and is advised to avoid prolonged kneeling, use knee pads for protection, and consider taking NSAIDs for pain relief. She is also educated about the importance of ice application and given an option for a compressive wrap to reduce swelling. |
|
|
Prepatellar bursitis is an inflammation of the bursa in the front of the kneecap (patella)
DX: Concern for septic bursitis in wrestlers - aspiration with gram stain and culture
TX: compressive wrap, NSAIDs, +/- aspiration, and immobilization for 1 week. Corticosteroid use is controversial
 Prepatellar bursitis, with a reference knee in the background. Caused by a sports injury, fluid was removed in an attempt to treat it, but the bursa was ultimately excised. References: Merck Manual · UpToDate |
|
Picmonic Prepatellar bursitis is an inflammation of the prepatellar bursa in front of the kneecap that can be caused by repeated trauma on the flexed knee (e.g., sports injuries, pressure from excessive kneeling). It is also known as Housemaid’s knee. Manifestations include pain and erythema. A minority of the cases can be complicated by septic bursitis from staphylococcus aureus. Aspiration can be done in patients with acute bursitis to rule out infectious causes of gout. NSAIDs are used to manage symptoms, and antibiotics should be added if an infectious etiology is suspected. Play Video + Quiz |
|
Patellar TendinitisPatient will present as → a 30-year-old male who comes to the office complaining of a sharp pain just below the kneecap that started after his regular weekend basketball games. He mentions the pain worsens when jumping or running and has been progressively getting more severe over the past month. He works as a physical education teacher and is very active throughout the week. On physical examination, there is tenderness to palpation at the patellar tendon insertion on the tibial tuberosity. The patient exhibits pain when resisting knee extension and during a squatting maneuver. There is no significant swelling or erythema, and the range of motion of the knee is intact. An ultrasound of the knee shows thickening of the patellar tendon and hypoechoic areas, indicating tendinopathy. Based on the clinical findings, a diagnosis of patellar tendinitis, also known as jumper’s knee, is made. Treatment recommendations include rest, ice, compression, and elevation (RICE), nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management, and a referral to physical therapy for eccentric strengthening exercises. The patient is also advised on the gradual resumption of sports activities and the use of a patellar tendon strap during activities that may aggravate the condition. |
|
An injury to the tissue connecting the kneecap to the shin bone (patellar tendon)
DX: History and physical examination are usually sufficient for diagnosis of infrapatellar tendinitis; however, MRI can show the extent of the injury.
TX: Ice, rest, activity modification, followed by physical therapy. Surgical excision and suture repair as needed
References: Merck Manual · UpToDate |
|
Patellofemoral Pain (PFP)Patient will present as → a 20-year-old female college student and recreational runner who reports experiencing a dull, aching pain around her kneecap that has been worsening over the past 3 months. She describes the pain as being particularly noticeable when she is climbing stairs, squatting, and sitting with her knees bent for prolonged periods during her lectures. She denies any specific injury but notes that the pain began when she increased her running mileage. Her medical history is unremarkable. On physical examination, there is pain on palpation of the patellar borders and slight swelling of the anterior knee. There is also a positive patellar compression test. Strength testing reveals mild quadriceps muscle weakness, and flexibility tests show tightness in her hamstrings and iliotibial band. No signs of instability or effusion are present. Conservative treatment is initiated with activity modification, quadriceps-strengthening exercises, hamstring and iliotibial band stretching, and instructions on proper footwear. The patient is advised to avoid activities that exacerbate symptoms and to gradually return to running, following a program that includes a proper warm-up and cool-down routine. |
|
Patellofemoral joint pain can be defined as anterior knee pain involving the patella and retinaculum that excludes other intraarticular and peripatellar pathology
"The term chondromalacia patella is used to describe pathologic changes in the articular cartilage of the patella, such as softening, erosion, and fragmentation. While frequently confused with PFP, chondromalacia patella is a pathologic diagnosis and constitutes a distinct cause of knee pain. - UpToDate" DX: Although PFP is a clinical diagnosis, the diagnosis can be supported by the patellofemoral compression test (reproduction of the pain with compression of the patella during knee extension) TX: Treatment is usually conservative with the use of physical therapy, weight loss, NSAIDs, and support braces 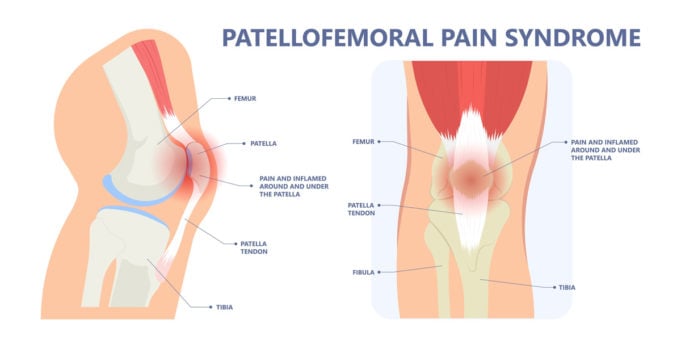 © Pepermpron by Adobe Stock References: Merck Manual · UpToDate |
|
Picmonic Patellofemoral Pain Syndrome
Patellofemoral Pain Syndrome, or PFPS, is an overuse injury of the knee, commonly seen in young athletic women. Pain in this syndrome is primarily poorly localized anterior knee pain, that worsens with squatting, running, prolonged sitting, and climbing stairs. Although PFPS is a clinical diagnosis, the diagnosis can be supported by the patellofemoral compression test and the apprehension sign. Treatment is usually conservative with the use of physical therapy, weight loss, NSAIDs, and support braces. Play Video + Quiz |
Ligament/Meniscal injuries
|
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now. |
|||||||||
Anterior Cruciate Ligament (ACL) TearPatient will present as → a 22-year-old female soccer player who reports a “popping” sensation in her knee followed by immediate swelling after pivoting awkwardly during a game yesterday. She states that her knee “gave out,” and she was unable to continue playing. She has experienced significant pain and has had difficulty bearing weight on the affected leg. She denies any previous knee problems. Medical history is unremarkable. On physical examination, her knee is swollen and warm to the touch, with a noticeable effusion. A Lachman test shows a significant increase in anterior translation of the tibia when compared to the unaffected leg, and the pivot-shift test elicits a feeling of instability and is positive. Magnetic resonance imaging (MRI) of the knee confirms a complete tear of the anterior cruciate ligament. The patient is referred to an orthopedic surgeon for evaluation of surgical options and is advised on the importance of pre-surgical physical therapy to reduce swelling and improve the range of motion. |
|||||||||
An ACL tear is a common sports injury that occurs when the anterior cruciate ligament (ACL) in the knee is torn. The ACL is one of four ligaments that connect the thighbone (femur) to the shinbone (tibia) and helps stabilize the knee joint. ACL tears are often caused by sudden changes in direction, pivoting, or landing from a jump
Testing:
**Segond fracture is an avulsion fracture of the knee that involves the lateral aspect of the tibial plateau and is frequently (~75% of cases) associated with ACL tears DX: Magnetic resonance imaging (MRI) can confirm the diagnosis
(watch a video of the ACL exam) 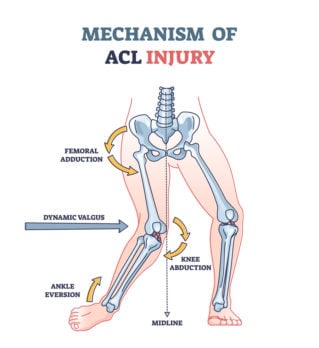 ACL tears are often caused by the combination of knee abduction, ankle eversion, and femoral adduction (image © VectorMine by Adobe Stock) References: Merck Manual · UpToDate |
|||||||||
A 33-year-old male presents to your office with a complaint of right knee injury associated with pain and swelling. He states he was running after his loose dog and suddenly stopped, hyperextended his knee, heard a pop and noticed immediate swelling. On physical examination, the Lachman test and anterior drawer test demonstrates joint laxity. Which of the following ligaments is most likely injured?
Question 1 Explanation: Anterior cruciate ligament injuries occur with sudden deceleration injuries. Patients often hear a pop and the diagnosis is aided by assessing the anterior drawer test and Lachman test. The immediate swelling as well as laxity with anterior drawer test and Lachman test should raise suspicion of anterior cruciate ligament injury.
There is 1 question to complete.
|
|||||||||
Picmonic Anterior cruciate ligament (ACL) tear
The ACL stabilizes the knee by resisting hyperextension and anterior dislocation of the tibia during flexion. Injuries typically occur during non-contact sports such as basketball and soccer, but can also occur from trauma. Play Video + Quiz |
Medial Collateral Ligament (MCL) TearPatient will present as → a 26-year-old college football player who is brought to the emergency department after being hit on the lateral side of the left knee. He reports hearing a pop, and then his knee buckled. He is now in severe pain and is having difficulty walking. On examination, there is swelling over the medial aspect of the left knee. There is laxity when a valgus stress test is performed on the knee. The results of the Lachman and McMurray tests are negative. You order an MRI of the knee with results seen here. |
|
The MCL is a thick band of tissue that runs along the inner side of the knee and stabilizes the joint. MCL tears are common in sports that involve contact or sudden changes in direction, such as football, basketball, and soccer. They can also occur from a fall or other direct blow to the outside of the knee
DX: MRI definitive study TX: Conservative treatment with bracing and physical therapy is typically effective
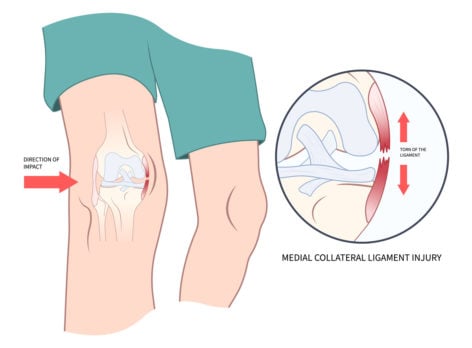 MCL tears are common in sports (such as football) as a result of a direct blow to the outside of the knee (image © Pepermpron by Adobe Stock) References: Merck Manual · UpToDate |
|
Picmonic Medial collateral ligament (MCL) tear
A medial collateral ligament (MCL) tear is an injury of the ligament that connects the femur to the tibia on the medial aspect of the knee. It occurs in patients that have experienced high-energy trauma. It is typically treated conservatively and can be clinically observed with the valgus stress test.
Play Video + Quiz
|
Lateral Collateral Ligament (LCL) TearPatient will present as → a 25-year-old soccer player who injures his knee after colliding with an opposing player during a game. On physical exam, his Lachman is weakly positive. He has laxity to varus stress with the knee flexed to 30 degrees. Dial test of the tibia shows increased external rotation at 30 degrees but not at 90 degrees in comparison to the contralateral leg. |
|
The lateral collateral ligament (LCL) is a strong band of tissue that connects the thighbone (femur) to the fibula, one of the two bones in the lower leg. An LCL tear is a common injury, especially among athletes who participate in sports that involve cutting, pivoting, or contact.
DX: Radiographs - AP, lateral, and varus stress radiographs
TX: Conservative treatment with bracing and therapy is typically effective
 Image of MRI showing lateral collateral ligament (LCL) rupture at the fibula head (arrowheads) and substance of the LCL (arrows) by Takeshi Oshima et al. License: CC BY 3.0 References: Merck Manual · UpToDate |
Posterior Cruciate Ligament (PCL) TearPatient will present as → a 22-year-old recreational soccer player who sustained a right knee injury 6 months ago. He has been treated with rest and rehabilitation but is unable to play at his previous level due to his knee “giving way.” Physical exam reveals 10° varus alignment when standing and a varus thrust with walking. Strength is full compared to the other side. Ligamentous exam reveals a stable ACL and MCL but opens to a varus stress and a 3+ posterior drawer and positive dial test at both 30° and 90° degrees of flexion. |
|
The posterior cruciate ligament (PCL) is located at the back of the knee and helps to prevent the shinbone from moving backward too far
DX: MRI is the confirmatory study for the diagnosis of PCL injury TX: Protected weight bearing and rehab indicated for isolated Grade I (partial) and II (complete isolated) injuries
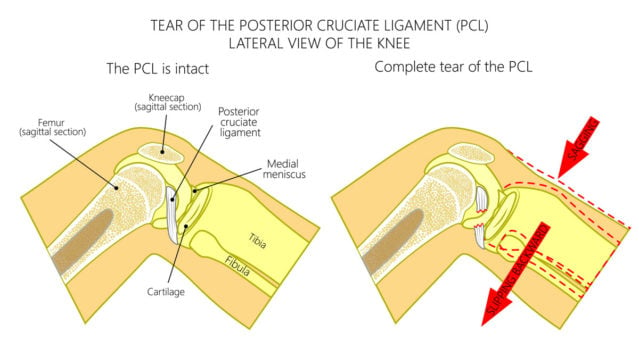 PCL injuries can also result from a blow to the knee while it is flexed or bent (image © Aksana by Adobe Stock)
References: Merck Manual · UpToDate |
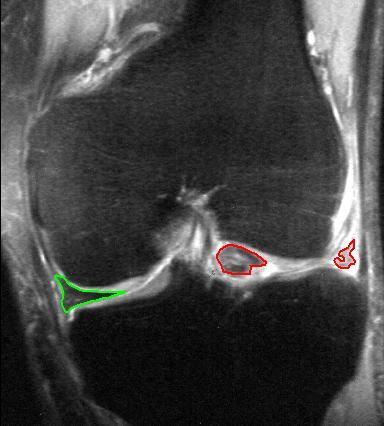
Meniscal TearPatient will present as → a 30-year-old male who reports knee pain and locking after twisting his knee while playing basketball a week ago. He mentions that the pain is localized to the medial side of the knee and has been persistent since the injury. The patient also experiences locking and discomfort when squatting. Medical history includes mild osteoarthritis. On physical examination, there is tenderness along the joint line, and McMurray’s test reproduces pain and a clicking sensation. The Apley grind test is also positive for reproducing pain and a sense of roughness on rotation of the foot with applied axial pressure. An MRI of the knee reveals a horizontal cleavage tear of the medial meniscus. Conservative management, including rest, ice, compression, and elevation (RICE) is initially recommended along with nonsteroidal anti-inflammatory drugs (NSAIDs). The patient is referred to physical therapy for exercises to strengthen the quadriceps and hamstrings. An orthopedic consultation is advised for possible arthroscopic evaluation and repair due to the mechanical symptoms. |
|
The meniscus is a C-shaped piece of cartilage that acts as a shock absorber between the shinbone and thighbone. Meniscal tears are most commonly caused by twisting the knee while playing sports or landing awkwardly on the knee after a fall
"MCL tears are often part of the "terrible triad," which includes an anterior cruciate ligament tear, medial collateral ligament tear, and meniscus tear" Testing
DX: Radiographs of the knee, possibly including sunrise, tunnel, posteroanterior, weight-bearing anteroposterior, and lateral views
TX: If the tear is not serious, physical therapy, compression, elevation, and icing of the knee can heal the meniscus
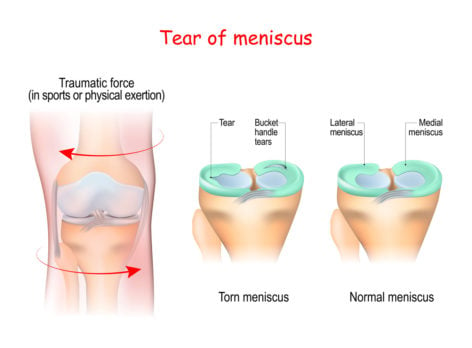 Meniscal tears are most commonly caused by twisting the knee while playing sports or landing awkwardly on the knee after a fall. (image © designua by Adobe Stock) References: Merck Manual · UpToDate |
|
Picmonic Meniscal Tear
The menisci are fibrocartilage semicircular bands that serve to stabilize the knee and absorb forces between the distal femoral condyles and the proximal tibial plateau of the knee. Injury can be sustained from trauma or in a degenerative manner. Symptoms include locking and clicking, as well as a positive McMurray test. Meniscus tears are typically managed conservatively, or in serious cases, surgery. Play Video + Quiz |