To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Patient will present as → a 37-year-old male complaining of rapid onset of severe mid-epigastric pain with radiation to the back after eating a large meal. The pain typically lessens when the patient leans forward or lies in the fetal position. Physical exam shows low-grade fever, epigastric tenderness, diminished bowel sounds, and bruising of the flanks. An abdominal CT scan shows localized dilation of the upper duodenum and a small collection of fluid in the left pleural cavity.
Acute Pancreatitis - epigastric abdominal pain with radiation to the back and elevated lipase - pain decreases when the patient leans forward
- It has many causes, including gallstones and chronic, heavy alcohol use
- The mnemonic GET SMASHHED is useful in recalling the most common causes:
- Gallstones, Ethanol, Trauma, Steroids, Mumps, Autoimmune disease, Scorpion sting, Hypercalcemia, Hyperlipidemia, ERCP and Drugs
- The mnemonic GET SMASHHED is useful in recalling the most common causes:
- Cullen's sign (bruising near the umbilicus) is superficial edema and bruising in the subcutaneous fatty tissue around the umbilicus.
- Grey Turner's sign (flank bruising) refers to bruising of the flanks, the part of the body between the last rib and the top of the hip
Ranson’s criteria for poor prognosis
Ranson's criteria: The Ranson criteria form a clinical prediction rule for predicting the severity of acute pancreatitis. Three or more means a more severe course:
At admit:
- Age > 55
- Leukocyte: >16,000
- Glucose: >200
- LDH: >350
- AST: >250
At 48 hrs:
- Arterial PO2: <60
- HCO3: <20
- Calcium: <8.0
- BUN: Increase by 1.8+
- Hematocrit: decrease by >10%
- Fluid sequestration >6L
Chronic Pancreatitis
Clinical features are the same as those of acute pancreatitis, with the addition of fat malabsorption and steatorrhea late in the disease. Fecal fat will be elevated if malabsorption is present.
The classic triad (look for this on your exam) of pancreatic calcification, steatorrhea, and diabetes mellitus occurs in only 20% of patients
- Permanent and progressive damage to the pancreas
- Epigastric abdominal pain, weight loss, diarrhea, and pancreatic pseudocyst (a circumscribed collection of fluid rich in pancreatic enzymes, blood, and necrotic tissue)
Will have prandial epigastric pain. Labs will show increased serum lipase (more sensitive and specific than amylase, but only with elevations of threefold or greater)
- An abdominal CT scan is the diagnostic test of choice
- Sentinel loops on X-Ray
- look for diminished bowel sounds as part of the exam question
- A CT scan using a pancreatic protocol or MRI with magnetic resonance cholangiopancreatography (MRCP) are the best initial diagnostic tests for chronic pancreatitis
The mainstay of treatment for acute pancreatitis is supportive therapy: IV fluid resuscitation, pain control, and nutritional support
- Antibiotics for extrapancreatic infections and infected necrosis
- Endoscopic retrograde cholangiopancreatography (ERCP) for acute pancreatitis and concurrent acute cholangitis
- Complication: pancreatic pseudocyst (a circumscribed collection of fluid rich in pancreatic enzymes, blood, and necrotic tissue)
- Patients with mild pancreatitis can progress to severe pancreatitis over the initial 48 hours, often due to inadequate fluid replacement
- Referral to a tertiary center is needed if acute pancreatitis is severe or evolving/worsening
The only definitive treatment for chronic pancreatitis is to address the underlying cause, which is most commonly alcohol, low-fat diet
 Osmosis Osmosis |
|
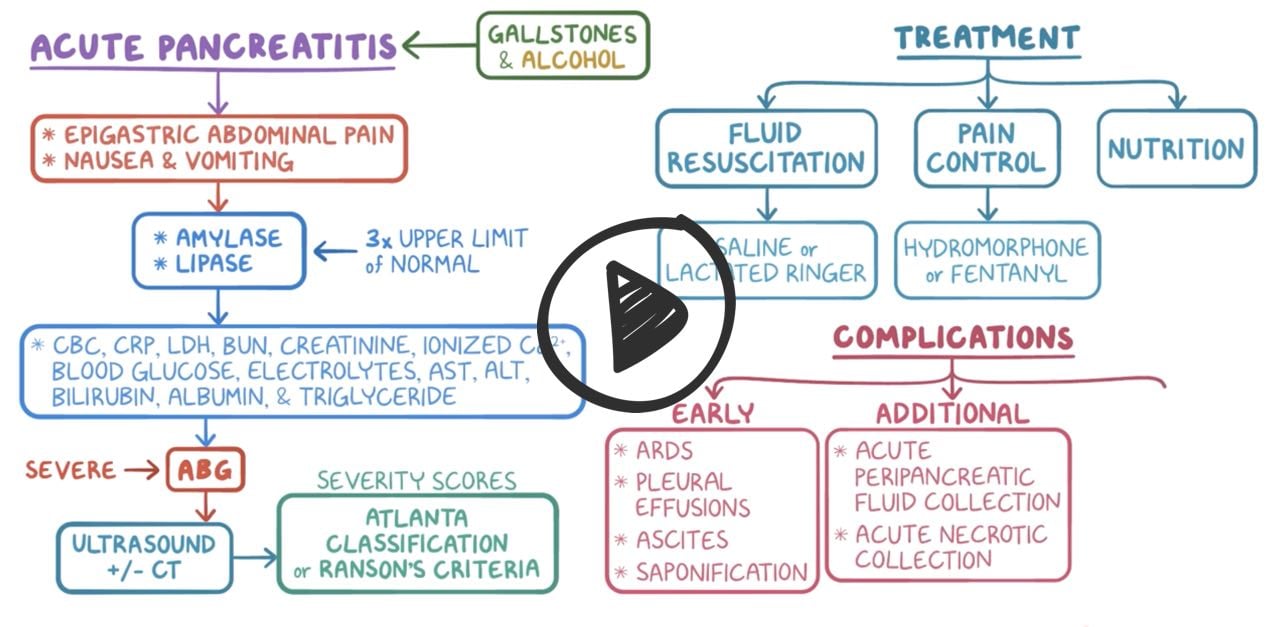 |
 Acute pancreatitis is an acute inflammation of the pancreas commonly caused by gallbladder disease or chronic alcohol intake. Symptoms often include abdominal pain, nausea, vomiting, anorexia, abdominal guarding and rigidity, decreased or absent bowel sounds. Elevated WBCs, generalized jaundice, and hypotension and tachycardia may also be present. Smoking is considered a risk factor.
Acute pancreatitis is an acute inflammation of the pancreas commonly caused by gallbladder disease or chronic alcohol intake. Symptoms often include abdominal pain, nausea, vomiting, anorexia, abdominal guarding and rigidity, decreased or absent bowel sounds. Elevated WBCs, generalized jaundice, and hypotension and tachycardia may also be present. Smoking is considered a risk factor.
Ranson’s Criteria
 A commonly used scaling system used to predict the prognosis and severity of acute pancreatitis, Ranson’s criteria consists of eleven parameters; five are assessed immediately on admission, and six are assessed as they develop over the next 48 hours, and the score is totaled. This card details the five admission criteria.
A commonly used scaling system used to predict the prognosis and severity of acute pancreatitis, Ranson’s criteria consists of eleven parameters; five are assessed immediately on admission, and six are assessed as they develop over the next 48 hours, and the score is totaled. This card details the five admission criteria.
| Ranson’s Criteria On Admission | Play Video + Quiz |
| Ranson’s Criteria During First 48 Hours | Play Video + Quiz |
Question 1 |
Acute pancreatitis | |
Acute appendicitis Hint: Usual presentation is periumbilical pain that is later referred to the right lower quadrant. No Cullen’s sign. | |
Acute cholecystitis Hint: Presents with right upper quadrant pain that is not relieved sitting and leaning forward. Not associated with Cullen’s sign. | |
Acute gastroenteritis Hint: Presents as diarrhea with vomiting, colicky abdominal pain. Pain not relieved by sitting and leaning forward. |
Question 2 |
complete blood count with differential | |
serum amylase and lipase level | |
computed tomography (CT) scan of the abdomen with contrast
| |
comprehensive metabolic panel | |
arterial blood gases |
Question 3 |
transabdominal ultrasonography | |
contrast-enhanced CT of the abdomen | |
magnetic resonance cholangiopancreatography
| |
plain radiograph (abdominal series)
|
Question 4 |
abrupt onset of epigastric pain with radiation to the back | |
nausea and vomiting
| |
elevated serum amylase
| |
all of the above
|
Question 5 |
eliminate oral intake for the first 48 hours | |
aggressive fluid replacement
| |
calcium replacement
| |
pain control
| |
intravenous H2 receptor blockers
|
Question 6 |
a “sentinel loop” | |
the “colon cutoff sign” Hint: Gas distending the right colon that abruptly stops in the mid or left transverse colon is called the colon cutoff sign. This is caused by colonic spasm adjacent to the pancreatic inflammation but is not as common as the sentinel loop. | |
air under the diaphragm Hint: Air under the diaphragm is suggestive of a perforated peptic ulcer. | |
distention in both the small bowel and the large bowel Hint: A completely distended small and large bowel suggests a distal bowel obstruction. | |
feces throughout the colon Hint: Constipation is not associated with acute pancreatitis. |
Question 7 |
pancreatic pseudocyst formation
| |
palpable gallbladder Hint: A palpable gallbladder is seen in obstruction at the ampulla or sphincter of Oddi. | |
enlarged spleen Hint: An enlarged spleen is unlikely in this patient given the clinical history, as is an enlarged liver. | |
enlarged liver |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture



