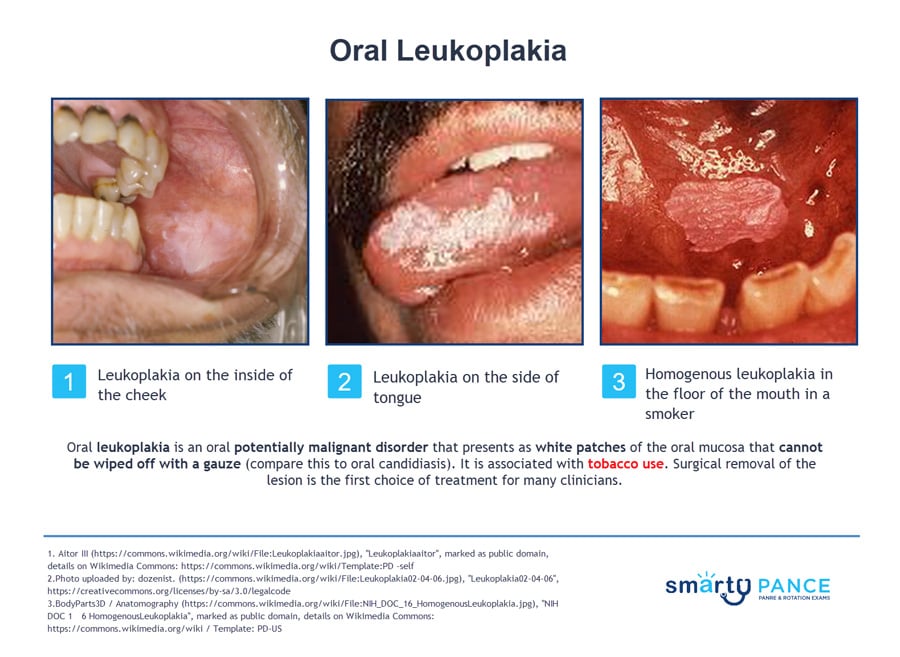
Patient will present as → a 42-year-old male with symptoms of the flu. On social history, the patient describes drinking 2-3 beers per day as well as smoking 1 pack of cigarettes per day. He is noted on physical exam to have a white plaque-like lesion on the side of the tongue, which could not be scraped off with a tongue depressor.
Oral leukoplakia is an oral potentially malignant disorder that presents as white patches of the oral mucosa that cannot be wiped off with a gauze (compare this to oral candidiasis)
- Tobacco use (smoked and especially smokeless), alcohol abuse, HPV infections
- Leukoplakia is in itself a benign and asymptomatic condition. However, about 5% will eventually develop squamous cell carcinoma (SCC)
- If there is an associated erythematous appearance (erythroplakia), there is a higher risk of dysplasia or cancer (90%)
*A separate disorder that is not premalignant is oral hairy leukoplakia, an Epstein-Barr virus-induced lesion that occurs almost entirely in HIV-infected patients
The diagnosis of leukoplakia is suspected in patients presenting with a white lesion of the oral mucosa that cannot be wiped off with gauze and that persists after eliminating potential etiologic factors, such as mechanical friction, for a six-week period
- Excisional biopsy is indicated for any undiagnosed leukoplakia
leukoplakia - all should be treated
- For 2–3 circumscribed lesions, surgical excision
- For multiple or large lesions where surgery would cause unacceptable deformity, consider cryosurgery or laser surgery
- Removal of predisposing habits (alcohol and tobacco)
- Complete excision is the standard treatment for dysplasia or malignancy
- After treatment, up to 30% of leukoplakia recurs, and some leukoplakia still transforms into squamous cell carcinoma
Oral Hairy Leukoplakia is unlikely to progress to squamous cell carcinoma
- Treatment with zidovudine, acyclovir, ganciclovir, foscarnet, and topical podophyllin or isotretinoin. Therapy is usually not indicated
Question 1 |
Alcohol consumption Hint: Weaker risk factor compared to smoking. | |
Areca nut chewing Hint: Not significantly linked. | |
Chronic gastroesophageal reflux Hint: Not specifically associated. | |
Smoking tobacco | |
Ultraviolet light exposure Hint: No evidence supporting this etiology. |
Question 2 |
Prescribe antifungal medication Hint: While antifungal medications are used for oral candidiasis, which can also present as white plaques, the history and characteristics of this lesion suggest oral leukoplakia rather than a fungal infection. A biopsy is needed for definitive diagnosis. | |
Advise cessation of smoking and alcohol use and re-evaluate in 6 months Hint: While cessation of smoking and alcohol is crucial in the management of oral leukoplakia and reducing the risk of malignant transformation, the lesion requires immediate evaluation through biopsy due to the potential for cancer. | |
Perform a biopsy of the lesion | |
Prescribe a course of oral corticosteroids Hint: Corticosteroids are not indicated in the treatment of oral leukoplakia. The mainstay of management, after biopsy and diagnosis, may involve eliminating risk factors and monitoring or surgical excision of dysplastic lesions. | |
Recommend the use of a topical anesthetic for symptom relief Hint: While topical anesthetics may provide symptom relief for painful oral lesions, this lesion is asymptomatic. The priority is to biopsy the lesion to rule out malignancy, not symptom management. |
Question 3 |
Broad spectrum antiviral medication Hint: Inappropriate treatment for oral leukoplakia or carcinoma in situ. | |
Imaging studies to evaluate involved lymph nodes Hint: Reserved only for invasive SCCA with basement membrane penetration, not CIS. | |
Supplemental vitamin A 25,000 units daily Hint: Not specifically recommended. | |
Surgical excision within 1-2 weeks Hint: Tobacco cessation more urgently needed for this smoker with CIS oral lesion prior to resection. | |
Strict tobacco cessation immediately |
|
List |
References: Merck Manual · UpToDate