47-year-old with pharyngitis and difficulty swallowing
Patient will present as → a 19-year-old male who you are seeing for follow-up from the urgent care, where he was seen 2 days earlier with a sore throat. The patient is febrile (102°F), has a muffled (hot potato) voice, and has extreme difficulty opening his mouth (trismus). He opens it just far enough for you to note uvular deviation.
To watch this and all of Joe Gilboy PA-C's video lessons, you must be a member. Members can log in here or join now.
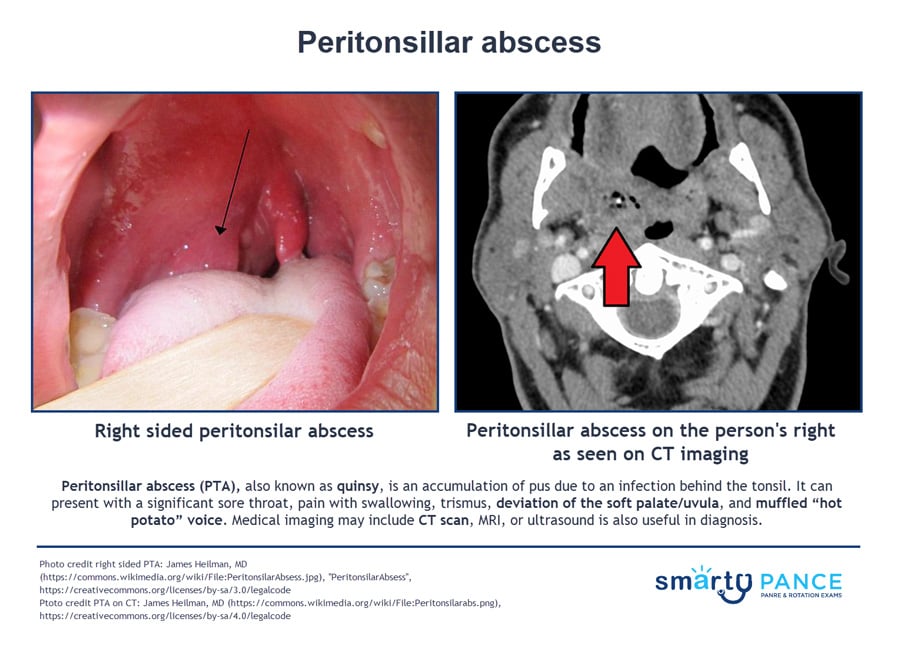
A peritonsillar abscess is a complication of tonsillitis and occurs when a collection of pus forms and spreads beyond the tonsils into the tissues of the throat next to one of the tonsils. Swollen tissues can block the airway
- A peritonsillar abscess can present with a significant sore throat, pain with swallowing, trismus (inability to open the mouth normally), deviation of the soft palate/uvula, and muffled “hot potato” voice
- Deviation of the soft palate and an asymmetric rise of the uvula is highly suggestive of abscess
- Also known as “Quincy's” abscess
- It usually involves multiple bacteria. Streptococcus and Staphylococcus are the most frequent aerobic pathogens, whereas Bacteroides sp is the predominant anaerobic pathogen
Xray, CT, or ultrasonography of the neck (which would show the collection of pus within the tissue) can help confirm the diagnosis when the physical examination is difficult, or the diagnosis is in doubt, particularly when the condition must be differentiated from a parapharyngeal infection or other deep neck infection
- All such patients require needle aspiration of the tonsillar mass and cultures. Aspiration of pus differentiates abscess from cellulitis
Treatment is surgical drainage, antibiotics, and steroids, particularly in situations where there is a lot of inflammation that obstructs the airway
- An initial 24-hour trial of appropriate parenteral antimicrobials (without surgical drainage) is justifiable in patients with presumed peritonsillar cellulitis who show no evidence of airway compromise, septicemia, severe trismus, or other complications
- Examples of antimicrobial therapy include parenteral ampicillin-sulbactam and IV clindamycin
- In less severe cases, oral antibiotics can be used for 7 to 10 days (i.e., amoxicillin, amoxicillin-clavulanate, clindamycin)
- Secure the airway early in a severe infection
- Tonsillectomy may also be considered in about 10% of patients (and those with recurrent peritonsillar abscess)
Question 1 |
Recurrent streptococcal pharyngitis Hint: This presentation suggests a complication of an incompletely treated streptococcal pharyngitis rather than recurrent disease. | |
Infectious mononucleosis Hint: Infectious mononucleosis may present with severe sore throat, fever, and cervical adenopathy in this age group, but would not cause deviation of the soft palate or the muffled voice. | |
Gonococcal pharyngitis Hint: Gonococcal pharyngitis usually follows a more indolent course than this patient's presentation. | |
Peritonsillar abscess |
Question 2 |
CBC with differential Hint: A CBC with differential would identify an infection but not specifically a retropharyngeal abscess. | |
fever and a muffled voice on examination Hint: The presence of fever and a muffled voice on physical exam is not specific for a retropharyngeal abscess. | |
CT of the neck with contrast | |
history of a recent throat infection Hint: A recent throat infection is not specific for a retropharyngeal abscess. |
Question 3 |
Needle aspiration | |
Corticosteroid administration Hint: Corticosteroids, nebulized epinephrine, and nasotracheal intubation are not indicated in the treatment of peritonsillar abscesses. | |
Nebulized epinephrine administration Hint: Corticosteroids, nebulized epinephrine, and nasotracheal intubation are not indicated in the treatment of peritonsillar abscesses. | |
Nasotracheal intubation Hint: Corticosteroids, nebulized epinephrine, and nasotracheal intubation are not indicated in the treatment of peritonsillar abscesses. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture