Patient will present as → a 51-year-old woman visiting her PA with concerns about recent changes in her menstrual cycle. She reports that her periods, which were previously regular, have become increasingly irregular over the past year, with her last menstrual period occurring six months ago. She also mentions experiencing frequent hot flashes, night sweats, and occasional mood swings. She denies any vaginal bleeding or discharge. Her medical history is unremarkable, and she is not on any medications. On examination, her vital signs are normal, and the physical examination is unremarkable. Her follicle-stimulating hormone (FSH) levels are found to be 40, consistent with menopause. The PA discusses the natural process of menopause and its symptoms with her, providing counseling on managing hot flashes and mood swings. She is advised about the importance of regular health screenings, including bone density tests, to assess for osteoporosis risk. The patient is also informed about lifestyle modifications, such as maintaining a healthy diet and regular exercise, and is offered information on hormone replacement therapy as an option for symptom management, discussing its benefits and risks.
Menopause is a natural decline in reproductive hormones when a woman reaches her 40s or 50s. It is a clinical diagnosis and is defined by:
- Cessation of menses for at least 12 months
- FSH > 30 (although not necessary for diagnosis)
The average age is 51 years (44-55 years old). On average women will spend 30+ years in the postmenopausal state
- Declines in estrogen and androstenedione (DHEA). Progesterone decreases as well but to a lesser degree
- Symptoms include irregular periods, hot flashes, irritability, and infertility
- Estrogen-responsive tissues such as the vaginal epithelium, breasts, and bones tend to atrophy in menopause
- After menopause, bone loss is 2.5% for the first 4 years and then 1% to 1.5% annually
- Due to estrogen deficiency, the vaginal pH increases from 3.5–4.5 to 6–8, predisposing it to the colonization of bacterial pathogens resulting in vaginitis and vaginal atrophy
- Atrophic endometrium and/or atrophic vaginitis are the most common causes of postmenopausal bleeding
Perimenopause is the transition between reproductive capability and menopause. The hallmark is irregular menstrual function, lasts 3-5 years
For healthy women ≥ age 45:
FSH and estradiol levels (FSH > 30) with ↓ estradiol
Menopause is a retrospective diagnosis based on 12 or more months of amenorrhea occurring at a mean age of 51 years
- The diagnosis is based on the appropriate age of a female patient for menopause (range, 45 to 55 years), symptoms of frequent classic “hot flashes,” night sweats, and the association of these symptoms with the cessation of menses
Women 40 - 45 years who present with irregular menstrual cycles and menopausal symptoms may be in the menopausal transition
- Same endocrine evaluation as for any woman with oligo/amenorrhea: serum human chorionic gonadotropin (hCG), prolactin, TSH, FSH
Women under age 40 years with irregular menses and menopausal symptoms should undergo a complete evaluation for premature ovarian failure
Hormonal Therapy: Estrogen and Progesterone replacement – Only indicated in symptomatic women
If uterus - HRT (estrogen + progesterone) if no uterus (estrogen alone) (ERT)
- For women who have had a hysterectomy, estrogen is used alone
- Oral, transdermal (patch, lotion, spray, or gel), or vaginal forms may be used. Treatment should start with the lowest dose; the dose is increased every 2 to 4 wk as needed
- Low doses include 0.3 mg PO once/day (conjugated equine or synthetic estrogens), 0.5 mg PO once/day (oral estradiol), and 0.025 mg once/day (estradiol patch)
- Women who have a uterus should be given progestin in addition to estrogen because unopposed estrogen increases the risk of endometrial cancer. The progestin is taken with estrogen continuously (i.e. daily) or sequentially (12 to 14 consecutive days of every 4 wks.)
- ↑ triglycerides
- Undiagnosed vaginal bleeding
- Endometrial cancer
- History of breast CA or estrogen-sensitive cancers
- CVD History
- DVT or PE history
For vaginal dryness, recommend vaginal stimulation and OTC vaginal lubricants and moisturizers, and if they are ineffective, prescribe low-dose vaginal estrogen creams, tablets, or rings
- OTC vaginal moisturizers (Replens, etc) 2 to 3 times a week at bedtime and encourage using lubricants (Astroglide, etc.) prior to sexual activity
- If that’s not enough, use a low-dose vaginal estrogen. Prescribe the vaginal cream (Estrace, etc) for use 2 to 3 nights per week...the tablet (Vagifem, etc) or insert (Imvexxy) twice a week...or the ring (Estring) every 3 months.
- These low-dose vaginal estrogens have minimal absorption...and usually don’t require a progestin like systemic estrogens.
Non-hormonal therapies: Cool temperatures, avoid hot, spicy foods or beverages, avoid ETOH, exercise, soy
- Alternative drugs for vasomotor symptoms
- SSRIs (paroxetine)
- SNRIs
- clonidine
- gabapentin
 Osmosis Osmosis |
|
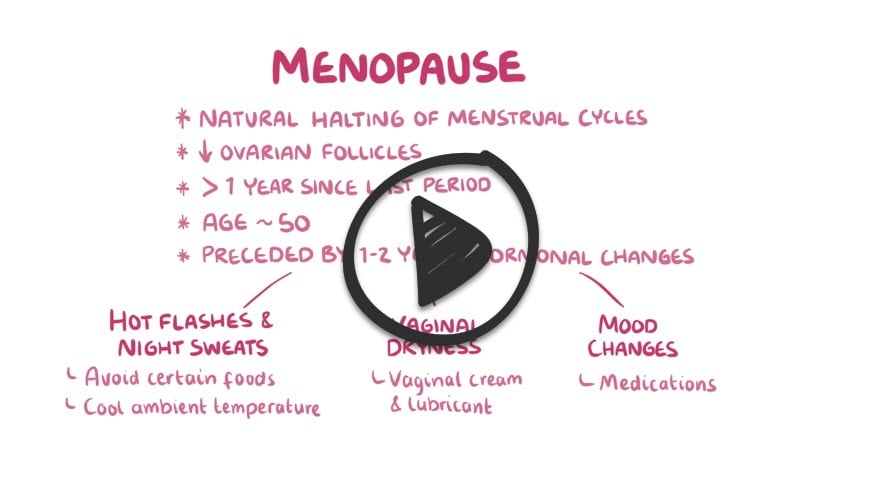 |
 Menopause is described by decreased estrogen production due to age-linked decline in ovarian follicles. It is defined as one whole year without ovulation, and the average age of menopause is 51 years old. Symptoms can be remembered with the HAVOCS mnemonic: Hot flashes, Atrophy of the Vagina, Osteoporosis, Coronary artery disease, and sleep disturbances.
Menopause is described by decreased estrogen production due to age-linked decline in ovarian follicles. It is defined as one whole year without ovulation, and the average age of menopause is 51 years old. Symptoms can be remembered with the HAVOCS mnemonic: Hot flashes, Atrophy of the Vagina, Osteoporosis, Coronary artery disease, and sleep disturbances.
| Menopause Symptoms | Play Video + Quiz |
| Menopause Lab Findings | Play Video + Quiz |
Question 1 |
pheochromocytoma | |
hyperthyroidism | |
menopause | |
generalized anxiety disorder | |
panic attacks |
Question 2 |
thyroid hormone replacement Hint: There is no strong evidence that this patient has hypothyroidism, and there is certainly no indication for empirical use of thyroid hormone without objective evidence of hypothyroidism (i.e., thyroid-stimulating hormone and thyroid function test). | |
estrogen with progestin therapy (hormone therapy [HT]) | |
antidepressants Hint: Antidepressants might help alleviate some of this patient’s symptoms, especially if she was also clinically depressed. However, this patient’s symptoms are most likely hormonally related, and HT/ ET alone often alleviates both the affective and the somatic symptoms of menopause. | |
estrogen alone (estrogen therapy [ET]) Hint: This patient still has her uterus, and ET (estrogen alone) is not recommended because of the significantly increased risk of endometrial hyperplasia or cancer with prolonged unopposed estrogen use. | |
progestin/ progesterone alone Hint: A progestin or progesterone alone may alleviate some of this patient’s symptoms, but her symptoms are related primarily to estrogen deficiency and thus respond best to ET. |
Question 3 |
breast cancer | |
endometrial cancer | |
colon cancer | |
osteoporotic fractures | |
all of the above |
Question 4 |
combined equine estrogen (CEE) appears to cause breast cancer | |
CEE appears to cause coronary heart disease (CHD) | |
medroxyprogesterone acetate appears to cause breast cancer | |
medroxyprogesterone acetate appears to cause CHD | |
daily combined use of 0.625 mg CEE and 2.5 mg medroxyprogesterone acetate progesterone (MPA) should not be initiated or continued for the primary prevention of CHD |
Question 5 |
intravaginal estrogen creams or tablets | |
an intravaginal estrogen ring | |
vaginal moisturizers | |
increased foreplay and intercourse | |
all of the above |
Question 6 |
black cohosh | |
soy isoflavones | |
red clover | |
selective serotonin reuptake inhibitors (SSRIs) and selective serotonin and norepinephrine reuptake inhibitor (SSNRIs) | |
all of the above |
|
List |
References: Merck Manual · UpToDate


