61 y/o M with recent COVID-19 infection, shortness of breath, and chest pain
Patient will present as → a 61-year-old male presents to the emergency department with a 24-hour history of chest pain, cough, and progressively worsening shortness of breath. He was diagnosed with COVID-19 after contact with an asymptomatic COVID-19 positive individual 10 days ago. At that time he reports experiencing a loss of taste and smell, fatigue, body aches, and cough. He has a history of hypercholesterolemia, hypertension, and a "heart murmur." His temperature is 98.6°F, blood pressure is 116/76 mmHg, pulse is 106/min, and respirations are 18/min with an oxygen saturation of 96% on room air. Labs are notable for an elevated D-dimer and mildly elevated troponin. EKG shows an S1Q3T3 pattern. Bedside ultrasound demonstrates marked dilation of the right ventricle with tricuspid regurgitation and elevated right ventricular systolic pressure. A CTA of the chest was performed demonstrating a large pulmonary embolism.
Most people infected with the COVID-19 virus will experience mild to moderate respiratory illness and recover without requiring special treatment
- Older people, and those with underlying medical problems like cardiovascular disease, diabetes, chronic respiratory disease, and cancer are more likely to develop serious illness
- It is thought to occur mainly through close-range contact via respiratory particles; virus released in respiratory secretions when a person with infection coughs, sneezes, or talks can infect another person if it is inhaled or makes direct contact with the mucous membranes
- Individuals with SARS-CoV-2 infection appear more likely to be infectious in the earlier stages of infection (including the few days prior to the development of symptoms)
- Transmission after 7 to 10 days of illness is unlikely, particularly for otherwise immunocompetent patients with nonsevere infection.
Symptoms
- Fever (~99% of cases)
- Fatigue (~70%)
- Dry cough (~60%)
- Myalgias (~35%)
- Dyspnea (~30%)
- Sputum (~27%)
- Anosmia (10-50%)
- Patients may develop gastrointestinal symptoms
- Nausea (~12%)
- Diarrhea (~19%)
- The incubation period is thought to be 2-14 days post-exposure
- Illness severity of this infection ranges from mild to critical
- Mild (~81% of cases)
- no dyspnea
- Severe (~14%)
- dyspnea
- respiratory rate ≥ 30/min
- hypoxia
- Critical (~5%)
- respiratory failure
- shock
- multiorgan dysfunction
- Mild (~81% of cases)
| COVID-19 Differential Diagnosis | |||||||
| Virus | Fever | Cough | Fatigue | Myalgia | Headache | Rhinitis | Sore Throat |
| COVID-19 | ↑↑↑ | ↑↑↑ | ↑↑↑ | ↑↑ | Rare | ↑ | ↑ |
| Influenza | ↑↑↑ | ↑↑↑ | ↑↑↑ | ↑↑↑ | ↑↑↑ | ↑ | ↑ |
| Common cold | Rare | ↑↑↑ | ↑ | ↑ | ↑↑ | ↑↑↑ | ↑↑↑ |
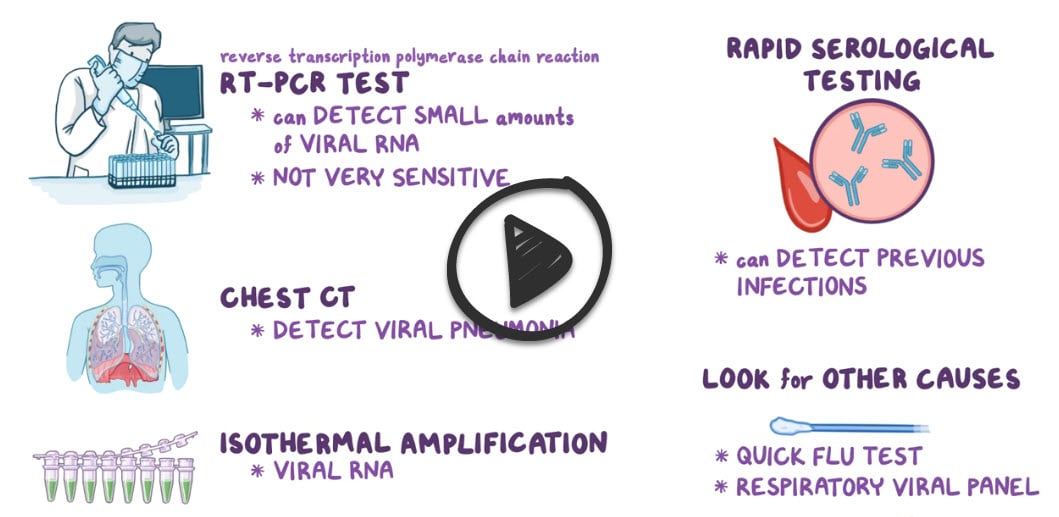
All symptomatic patients with suspected COVID-19 should undergo testing
- Nucleic acid amplification testing (NAAT), most commonly with a reverse-transcription polymerase chain reaction (RT-PCR) assay, to detect SARS-CoV-2 RNA from the upper respiratory tract is the preferred initial diagnostic test for COVID-19
- A positive NAAT for SARS-CoV-2 confirms the diagnosis of COVID-19
- Collection of a nasopharyngeal swab
- An oropharyngeal swab can also be collected (not essential)
- A positive NAAT for SARS-CoV-2 confirms the diagnosis of COVID-19
Additional testing
-
- WBC count - variable (leukopenia, leukocytosis, and lymphopenia)
- Chest CT - ground-glass opacification (GGO), consolidative abnormalities may or may not be present, more likely to affect both lungs, particularly in the lower lobes, and in a peripheral distribution
- ↑ D-dimer
- ↑ ferritin and C-reactive protein
- ↑ creatine phosphokinase
- ↑ troponin
- ↑ lactate dehydrogenase
- ↑ prothrombin time
- Acute kidney injury
- Severe lymphopenia
Indications for testing asymptomatic individuals
- Close contact with an individual with COVID-19
- Screening in congregate settings (eg, long-term care facilities, correctional and detention facilities, homeless shelters)
- Screening hospitalized patients in high-prevalence regions
- Post-exposure testing be done five to seven days after exposure, although the optimal timing is uncertain
Antigen tests that detect SARS-CoV-2 antigen can be performed rapidly and at the point of care
- Although typically less sensitive than NAATs, they can be a useful alternative for the diagnosis of patients soon after the onset of symptoms
- Antigen tests are also useful for serial screening for infection in high-risk settings (eg, congregate settings)
Diagnostic tests for COVID-19
| Test category | Primary clinical use | Specimen type | Performance characteristics | Comments |
| NAATs (including RT-PCR) | Diagnosis of current infection | Respiratory tract specimens | High analytic sensitivity and specificity in ideal settings.
Clinical performance depends on the type and quality of the specimen and the duration of illness at the time of testing. Reported false-negative rate ranges from <5 to 40%, depending on the test used. |
Time to perform the test ranges from 15 minutes to 8 hours.Δ
Turnaround time is influenced by the test used and laboratory workflow. Some assays allow home collection of specimens that are mailed in. |
| Serology (antibody detection) | Diagnosis of prior infection (or infection of at least 3 to 4 weeks' duration) | Blood | Sensitivity and specificity are highly variable.
Detectable antibodies generally take several days to weeks to develop; IgG usually develops by 14 days after onset of symptoms. Cross-reactivity with other coronaviruses has been reported. Individual results should be interpreted with caution in settings of low seroprevalence; serologic tests that have high specificity still have a low positive predictive value. |
Time to perform the test ranges from 15 minutes to 2 hours.
Turnaround time is influenced by the test used and laboratory workflow. It remains uncertain whether a positive antibody test indicates immunity against future infection. |
| Antigen tests | Diagnosis of current infection | Nasopharyngeal or nasal swabs | Antigen tests are generally less sensitive than nucleic acid tests.
Sensitivity is highest in symptomatic individuals within 5 to 7 days of symptom onset. |
Time to perform the test is <1 hour. |
Outpatient evaluation and treatment:
Patients should be referred to an outpatient clinic if they have one or more of the following features:
- Mild dyspnea in a patient with an oxygen saturation on room air between 91 to 94 percent
- Mild dyspnea in a patient with established or possible risk factors for severe disease
- Moderate dyspnea in any patient
- Symptoms concerning enough to warrant in-person evaluation (eg, mild orthostasis) but not severe enough to require ED referral
In non-hospitalized patients, dexamethasone, prednisone, or other corticosteroids are not indicated
- Patients with concomitant acute exacerbation of asthma or chronic obstructive pulmonary disease (COPD) should receive appropriate treatment with systemic glucocorticoids as indicated
- For patients with documented COVID-19, treatment with antibiotics is not indicated. Data are limited, but bacterial superinfection does not appear to be a prominent feature of COVID-19
Hospitalization
Refer patients with one or more of the following features to the ED for further management and likely hospital admission
- Severe dyspnea (dyspnea at rest, and interfering with the ability to speak in complete sentences)
- Oxygen saturation on room air of ≤90 percent, regardless of the severity of dyspnea
- Concerning alterations in mentation (eg, confusion, change in behavior, difficulty in rousing) or other signs and symptoms of hypoperfusion or hypoxia (eg, falls, hypotension, cyanosis, anuria, chest pain suggestive of acute coronary syndrome)
Treatment in hospital:
- Patients hospitalized with COVID-19 should receive pharmacologic prophylaxis for venous thromboembolism
- For patients with nonsevere disease, care is primarily supportive, with close monitoring for disease progression
- For hospitalized patients with hypoxia who are not yet on oxygen, initiate remdesivir
- For hospitalized patients who are receiving low-flow supplemental oxygen, initiate low-dose dexamethasone and remdesivir
- For patients who have significantly elevated inflammatory markers (eg, C-reactive protein [CRP] level ≥75 mg/L) and continuously increasing oxygen requirements despite dexamethasone, we add tocilizumab on a case-by-case basis
- Acetaminophen is the preferred antipyretic agent, if possible. If NSAIDs are needed, use the lowest effective dose
- People who are on an ACE inhibitor or ARB, ASA, and statins should not stop their medication.
Individuals who have close contact with someone with known or suspected COVID-19 should monitor for symptoms and self-quarantine (ie, stay at home, physically distanced from others)
- The preferred quarantine period is 14 days; shorter quarantine periods of 7 days (following a negative viral test within 48 hours) or 10 days are acceptable alternatives
- Hydroxychloroquine was one candidate agent for either pre-or post-exposure prophylaxis, but available placebo-controlled trial data suggest it is not effective in preventing infection
Prevention:
- Respiratory hygiene: maintain 6 feet of distance from others, masks (N95 respirators), and face shields or goggles for health care personnel or persons taking care of infected individuals in a health care facility or home
- Hand hygiene: hands should be washed with water and soap or virucidal hand disinfectant, avoid face touching
- Face coverings: the CDC and WHO recommend wearing masks when in public spaces and when in the presence of individuals outside of one's household
- Social and physical distancing: Avoidance of crowds and non-essential travel
- Screening for infection in high-risk settings (e.g., nursing facilities, college campuses, hospital employees): testing-based screening is advantageous compared to symptom-based screening in that it allows the identification of asymptomatic infections
Vaccines: There are several vaccines authorized and recommended to prevent COVID-19
For more information, please check out the following links
 Osmosis Osmosis |
|
 |
Coronavirus is an RNA virus, who’s genetic material is single-stranded linear and positive-sense. Its capsid is helical in shape, and enveloped. It leads to the common cold, and a particular strain of coronavirus leads to SARS (severe acute respiratory syndrome).
Play Video + QuizReferences: Merck Manual · UpToDate





