Follow along with the NCCPA™ PANCE and PANRE Cardiology Content Blueprint
- 52 PANCE and PANRE Cardiology Content Blueprint Lessons
- Hours of live recorded PANCE/PANRE video review
- 145-Question Cardiology Exam (available to Smarty PANCE members)
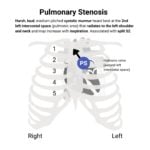
- Cardiac murmurs, cardiac pharmacology, and EKG review with Joe Gilboy PA-C
- 100's of Cardiology Pearls Flashcards covering every topic on the Blueprint
- Ten Comprehensive Cardiology Content Blueprint high-yield summary tables
- ReelDx™ integrated video content (available to Smarty PANCE + ReelDx members)
- Picmonic integrated video content and quizzes (available with Picmonic upgrade)