100% Money-Back Guarantee
No questions asked, 100% money-back guarantee anytime within 60 days of purchase + you pass or your money back!
Hurry, the 1-year membership is currently discounted for a limited time only!
We offer discounts for military veterans, group-rate and institutional pricing, and Smarty PANCE gift certificates.
Number of satisfied users
Two Week All Access Pass
- Access to all PANCE/PANRE Practice Exams (1,000's of board review questions)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses (over 450 Blueprint Topics and Modules)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE and PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!
Three Month All Access Pass
- Access to all PANCE/PANRE Practice Exams (1,000's of board review questions)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses (over 450 Blueprint Topics and Modules)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE/PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!

One Year All Access Pass
- 1 year unlimited access
- All PANCE/PANRE Practice Exams with 1,000's of board review questions (Priceless)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses with over 450 Blueprint Topics and Modules ($250 Value)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE and PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!

One Year All Access Pass + ReelDx™
- 1 year unlimited access + integrated ReelDx™ video content and ReelDx patient video content library ($249 Value)
- All PANCE/PANRE Practice Exams with 1,000's of board review questions (Priceless)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses with over 450 Blueprint Topics and Modules ($250 Value)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE and PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!
Here's What's Included When You Sign Up
Follow along with the exact NCCPA™ PANCE and PANRE Content Blueprint
Cover the entire content blueprint step by step, made simple with exam day question stems, pearls, need-to-know diagnostic studies, and gold standard treatments.
There are fourteen blueprint courses, over 467 lessons, and thousands of integrated board review questions, quizzes, and flashcards.
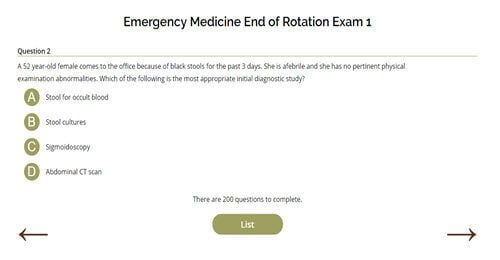
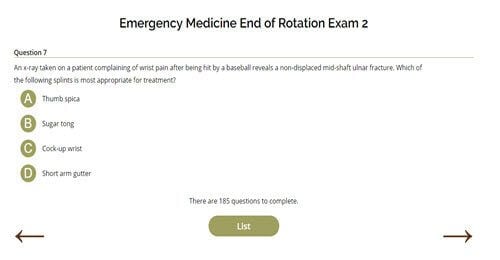
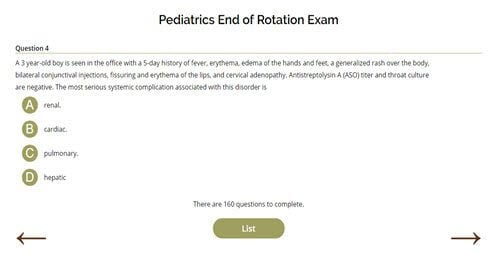
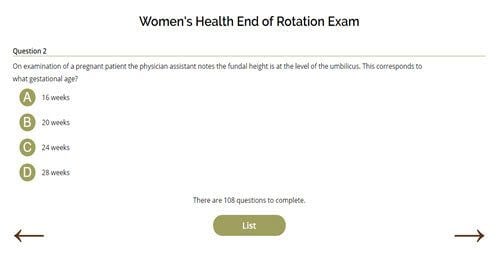
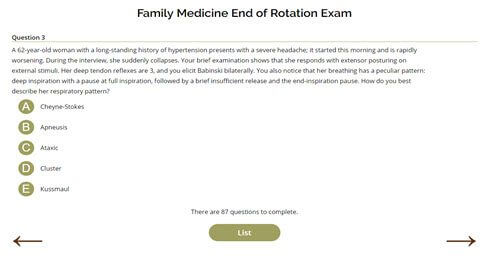
Are you a student on rotation? Instant access to seven End of Rotation Exams (and growing)!
Perfect for PANCE and PANRE preparation, current students preparing for end of rotation (EOR) exams, or self-study.
You don't need to know everything on exam day, so why not focus only on what matters?
Study Blueprint Topics and Quizzes with Real Patient Video Cases
We have partnered with ReelDx™ to give you exclusive access to real patient video cases with ultrasound, imaging, and lab data plus topics captured by providers in the ER, exam room, ambulance, and developing world. These cases are integrated directly into the NCCPA/PAEA PANCE, PANRE, and EOR Blueprint lessons and as part of our exclusive Smarty PANCE + ReelDx video content library.
*ReelDx + SMARTYPANCE members save big! Compare this to the $249/Year ReelDx standalone subscription
100's of Hours of Audio and Video Review
Say goodbye to that unproductive commute! Listen on the go with board review veteran Joe Gilboy, PA-C, as he makes learning fun and effortlessly deconstructs complex topics. Hundreds of hours of audio programming are available to all members of the Smarty PANCE.
What students are saying…
Read more Smarty PANCE member testimonials
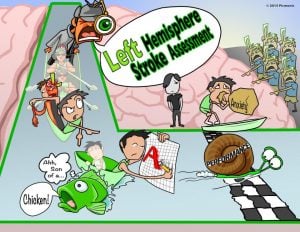
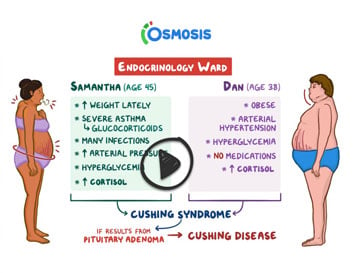
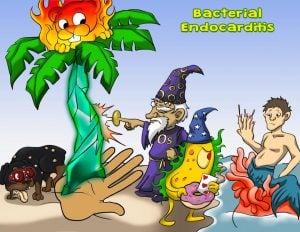
Picmonic and Osmosis Integrated NCCPA™ Content Blueprint Lessons
Seamlessly supplement your studies with high-yield Picmonics and Osmosis video lessons for everything you're struggling to remember
In randomized, double-blind, controlled studies, the Picmonic and Osmosis Learning Systems were compared to traditional learning systems and found that students improved by 331% in memory retention!
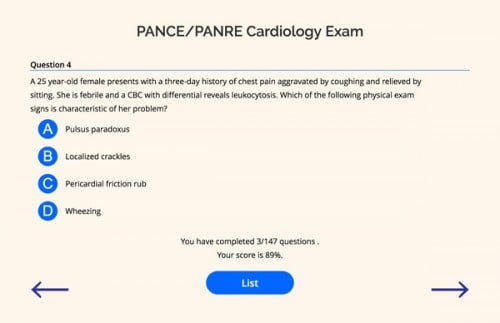
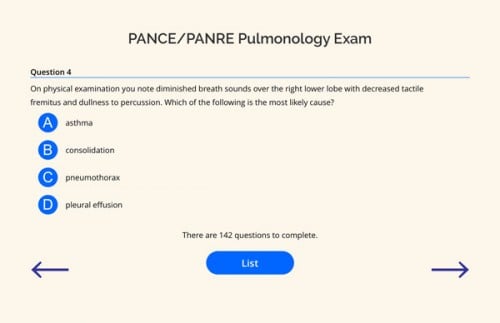
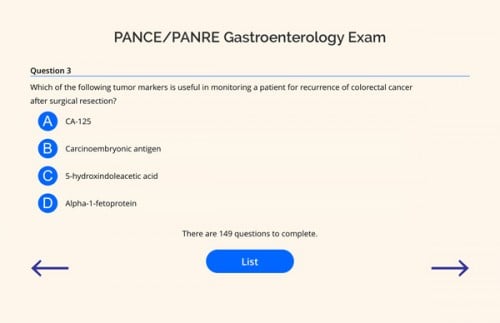
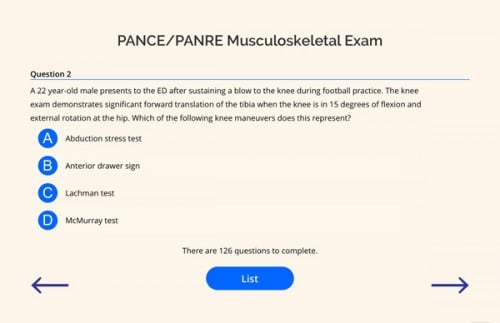
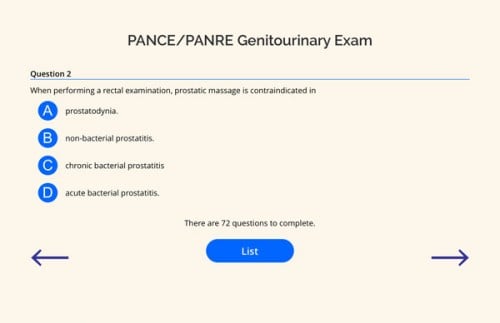
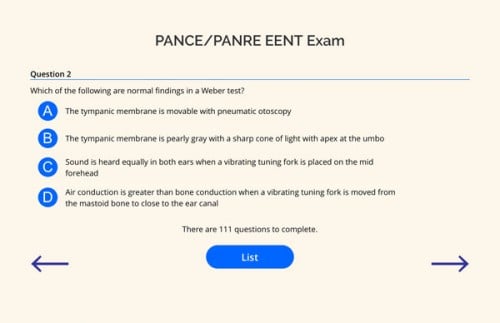
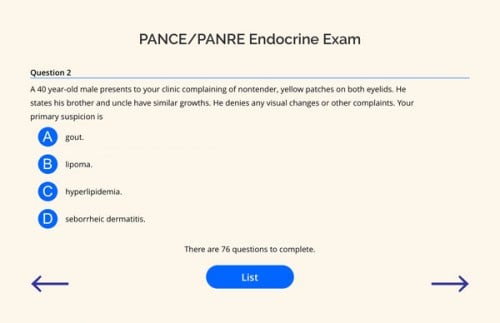
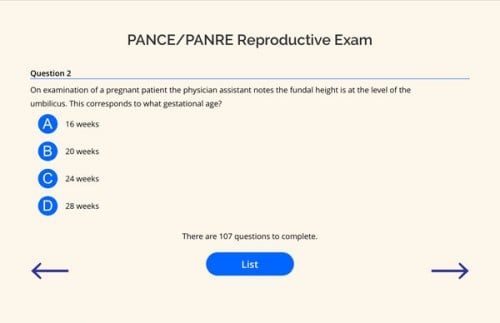
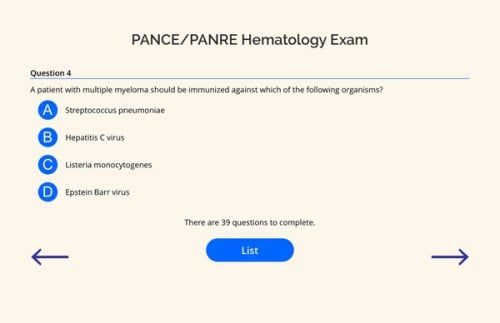
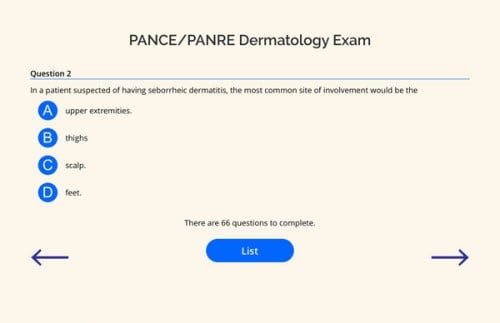
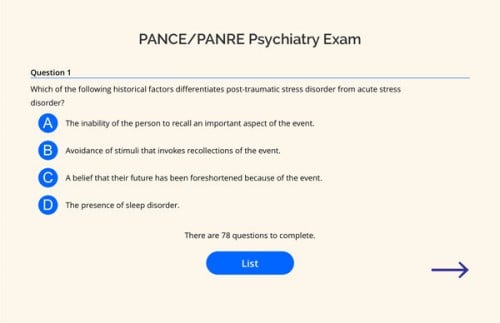
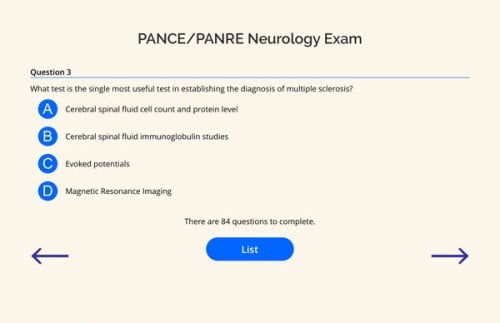
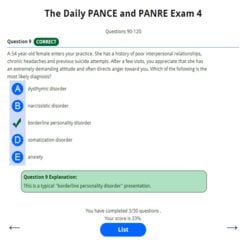
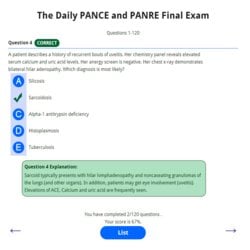
The Ultimate PANCE and PANRE QBANK
(Members Only)
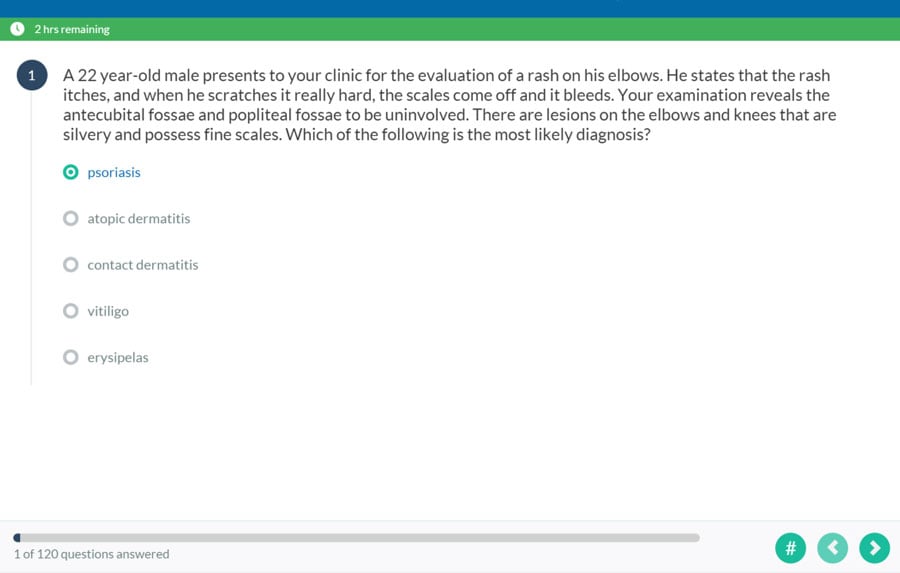
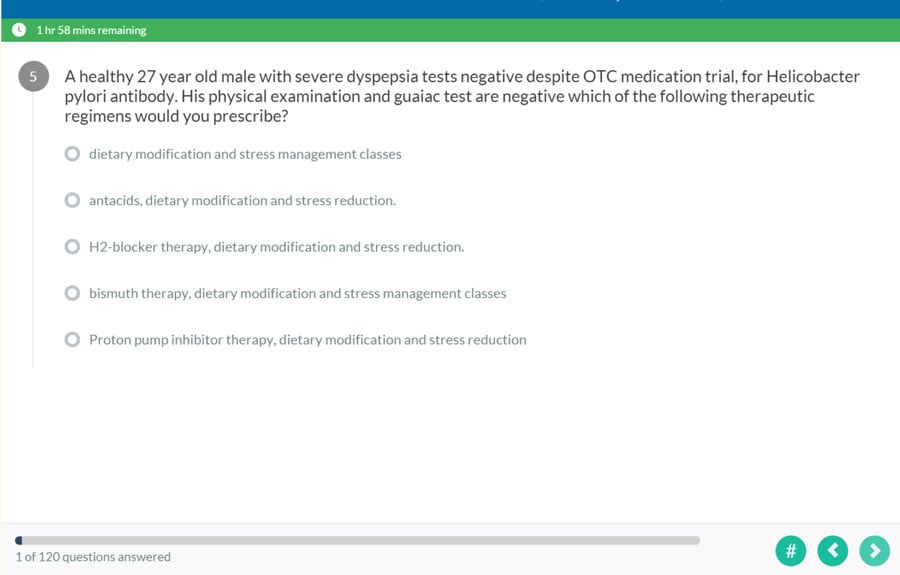
The PANCE and PANRE are made up of 100's of multiple-choice questions, so it only makes sense that your board review does the same
Thirteen Content Blueprint Topic-Specific Practice Exams with Over 1,021 Questions
Is there a specific area you need more practice with? If you have already started studying, you should have already identified some areas for improvement. I know mine. It’s neurology.
Following the NCCPA content blueprint, these exams break questions down by topic and let you focus your time on what matters most to you. Start with your weakest subject, then take some time to quiz yourself on the PANCE/PANRE hot spots: Cardiovascular, Musculoskeletal, Pulmonary, and GI.
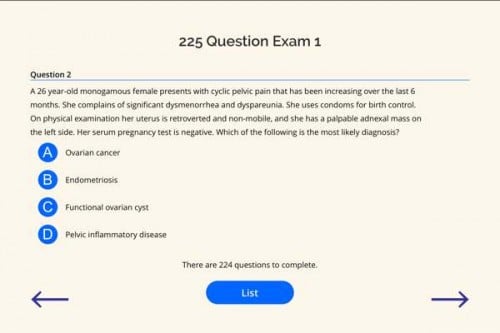
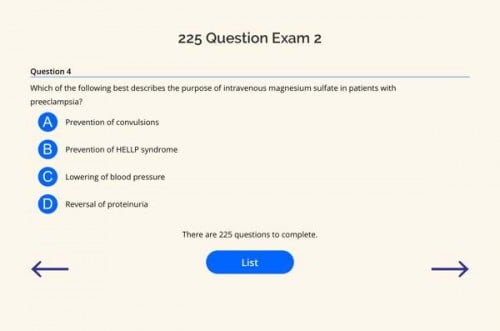
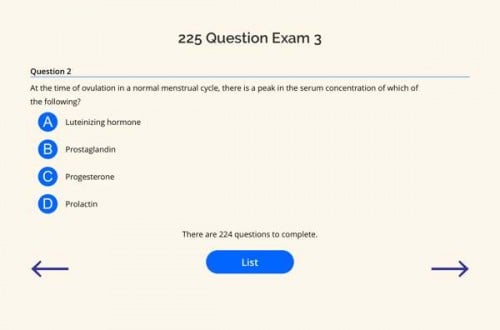
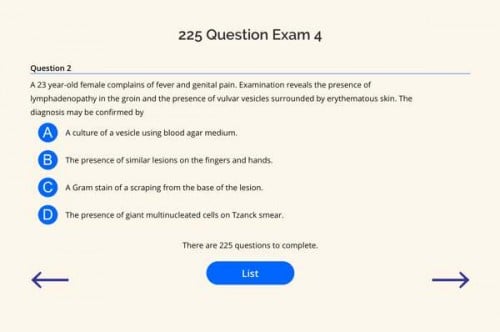
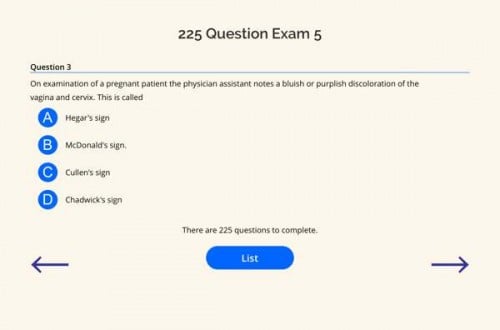
FIVE 225 Question PANCE and PANRE Practice Exams (1,225 questions)
Studies have shown, that without a doubt the most effective way to prepare for an exam is to practice within the format of the exam itself.
These five 250-question practice exams will not only keep you busy but also get you into the habit of taking an online, computer-based exam that requires patience and persistence to master. If you can make it through all these questions, you will be well on your way to PANCE/PANRE success.
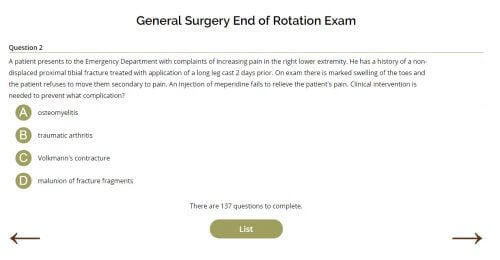
Six End of Rotation Exams (And Growing)
Are you a current student preparing for your end-of-rotation exams? Use these end-of-rotation exams which follow the PAEA EOR blueprint and topic list to nail down essential rotation-specific knowledge.
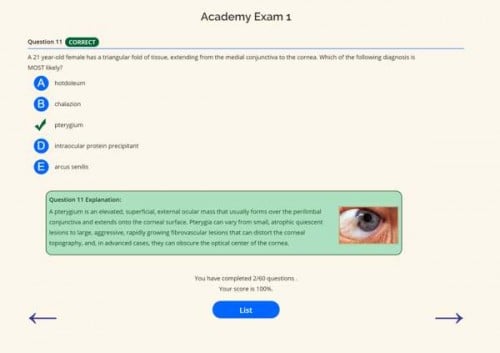
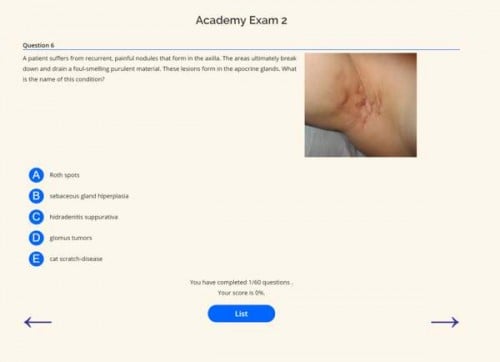
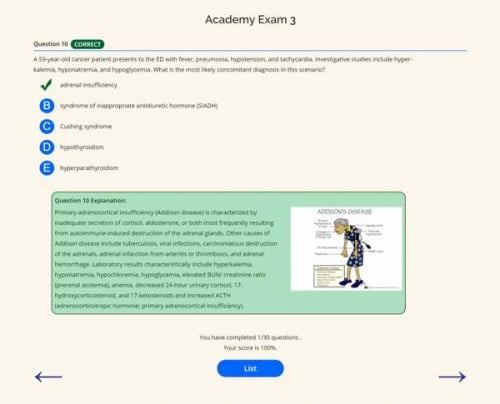
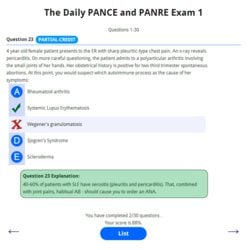
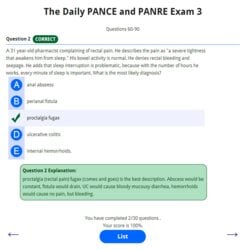
Four 60 Questions Interactive Academy Exams
These exams are built with your learning in mind—now even more interactive with photos, videos, tables, ECGs, “learning links,” and more!
Two 120-Question Comprehensive PANCE and PANRE Exams
These are my original 120-question PANCE and PANRE practice exams.
These are graded, timed exams, and just like the actual PANCE and PANRE, you will have 1 minute to complete each question. You will have the ability to review your answers at the end.
The 120-Question Daily PANCE and PANRE Email Exam Series
These exams are built to test your knowledge of the daily PANCE and PANRE email series (sign up below)
Each exam consists of questions from the corresponding day the question (or questions) were sent. Therefore, exam one consists of questions from days 1-30, exam two is from days 30-60, and the third and fourth exams are composed of additional questions included in the fast-track email series (if you signed up).
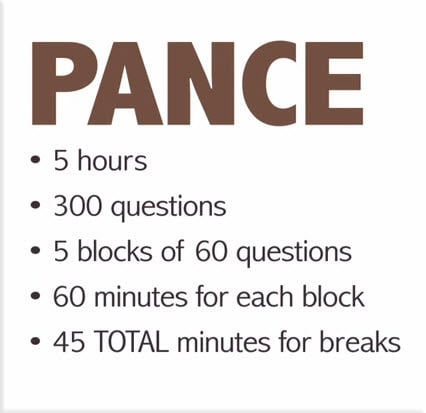
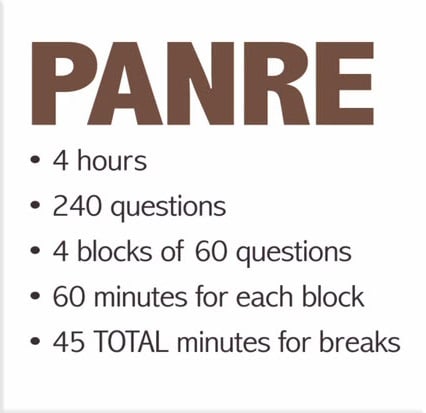
300 Question Timed Virtual PANCE and PANRE
The goal of this exercise is to simulate your actual test day as best as we can.
By practicing within this environment, you will make great strides in decreasing your anxiety come test day.
Before you start your virtual exam, make sure you have at least 5 hours and eliminate all distractions. Commit to completing all the blocks in one sitting!
Not ready to tackle the entire virtual PANCE or PANRE?
Now, you can study each block on its own or review the blocks with interactive hints and teaching points. Follow the links below to study and learn from each 60-question block until you can do it with your eyes closed. Then take your virtual PANCE or PANRE
Sign up for the FREE Daily PANCE and PANRE Email Series
Also included with each membership is an additional premium 30-day fast-track email series with sixty additional questions
High Yield PANCE and PANRE Flashcards as Part of all Learning Modules
Solidify high-yield concepts through these PANCE and PANRE Pearl flashcards (included with each course)
Quizlet Mobile (Flashcards) - 300 Daily Challenge Flashcard sets broken into bite-sized morsels designed to keep you on the ball. Now available with email auto-reminders!
Using the Quizlet App on your smartphone or reading device is a great way to study. You must install the appropriate App for your device, create an account with Quizlet, and then use the "flashcard" links and passwords included to access the PANCE and PANRE Practice exam flashcards.
 *You can access all Flashcard sets on Quizlet or with the Quizlet mobile app.
*You can access all Flashcard sets on Quizlet or with the Quizlet mobile app.
Available as a Mobile app on most platforms:
- iOS (iPhone, iPad, iPod Touch)
- Android
- Kindle Fire
- Windows Phone
- Nook
The Audio PANCE and PANRE (Members Only Addition)
 The Audio PANCE and PANRE is a multiple choice PANCE and PANRE audio exam to study on the go.
The Audio PANCE and PANRE is a multiple choice PANCE and PANRE audio exam to study on the go.
The podcast is currently available on Stitcher and iTunes but is limited to every other episode. Members of the SMARTY PANCE receive the full premium audio package containing over 4 hours and 260 questions of Audio for FREE when you register.
To top it off, the SMARTY PANCE version is updated with new content monthly and will download to your mobile device automatically when used with any podcasting app.
Episode 35 (Questions 1-10)
"Great review for the PANCE and PANRE! I am taking my PANRE in 2 months, so I was delighted to find this podcast and take it with me on my 30-minute commute to work. Having 10 Questions per episode breaks the material down into manageable “chunks,” and learning with test questions seems appropriate given that is what we will be facing come test day. So happy to have this podcast, can’t thank you enough!"
Smarty PANCE has helped over 40,000 PAs like yourself pass their boards and end of rotation exams
Read more Smarty PANCE member testimonials
PANCE and PANRE 233 Topic Review Tables
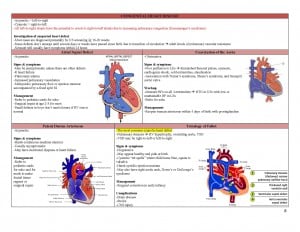 I must thank my friend over at “The Running PA” for sharing these review tables. I have compiled these tables into 233 easy-to-study slides. As a member, you will gain FREE access to download this compilation or review it online.
I must thank my friend over at “The Running PA” for sharing these review tables. I have compiled these tables into 233 easy-to-study slides. As a member, you will gain FREE access to download this compilation or review it online.
You will have 3 Options:
- View in browser
- Download individual jpg flashcards (to view in your photo viewer)
- Download as a single PDF
Compare Smarty PANCE to Other Popular Online Resources
Online Exam Sites (Limited and Pricey)
- NCCPA 120 Question Exam: $50 per 120-question exam ($500 for 1,200 questions)
- Kaplan Question Bank + high yield: $499 for 1,100 questions
- Exam Master: $600 for twelve months
- HippoPA: $390 for 1,700 questions and three months of access
Comprehensive Exam Review (Pricey)
In my opinion, these comprehensive but very pricey review courses are not always better than a good review book and a whole lot of practice questions. This may be the way to go if you have been away from the profession for some time, but given the price, it is often just not worth the money.
Nothing Beats Real-World Practice
Smarty PANCE is built for physician assistants by physician assistants. It is built upon clinical vignettes and highly focused multiple-choice questions (literally 1,000s of them) to take the pain out of learning and focus on the essentials while replicating exactly what you will see come test day.
Smarty PANCE works. Since launching in January 2014, over 65,000 people have signed up and benefited from these materials; I am proud to say that we have close to a 100% pass rate, and the feedback has been wonderful
Smarty PANCE is affordable! Because great review should blow your mind, not your bank!
Smarty PANCE works great on your iPad! These exams have large touch-friendly buttons, an adaptive design to fit all screen sizes, and a large font. They work perfectly on an iPad or tablet device, and you won't need to buy a new pair of prescription glasses.
100% Money-Back Guarantee!
No questions asked, and there is a 100% money-back guarantee anytime within 60 days of purchase + you pass or your money back!
(Hurry, the 1-year membership is currently discounted for a limited time only)
Two Week All Access Pass
- Access to all PANCE/PANRE Practice Exams (1,000's of board review questions)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses (over 450 Blueprint Topics and Modules)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE and PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!
Three Month All Access Pass
- Access to all PANCE/PANRE Practice Exams (1,000's of board review questions)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses (over 450 Blueprint Topics and Modules)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE/PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!

One Year All Access Pass
- 1 year unlimited access
- All PANCE/PANRE Practice Exams with 1,000's of board review questions (Priceless)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses with over 450 Blueprint Topics and Modules ($250 Value)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE and PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!

One Year All Access Pass + ReelDx™
- 1 year unlimited access + integrated ReelDx™ video content and ReelDx patient video content library ($249 Value)
- All PANCE/PANRE Practice Exams with 1,000's of board review questions (Priceless)
- Access to all 14 NCCPA PANCE/PANRE Blueprint Courses with over 450 Blueprint Topics and Modules ($250 Value)
- Picmonic™ integration
- Seven End of Rotation Exams (and growing)
- Seven End of Rotation Review Courses
- End of Curriculum™ Exam Course
- Audio and Video Lectures with Joe Gilboy PA-C
- FREE Subscription to Fast Track Email Series
- Premium subscription to the Audio PANCE and PANRE Podcast (Over 12 hours of audio board review content)
- PANCE/PANRE Board Review Flashcard Sets (1000's of topic specific high yield flashcards)
- PANCE and PANRE Board Review Tables
- Access to the Smarty PANCE Member Community!