The multiple endocrine neoplasias (MEN) syndromes comprise four genetically distinct inherited familial diseases involving adenomatous hyperplasia and malignant tumors in several endocrine glands.
- MEN are inherited conditions with the propensity to develop multiple endocrine tumors.
- MEN follows an autosomal dominant inheritance pattern with incomplete penetrance and symptoms and signs that develop at any age.
- The endocrine glands affected in multiple endocrine neoplasia are the pituitary gland, the thyroid gland, the parathyroid glands, the adrenal glands, and the pancreas.
- MEN 1 (3 Ps) – Parathyroid, Pituitary, Pancreatic
- MEN 2A (2Ps, 1M) – Pheochromocytoma, Parathyroid, Medullary Thyroid Ca
- MEN 2B (1P, 2Ms) – Pheochromocytoma, Medullary Thyroid Ca, Marfanoid habitus/mucosal neuroma
MEN 4 – Men IV syndrome is clinically indistinguishable from MEN I syndrome EXCEPT that it occurs due to a mutation in CDKN1B
Four Types of Multiple Endocrine Neoplasia (MEN):
MEN 1 (Wermer syndrome) - MEN 1 involves primarily hyperplasia or sometimes adenomas of the parathyroid glands (with resultant hyperparathyroidism) and tumors of the pancreatic islet cells and/or pituitary gland.
- 3 P's for MEN 1: P arathyroid, P ancreatic, P ituitary- The most common tumor is a parathyroid tumor!
- Parathyroid hyperplasia (in 90% of the patients with MEN I)
- Pancreatic islet cell tumors (in two-thirds of the patients with MEN I)—ZES (50%), insulinoma (20%)
- Pituitary tumors (in two-thirds of the patients with MEN I)
MEN type 2A (Sipple syndrome) - MEN 2A involves primarily medullary thyroid carcinoma, pheochromocytoma, hyperplasia, or sometimes adenomas of the parathyroid glands (with resultant hyperparathyroidism).
- (2Ps, 1M) P heochromocytoma, P arathyroid, M edullary Thyroid Ca
- Medullary thyroid carcinoma (in 100% of the patients with MEN IIA)
- Pheochromocytoma (in more than one-third of the patients with MEN IIA)
- Parathyroid hyperplasia (in 50% of the patients with MEN IIA)
MEN type 2B (also called MEN 3) - MEN 2B involves primarily medullary thyroid carcinoma, pheochromocytoma, multiple mucosal and mucosal neuromas, and marfanoid habitus.
- In MEN 2B, the type of tumors are the same as 2A, except there is no parathyroid adenoma. Instead, they have multiple neuromas, which are tumors that come from nerve tissue in the skin and mouth and marfanoid body habitus.
- (1P, 2Ms) - P heochromocytoma, M edullary Thyroid Ca, M arfanoid habitus/mucosal neuroma
- Mucosal neuromas (in 100% of the patients with MEN IIB)—in the nasopharynx, oropharynx, larynx, and conjunctiva
- Medullary thyroid carcinoma (in 85% of the patients with MEN IIB)—more aggressive than in MEN IIA
- Marfanoid body habitus
- Pheochromocytoma
MEN 4 syndrome is clinically indistinguishable from MEN I syndrome EXCEPT that it occurs due to a mutation in CDKN1B
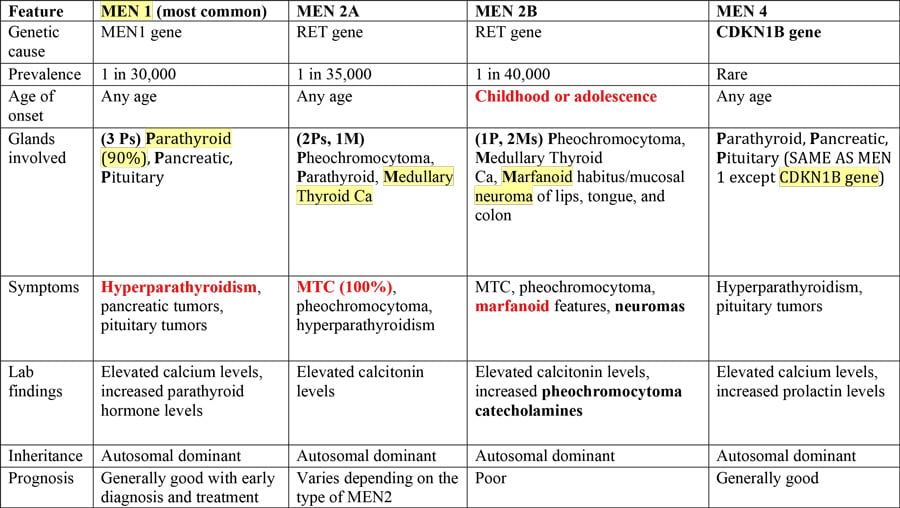
Here is a table summarizing the four types of MEN, highlighting the key differences:
| Feature | MEN 1 (most common) | MEN 2A | MEN 2B | MEN 4 |
| Genetic cause | MEN1 gene | RET gene | RET gene | CDKN1B gene |
| Prevalence | 1 in 30,000 | 1 in 35,000 | 1 in 40,000 | Rare |
| Age of onset | Any age | Any age | Childhood or adolescence | Any age |
| Glands involved | (3 Ps) - Parathyroid (90%), Pancreatic, Pituitary | (2Ps, 1M) Pheochromocytoma, Parathyroid, Medullary Thyroid Ca | (1P, 2Ms) - Pheochromocytoma, Medullary Thyroid Ca, Marfanoid habitus/mucosal neuroma of lips, tongue, and colon | Parathyroid, Pancreatic, Pituitary (SAME AS MEN 1 except CDKN1B gene) |
| Symptoms | Hyperparathyroidism, pancreatic tumors, pituitary tumors | Medullary thyroid cancer (100%), pheochromocytoma, hyperparathyroidism | MTC, pheochromocytoma, marfanoid features, neuromas | Hyperparathyroidism, pituitary tumors |
| Lab findings | Elevated calcium levels, increased parathyroid hormone levels | Elevated calcitonin levels | Elevated calcitonin levels, increased pheochromocytoma catecholamines | Elevated calcium levels, increased prolactin levels |
| Inheritance | Autosomal dominant | Autosomal dominant | Autosomal dominant | Autosomal dominant |
| Prognosis | Generally good with early diagnosis and treatment | Varies depending on the type of MEN2 | Poor | Generally good |
- In MEN type 1 – a pituitary adenoma might press on nearby brain tissue, causing headaches, or it could press on the optic nerves, causing vision problems.
- In MEN type 2 A and B – a thyroid tumor might compress nearby organs in the neck, causing hoarseness, coughing, and trouble swallowing.
- In MEN type 2B – neuromas typically grow on the tongue, lips, and the roof of the mouth.
- In MEN type 4 – is the same as type 1, except genetic testing will reveal a mutation in the CDKN1B gene.
The multiple endocrine neoplasias (MEN) syndromes are covered as part of your PANCE Endocrinology Blueprint under the topic of Endocrine Neoplasms and as part of the Endocrine System End of Curriculum Exam Blueprint.
Smarty PANCE Members can view associated clinical vignettes covering each MEN subtype and review clinical PEARLS, along with appropriate diagnosis and treatment. Take some time to review the table above and understand the key differences associated with each of the MEN syndromes. Most questions on this topic will revolve around your ability first to identify MEN and then differentiate between the different types of MEN syndromes. If you know the key differences, you should have no problem answering this question correctly.
Happy Studying!
Stephen Pasquini PA-C