Congratulations - you have completed ACADEMY Exam 1.
You scored %%SCORE%% out of %%TOTAL%%.
Your performance has been rated as %%RATING%%
%%FORM%%
Have Your Exam Results Emailed to You
Enter your name and email address below to have your results as well as the test questions, your answers and the correct answers delivered to your inbox.
Your answers are highlighted below.
Question 1 |
A 22-year-old male presents to your clinic for the evaluation of a rash on his elbows. He states that the rash itches, and when he scratches it hard, the scales come off and it bleeds. Examination reveals the antecubital fossae and popliteal fossae to be uninvolved. There are lesions on the elbows and knees that are silvery and possess fine scales. Which of the following is the most likely diagnosis?
Atopic dermatitis | |
Contact dermatitis | |
Psoriasis | |
Vitiligo | |
Erysipelas |
Question 1 Explanation:
Psoriasis is a chronic skin condition characterized by well-demarcated plaques with silvery scales, commonly located on the elbows, knees, scalp, and lower back. The description of the rash in this patient, particularly the presence of silvery scales and the tendency to bleed when scratched (Auspitz sign), is highly indicative of psoriasis. Psoriasis is an autoimmune condition and can be associated with joint pain in some individuals (psoriatic arthritis). (Review Blueprint Topic: Psoriasis)
Question 2 |
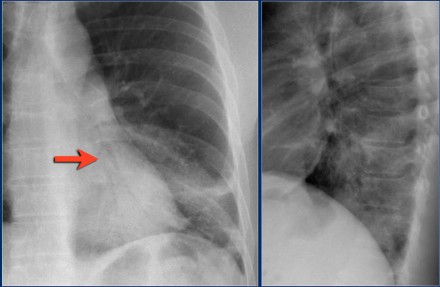
A 42 year-old healthy male presents with an acute cough, right sided chest pain with inspiration, a fever and a history of a single, shaking chill. He has localized rales in the right base. Which of the following is the most likely etiology of his pneumonia?
Streptococcus pneumoniae | |
Hemophilus influenza | |
Staphylococcus aureus | |
Mycoplasma pneumoniae | |
Pseudomonas aeruginosa |
Question 3 |
A 48 year-old male presents for an evaluation of hypertension. His CBC and serum chemistries are normal. His urinalysis reveals 15 RBCs/HPF. His abdominal ultrasound demonstrates multiple, bilateral fluid collections within the kidneys. Which diagnosis is most likely?
renal carcinoma (bilaterally) | |
medullary sponge kidneys | |
Goodpasture's Syndrome | |
renal artery stenosis | |
polycystic kidney disease |
Question 3 Explanation:
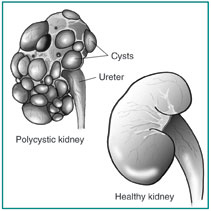 Polycystic kidney disease is a kidney disorder passed down through families in which many cysts form in the kidneys, causing them to become enlarged.
PKD can also cause cysts in the liver and problems in other organs, such as blood vessels in the brain and heart. The number of cysts as well as the complications they cause help doctors distinguish PKD from the usually harmless "simple" cysts that often form in the kidneys in later years of life.
Polycystic kidney disease is a kidney disorder passed down through families in which many cysts form in the kidneys, causing them to become enlarged.
PKD can also cause cysts in the liver and problems in other organs, such as blood vessels in the brain and heart. The number of cysts as well as the complications they cause help doctors distinguish PKD from the usually harmless "simple" cysts that often form in the kidneys in later years of life.
Question 4 |
An 18 year-old male is brought to you facility by his sister. She states that recently he has been not himself. His mood has been alternating from happy and euphoric to irritable and depressed. On examination, you note marked nasal congestion, dilated pupils, a heart rate of 116 and an elevated blood pressure. You suspect:
an acute narcotic overdose | |
cocaine intoxication | |
acute anxiety | |
an acute manic episode | |
a personality disorder |
Question 4 Explanation:
Nearly every organ system can be affected by cocaine toxicity. Aside from alcohol (and not including tobacco-related illnesses), cocaine is the most common cause of drug-related emergency department (ED) visits in the United States.
There are 3 reported phases of acute cocaine toxicity. In fatal cases, the onset and progression are accelerated, with convulsions and death frequently occurring in 2-3 minutes, though sometimes in 30 minutes.
Learn More
Question 5 |
A healthy 27 year old male with severe dyspepsia tests negative despite OTC medication trial, for Helicobacter pylori antibody. His physical examination and guaiac test are negative which of the following therapeutic regimens would you prescribe?
dietary modification and stress management classes | |
antacids, dietary modification and stress reduction. | |
H2-blocker therapy and stress reduction. | |
bismuth therapy, dietary modification and stress managment classes | |
Proton pump inhibitor therapy,dietary modification and stress reduction |
Question 5 Explanation:
Treatment of gastroesophageal reflux disease involves a stepwise approach. The goals are to control symptoms, to heal esophagitis, and to prevent recurrent esophagitis or other complications. The treatment is based on lifestyle modification and control of gastric acid secretion through medical therapy with antacids or proton pump inhibitors or surgical treatment with corrective antireflux surgery. Learn More
Question 6 |
All of the following are MAJOR manifestation of acute rheumatic fever as described by the Modified Jones criteria EXCEPT:
carditis | |
polyarthritis | |
a fever > 102.2 F (39 degrees C) | |
erythema marginatum. | |
chorea |
Question 6 Explanation:
JONES CRITERIA:
Major criteria:
- Joint (arthritis)
- Obvious (Cardiac)
- Nodule (Rheumatic)
- Erythema marginatum
- Sydenham chorea
- Inflammatory cells (leukocytosis)
- Temperature (fever)
- ESR/CRP elevated
- Raised PR interval
- Itself (previous Hx of Rheumatic fever)
- Arthralgia
Question 7 |
The drug of choice for Mycoplasma pneumonia during pregnancy is:
tetracycline | |
erythromycin | |
albuterol | |
ciprofloxacin | |
amoxicillin |
Question 8 |
A patient has a documented anaphylactic allergic reaction to penicillin. Which of the following agents would most appropriate to prescribe as a substitute, when clinically warranted?
amoxicillin | |
bacampicillin | |
cephalexin | |
clarithromycin | |
cloxacillin |
Question 8 Explanation:
 Penicillin antibiotics are the most common cause of drug allergies. Some people who are allergic to penicillin are also allergic to other closely related antibiotics, including cephalosporins, such as cephalexin, cefprozil, and cefuroxime.
Many people who believe that they have an allergy to penicillin do not. They currently may be less sensitive to penicillin than they were in the past. Or they may have had an adverse reaction, such as a side effect, rather than an allergic reaction. A skin test is the best way to find out whether you have a penicillin allergy.
Penicillin antibiotics are the most common cause of drug allergies. Some people who are allergic to penicillin are also allergic to other closely related antibiotics, including cephalosporins, such as cephalexin, cefprozil, and cefuroxime.
Many people who believe that they have an allergy to penicillin do not. They currently may be less sensitive to penicillin than they were in the past. Or they may have had an adverse reaction, such as a side effect, rather than an allergic reaction. A skin test is the best way to find out whether you have a penicillin allergy.
Question 9 |
According to the Parkland formula (4 ml/kg % body surface area burned), of the total fluid requirements during the first 24 hours after a burn, one-half (50%) of the fluid should be administered over the initial:
2 hours | |
4 hours | |
8 hours | |
12 hours | |
16 hours |
Question 9 Explanation:
Burn Injury Fluid Resuscitation, Adult (Parkland crystalloid estimate)
Total Crystalloid For First 24 Hours = 4 (x ) Weight (x) Percent Nonsuperficial BurnArea
Learn More
Question 10 |
A patient with notching of the maxillary incisors most likely:
has a history of congenital syphilis. | |
Was exposed in utero to tetracycline. | |
Was administered a sulfa product before age two months. | |
Had an intraoral infection with Mycoplasma pneumoniae. | |
Continued pacifier use extending into the third year of age. |
Question 10 Explanation:
Congenital syphilis is syphilis present in utero and at birth, and occurs when a child is born to a mother with secondary syphilis. Untreated syphilis results in a high risk of a poor outcome of pregnancy, including mulberry molars in the fetus. Syphilis can cause miscarriages, premature births, stillbirths, or death of newborn babies. Some infants with congenital syphilis have symptoms at birth, but most develop symptoms later. Untreated babies can have deformities, delays in development, or seizures along with many other problems such as rash, fever, hepatosplenomegaly, anemia, and jaundice. Sores on infected babies are infectious. Rarely, the symptoms of syphilis go unseen in infants so that they develop the symptoms of late-stage syphilis, including damage to their bones, teeth, eyes, ears, and brain.
Question 11 |
A 21 year-old female has a triangular fold of tissue, extending from the medial conjunctiva to the cornea. Which of the following diagnosis is MOST likely?
hordeolum | |
chalazion | |
pterygium | |
intraocular protein precipitant | |
arcus senilis |
Question 11 Explanation:
 A pterygium is an elevated, superficial, external ocular mass that usually forms over the perilimbal conjunctiva and extends onto the corneal surface. Pterygia can vary from small, atrophic quiescent lesions to large, aggressive, rapidly growing fibrovascular lesions that can distort the corneal topography, and, in advanced cases, they can obscure the optical center of the cornea.
A pterygium is an elevated, superficial, external ocular mass that usually forms over the perilimbal conjunctiva and extends onto the corneal surface. Pterygia can vary from small, atrophic quiescent lesions to large, aggressive, rapidly growing fibrovascular lesions that can distort the corneal topography, and, in advanced cases, they can obscure the optical center of the cornea.
Question 12 |
A 5 year-old female is brought to your facility by her parents. They have noted increasing ataxia in their daughter over the past two weeks. An MRI of the brain demonstrates a mass arising from the roof of the fourth ventricle. What is the most likely diagnosis?
astrocytoma | |
ependyoma | |
glioblastoma multiforme | |
hemangioblastoma | |
medulloblastoma |
Question 12 Explanation:
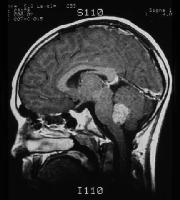 Medulloblastoma (seen in the image below) is the most common malignant brain tumor in children, accounting for 10-20% of primary CNS neoplasms and approximately 40% of all posterior fossa tumors.
Learn more
Medulloblastoma (seen in the image below) is the most common malignant brain tumor in children, accounting for 10-20% of primary CNS neoplasms and approximately 40% of all posterior fossa tumors.
Learn moreQuestion 13 |
Which of the following is the most common childhood malignancy?
Hodgkin's lymphoma | |
Non-Hodgkin's lymphoma | |
Acute myelogenous leukemia (AML) | |
Acute lymphoblastic leukemia (ALL) | |
Neuroblastoma |
Question 13 Explanation:
Acute lymphoblastic leukemia (ALL) is the most common malignancy diagnosed in children, representing nearly one third of all pediatric cancers.
Children with acute lymphoblastic leukemia (ALL) often present with signs and symptoms that reflect bone marrow infiltration and/or extramedullary disease. When leukemic blasts replace the bone marrow, patients present with signs of bone marrow failure, including anemia, thrombocytopenia, and neutropenia.
Learn More
Question 14 |
A patient's serum glycosylated hemoglobin result is 11%. Which of the following most closely approximates the average serum glucose level during the previous eight weeks?
90- 139 | |
140 - 169 | |
170 - 219 | |
220 - 330 | |
331 - 400 |
Question 14 Explanation:
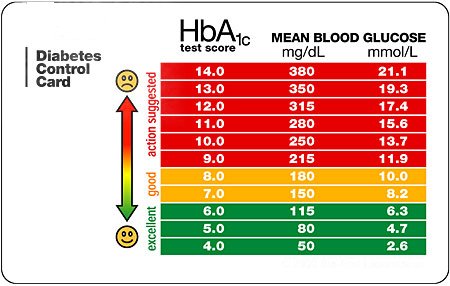 Of interest, studies have shown that there is a 10% decrease in relative risk for every 1% reduction in A1c.
So, if a patients starts off with an A1c of 10.7 and drops to 8.2, though they are not yet at goal, they have managed to decrease their risk of microvascular complications by about 20%. The closer to normal the A1c, the lower the absolute risk for microvascular complications.
Of interest, studies have shown that there is a 10% decrease in relative risk for every 1% reduction in A1c.
So, if a patients starts off with an A1c of 10.7 and drops to 8.2, though they are not yet at goal, they have managed to decrease their risk of microvascular complications by about 20%. The closer to normal the A1c, the lower the absolute risk for microvascular complications.Question 15 |
Which of the following conditions classically presents with Charcot's triad and if left untreated has a mortality rate of almost 100%?
acute acalculous cholecystitis | |
porcelain gallbladder | |
acute cholangitis | |
pigment-stone cholelithiasis | |
choledocholithiasis |
Question 15 Explanation:
Cholangitis is an infection of the biliary tract with the potential to cause significant morbidity and mortality. Many patients with acute cholangitis respond to antibiotic therapy; however, patients with severe or toxic cholangitis may not respond and may require emergency biliary drainage. Jean M. Charcot recognized this illness in 1877 when he described a triad of fever, jaundice, and right upper quadrant pain. In 1959, Reynolds and Dargon described a more severe form of the illness that included the additional components of septic shock and mental confusion, which is referred to as the Reynolds pentad.
Learn More
Question 16 |
The vaginal mucosa may appear cyanotic in early pregnancy. This bluish discoloration is referred to as:
Hegar's sign | |
Cullen's sign. | |
Chadwick's sign. | |
Frank-Turner sign. | |
Kehr's sign. |
Question 16 Explanation:
 Chadwick's sign is a bluish discoloration of the cervix, vagina, and labia resulting from increased blood flow. It is considered an indication of pregnancy, and can be observed as early as 6–8 weeks after conception, and its presence is an early sign of pregnancy.
These color changes were discovered in approximately 1836 by French doctor Étienne Joseph Jacquemin (1796-1872), and are named after James Read Chadwick, who drew attention to it in a paper read before the American Gynecological Society in 1886 and published in the following year, wherein he credited Jacquemin for their discovery.
Chadwick's sign is a bluish discoloration of the cervix, vagina, and labia resulting from increased blood flow. It is considered an indication of pregnancy, and can be observed as early as 6–8 weeks after conception, and its presence is an early sign of pregnancy.
These color changes were discovered in approximately 1836 by French doctor Étienne Joseph Jacquemin (1796-1872), and are named after James Read Chadwick, who drew attention to it in a paper read before the American Gynecological Society in 1886 and published in the following year, wherein he credited Jacquemin for their discovery.Question 17 |
Which of the following arrhythmia's is most commonly associated with Adam-Stokes syncope?
AV block - first degree | |
AV block - second degree; Mobitz type I | |
AV block - second degree; Mobitz type II | |
AV block - third degree | |
Wenekebach phenomenon |
Question 17 Explanation:
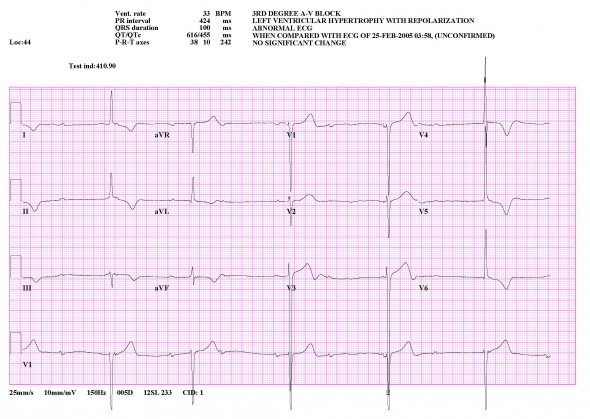 To gain an understanding of pediatric third-degree acquired atrioventricular (AV) block (AVB), one must first understand the concepts behind AV blocks. In general, AV block refers to a conduction delay or interruption of the impulses generated in the atrium before they reach the ventricles. AV block may be transient or permanent, and the anatomic level at which it occurs varies. These features determine the clinical significance of this condition, which may range from minimal to severely symptomatic, including Stokes-Adams syncope, congestive heart failure, or sudden death.
To gain an understanding of pediatric third-degree acquired atrioventricular (AV) block (AVB), one must first understand the concepts behind AV blocks. In general, AV block refers to a conduction delay or interruption of the impulses generated in the atrium before they reach the ventricles. AV block may be transient or permanent, and the anatomic level at which it occurs varies. These features determine the clinical significance of this condition, which may range from minimal to severely symptomatic, including Stokes-Adams syncope, congestive heart failure, or sudden death.Question 18 |
The agent used to treat gout that reduces the production of uric acid is:
probenecid Hint: Probenecid (Lannett's Probalan) is a uricosuric drug that increases uric acid excretion in the urine | |
colchicine Hint: Although colchicine was once the treatment of choice for acute gout, it is now less commonly used than NSAIDs because of its narrow therapeutic window and risk of toxicity. To be effective, colchicine therapy is ideally initiated within 36 hours of onset of the acute attack. When used for acute gout in classic hourly dosing regimens (no longer recommended), colchicine causes adverse GI effects, particularly diarrhea and vomiting, in 80% of patients. | |
allopurinol | |
sulfinpyrazone. | |
theophylline. |
Question 18 Explanation:
Allopurinol blocks xanthine oxidase and thus reduces the generation of uric acid. Approximately 3-10% of patients taking allopurinol develop symptoms of intolerance, such as dyspepsia, headache, diarrhea, or pruritic maculopapular rash.
Question 19 |
You decide that a patient's blood pressure warrants a diagnosis of hypertension. He is a healthy 36 year-old male with no medical history or risk factors for coronary artery disease. Which of the following tests is NOT recommended as baseline testing in the evaluation of such a patient?
serum sodium, potassium, chloride and bicarbonate | |
urinalysis | |
serum creatinine | |
serum glucose | |
plasma rennin |
Question 19 Explanation:
Plasma renin activity (PRA), also known as the renin (active) assay or random plasma renin, is a measure of the activity of the plasma enzyme renin, which plays a major role in the body's regulation of blood pressure, thirst, and urine output. PRA is sometimes measured, specially in case of certain diseases which present with hypertension or hypotension. This is not recommended as a baseline test for our patient above.
Question 20 |
A patient presents with vertigo. Which of the following characteristics is most suggestive of a peripheral etiology?
invoked nystagmus that lasts loner than 60 seconds | |
the absence of nausea | |
the absence of vomiting | |
a hearing loss. | |
the absence of tinnitus |
Question 20 Explanation:
Dizziness and vertigo are common clinical complaints. Vertigo is caused by a disturbed vestibular system and is subdivided into peripheral vertigo (due to failure of the end organs) or central vertigo (due to failure of the vestibular nerves or central connections to the brainstem and cerebellum).
Question 21 |
A patient with recurrent kidney stones wishes to minimize the likelihood of future events. Which of the following is the best advice to reduce the chance of another occurrence?
increase protein while restricting sodium in the diet | |
increase sodium while restricting protein in the diet | |
institute a low fat diet | |
institute a low carbohydrate diet | |
institute a low sodium and low protein diet |
Question 21 Explanation:
In almost all patients in whom stones form, an increase in fluid intake and, therefore, an increase in urine output is recommended. This is likely the single most important aspect of stone prophylaxis. Patients with recurrent nephrolithiasis traditionally have been instructed to drink 8 glasses of fluid daily to maintain adequate hydration and decrease chance of urinary supersaturation with stone-forming salts. The goal is a total urine volume in 24 hours in excess of 2 liters.
The only other general dietary guidelines are to avoid excessive salt and protein intake. Moderation of calcium and oxalate intake is also reasonable, but great care must be taken not to indiscriminately instruct the patient to reduce calcium intake.
Dietary calcium should not be restricted beyond normal unless specifically indicated based on 24-hour urinalysis findings. Urinary calcium levels are normal in many patients with calcium stones. Reducing dietary calcium in these patients may actually worsen their stone disease, because more oxalate is absorbed from the GI tract in the absence of sufficient intestinal calcium to bind with it. This results in a net increase in oxalate absorption and hyperoxaluria, which tends to increase new kidney stone formation in patients with calcium oxalate calculi.
An empiric restriction of dietary calcium may also adversely affect bone mineralization and may have osteoporosis implications, especially in women. This practice should be condemned unless indicated based on a metabolic evaluation.
As a rule, dietary calcium should be restricted to 600-800 mg/d in patients with diet-responsive hypercalciuria who form calcium stones. This is roughly equivalent to a single high-calcium or dairy meal per day.
Learn More
Question 22 |
The risk of extrapyramidal side effects (pseudoparkinsonism) and tardive dyskinesia is associated with which class of medications?
Amphetamines | |
Benzodiazepines | |
Monoamine oxidase inhibitors (MAOIs) | |
Tricyclic antidepressants (TCAs) | |
Typical (first-generation) antipsychotics |
Question 22 Explanation:
Typical antipsychotics (e.g., haloperidol, chlorpromazine, fluphenazine) can produce extrapyramidal symptoms (EPS) via blockade of dopamine (D2) receptors in the nigrostriatum. Symptoms can include akinesia, bradykinesia, mask-like facial expression, tremor, cogwheel rigidity, and postural abnormalities. Tardive dyskinesia may also occur.
Question 23 |
A 5 year-old has a large forehead, a broad nasal bridge, wide-spaced eyes, small, low-set ears and a broad protruding tongue. You also note short broad hands with a curvature of the fifth finger. On ophthalmic examination, you note Brushfield spots. Which of the following is the most likely diagnosis?
Kleinfelter's syndrome | |
Turner's syndrome | |
Fragile X syndrome | |
Down's syndrome | |
Cri du chat syndrome |
Question 23 Explanation:
 Down syndrome is by far the most common and best known chromosomal disorder in humans and the most common cause of intellectual disability. It is primarily caused by trisomy of chromosome 21, which gives rise to multiple systemic complications as part of the syndrome. However, not all defects occur in each patient; there is a wide range of phenotypic variation.
Down syndrome is by far the most common and best known chromosomal disorder in humans and the most common cause of intellectual disability. It is primarily caused by trisomy of chromosome 21, which gives rise to multiple systemic complications as part of the syndrome. However, not all defects occur in each patient; there is a wide range of phenotypic variation.Question 24 |
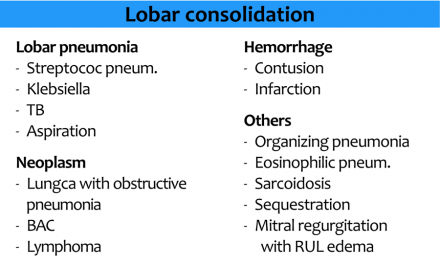
You overhear the cardiology interns discussing an EKG that demonstrates "electrical alternans." They cannot determine the etiology for this phenomenon. You offer assistance and advise them that a common etiology for this EKG pattern is:
a right sided pneumothorax. | |
a left-sided pneumothorax. | |
mitral stenosis. | |
a subarachnoid hemorrhage. | |
a pericardial effusion. |
Question 25 |
A patient driving cross-country experiences an automotive mishap. He spends one night at a farmhouse. During the night, he experiences the abrupt onset of a fever, cough and shortness of breath. Two days after leaving, he is much better, but presents to your office for an opinion. The examination and a chest x-ray are normal. The next day, the patient is asymptomatic. What was the most likely cause?
Blastomycosis | |
spontaneous pneumothorax | |
Goodpasture syndrome | |
pneumonitis | |
Mycobacterium infection |
Question 25 Explanation:
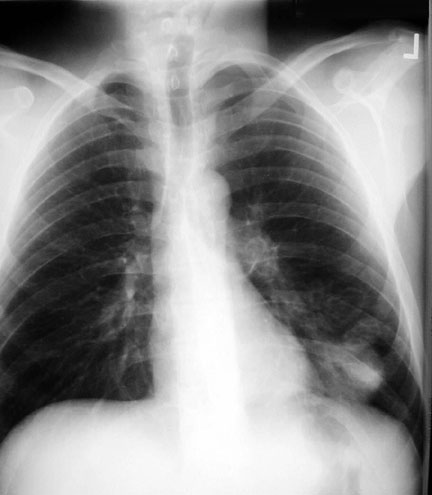 Blastomycosis is a common infection among dogs in endemic areas. It may serve as an indicator of human disease because of the shared environment. Blastomycosis is reported in other animals, including the horse, cow, cat, bat, and lion.
Chest radiograph from a patient with pulmonary blastomycosis demonstrates multiple nodular lesions, some of which are cavitating, in the left lower lobe. Cavitation occurs in 15-20% of patients with blastomycosis.
Blastomycosis is a common infection among dogs in endemic areas. It may serve as an indicator of human disease because of the shared environment. Blastomycosis is reported in other animals, including the horse, cow, cat, bat, and lion.
Chest radiograph from a patient with pulmonary blastomycosis demonstrates multiple nodular lesions, some of which are cavitating, in the left lower lobe. Cavitation occurs in 15-20% of patients with blastomycosis.Question 26 |
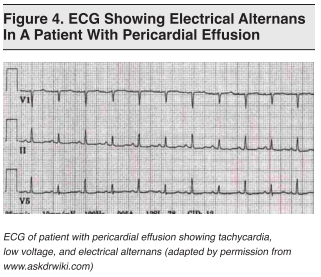
Approximately two weeks after you prescribed a course of beta-lactam antibiotics to a patient, she returns complaining of severs and diffuse arthralgias. Which of the following is most likely responsible for her poly-arthralgias?
Type I allergic reaction | |
Type II allergic reaction | |
Type III allergic reaction. | |
Type IV allergic reaction | |
Type V allergic reaction |
Question 27 |
What is the pathognomonic feature of multifocal atrial tachycardia on an EKG?
heart rate > 200 | |
left axis deviation | |
amplitude of QRS complexes | |
greater than three different P waves with varying PR intervals | |
depression of the PR intervals in leads II, III and a VF only |
Question 27 Explanation:
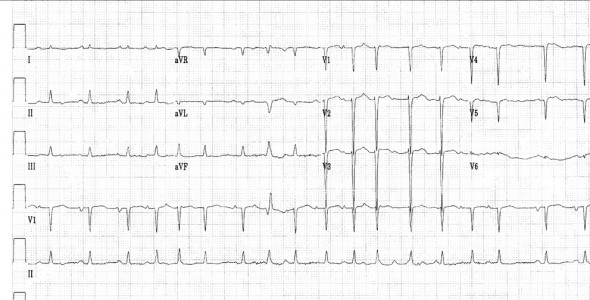 Multifocal atrial tachycardia (MAT) is a cardiac arrhythmia caused by multiple sites of competing atrial activity. It is characterized by an irregular atrial rate greater than 100 beats per minute (bpm). Atrial activity is well organized, with at least 3 morphologically distinct P waves, irregular P-P intervals, and an isoelectric baseline between the P waves.
Learn More
Multifocal atrial tachycardia (MAT) is a cardiac arrhythmia caused by multiple sites of competing atrial activity. It is characterized by an irregular atrial rate greater than 100 beats per minute (bpm). Atrial activity is well organized, with at least 3 morphologically distinct P waves, irregular P-P intervals, and an isoelectric baseline between the P waves.
Learn MoreQuestion 28 |
A newborn infant demonstrates hypoplasia of the distal phalanges, small nails, a flat nasal bridge and a cleft palate. Which of the following agents is likely responsible for these classic findings?
warfarin | |
phenytoin | |
alcohol | |
thalidomide | |
a retinoid |
Question 28 Explanation:
Fetal warfarin syndrome (Dysmorphism due to warfarin, Warfarin embryopathy ) is a condition associated with the administration of Warfarin during pregnancy.
Associated conditions include hypoplasia of nasal bridge, laryngomalacia, pectus carinatum, congenital heart defects, ventriculomegaly, agenesis of the corpus callosum, stippled epiphyses, telebrachydactyly, and growth retardation.
It is also known as "DiSala syndrome". The symptoms are as follows:
- Nasal hypoplasia
- Depressed nasal bridge
- Deep groove between the nostril and nasal tip
- Stippling of uncalcified epiphyses during the first year
- Mild hypoplasia of nails
- Shortened fingers
- Low birth weight
- Significant mental retardation
- Seizures
- Reduced muscle tone
- Widely spaced nipples
- Deafness
- Feeding difficulty
- Failure to thrive
Question 29 |
A 34 year-old female presents to the office complaining that one of her pupils is small and irregular. During her examination, you note that the pupil does not respond to direct or consensual light stimuli. It does, however, become smaller during accommodation testing. What is the most likely diagnosis?
syphilis | |
internal carotid stenosis on the ipsilateral side | |
internal carotid stenosis on the contralateral side | |
hyponatremia | |
hypernatremia |
Question 29 Explanation:
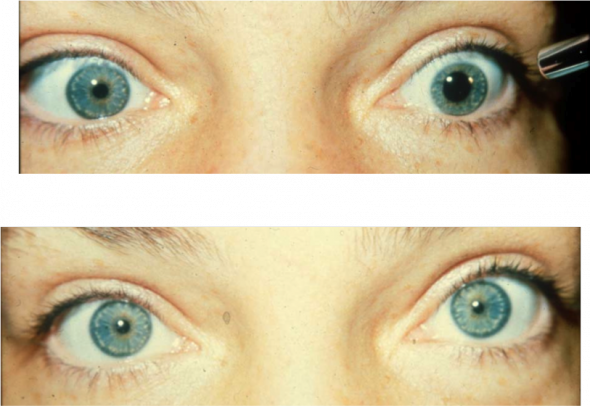 Argyll Robertson pupils (“AR pupils” or colloquially as"Prostitute's Pupil") are bilateral small pupils that reduce in size when the patient focuses on a near object (they “accommodate”), but do not constrict when exposed to bright light (they do not “react” to light). They are a highly specific sign of neurosyphilis, and might also be a sign of diabetic neuropathy.
Argyll Robertson pupils (“AR pupils” or colloquially as"Prostitute's Pupil") are bilateral small pupils that reduce in size when the patient focuses on a near object (they “accommodate”), but do not constrict when exposed to bright light (they do not “react” to light). They are a highly specific sign of neurosyphilis, and might also be a sign of diabetic neuropathy.
Question 30 |
At a blood level of 60 micrograms per milliliter, four of the following agents will be in a toxic range. Which of the following anticonvulsant medications will be in the therapeutic range?
Phenytoin Hint: The total phenytoin reference range varies by age, as follows:
Children and adults: 10-20 µg/mL
Neonates: 8-15 µg/mL
Toxic phenytoin levels are defined as greater than 30 µg/mL.
Lethal levels are defined as greater than 100 µg/m | |
carbarmazepine Hint: The therapeutic reference range of carbamazepine is 4-12 mg/L.
The minimum toxic level is 10 mg/kg.
The toxic concentration/critical laboratory value is greater than 30-40 mg/L. | |
valproic acid | |
Phenobarbital Hint: The therapeutic reference range of phenobarbital varies by age, as follows:
Infants and children (< 5 years): 15-30 µg/mL
Adults: 15-40 µg/mL
The minimum toxic level is 30 µg/mL. | |
primidone |
Question 30 Explanation:
The therapeutic range for valproic acid (total) is 50-125 µg/mL. The toxic level is greater than 150 µg/mL.
Question 31 |
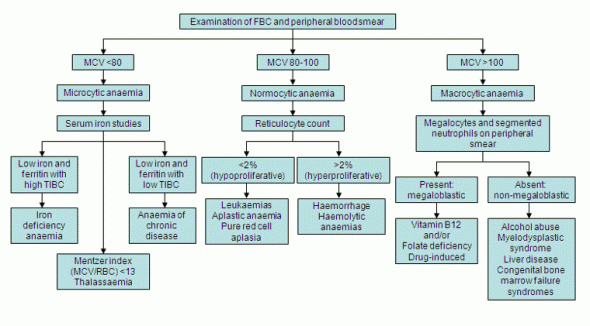
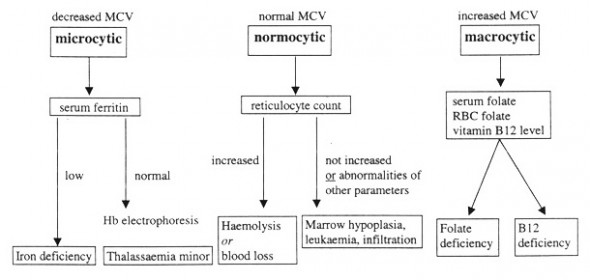
Which of the following would most likely be diagnosed in a patient that has an MCV of 106 fl?
iron deficiency | |
thalassemia | |
sideroblastic anemia | |
anemia of chronic renal failure | |
Viitamin B12 deficiency |
Question 32 |
A 46 year-old female has complained of increasing episodes of "crushing chest pain that awakens her during the night." Which of the following agents will likely be administered to her during the coronary angiogram she has scheduled?
propranolol | |
verapamil | |
nitroglycerin | |
ergonovine | |
lidocaine |
Question 32 Explanation:
This is Prinzmetal's Angina
Prinzmetal's angina should be suspected any time a person has severe chest pain accompanied by dramatic ECG changes, but a cardiac catheterization shows apparently normal coronary arteries.
Once the diagnosis is suspected, the cardiologist usually performs what is called "provocative testing," to show whether coronary artery spasm can be induced. If so, Prinzmetal's angina can be definitively diagnosed. Two types of "provocation" are often used to attempt to induce coronary artery spasm - hyperventilation, and ergonovine.
Question 33 |
You are evaluating a patient with cirrhosis. Which of the following laboratory values is most suggestive of a defect in liver synthetic function?
urine positive for bilirubin | |
elevated serum AST level | |
prolonged INR | |
elevated total bilirubin | |
elevated direct bilirubin |
Question 33 Explanation:
Clotting is the end result of a complex series of enzymatic reactions involving clotting factors, all of which are produced in the liver except factor VIII, which is produced by vascular endothelial cells.
The prothrombin time is a measure of the rate at which prothrombin is converted to thrombin, reflecting the extrinsic pathway of coagulation. Factors involved in the synthesis of prothrombin include II, V, VII, and X
Measurement of the prothrombin time in patients with liver disease is most useful in cases of acute liver disease. Unlike the serum albumin, the prothrombin time allows an assessment of current hepatic synthetic function; factor VII has the shortest serum half-life (six hours) of all the clotting factors.
Question 34 |
During the first year of "typical" use, which method of contraception is LEAST effective?
intrauterine devices | |
oral contraceptives | |
implanon | |
condoms | |
diaphragms |
Question 34 Explanation:
Effectiveness figures are based on 100 couples using the method for a year and show the percentage of women who do not get pregnant while using the method for 1 year.
| METHOD | USE EFFECTIVENESS (Actual Use) | THEORETICAL EFFECTIVENESS (Perfect Use) |
|---|---|---|
| EVRA PATCH | 92% | 99.7% |
| PILL - Combined - Progestin | 92% 92% | 99.7% 99.7% |
| NUVARING | 92% | 99.7% |
| IUD Copper T Levonorgestrel (Mirena) | 99.2% 99.9% | 99.4% 99.9% |
| DIAPHRAGM & SPERMICIDE | 84% | 94% |
| SPERMICIDE & MALE CONDOMS** | no confirmed data | 99% |
| FEMALE CONDOM ALONE | 79% | 95% |
| MALE CONDOM ALONE | 85% | 98% |
| SPERMICIDES*** | 71% | 82% |
| TUBAL LIGATION | 99.5% | 99.5% |
| VASECTOMY | 99.85% | 99.9% |
| CERVICAL CAP Woman has had children Woman has not had children | 68% 84% | 74% 91% |
| DEPO-PROVERA | 97% | 99.95% |
| SPONGE Woman has had children Woman has not had children | 68% 84% | 80% 91% |
| FERTILITY AWARENESS METHOD | 75% | 95-97% |
| WITHDRAWAL | 73% | 96% |
| NO METHOD (CHANCE) | 15% | 15% |
Question 35 |
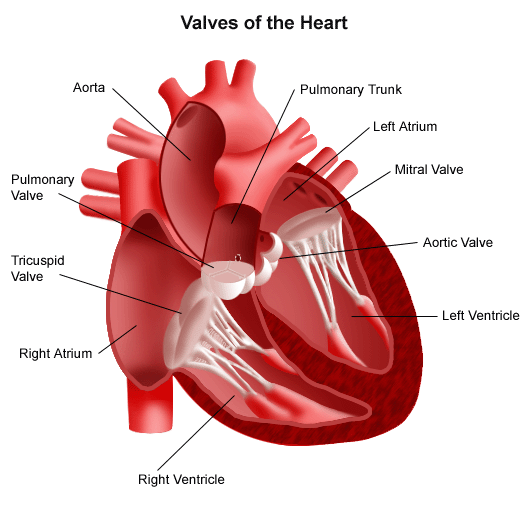
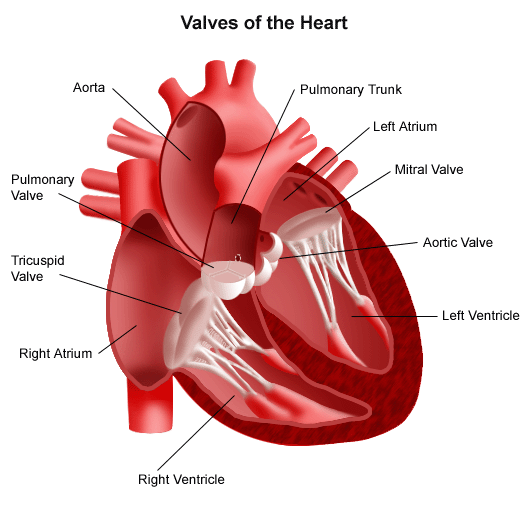
The murmur of mitral stenosis is best auscultated:
with the patient supine, at the apex of the heart. | |
with the patient sitting, at the base of the heart. | |
with the patient lying on the left side, at the apex of the heart | |
with the patient leaning forward, at the base-of the heart. | |
during a valsalva maneuver. |
Question 35 Explanation:
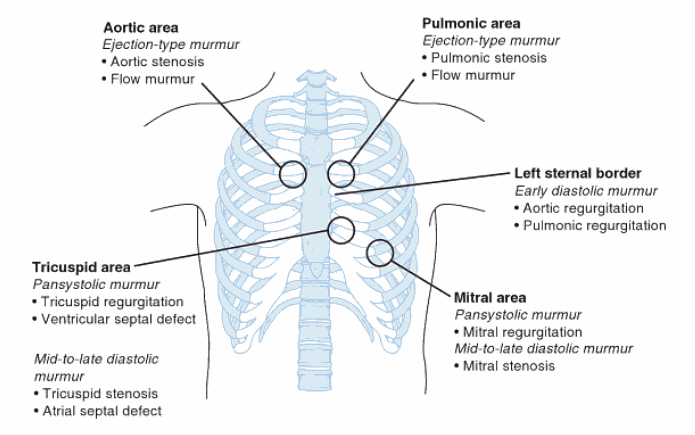 Mitral stenosis (MS) is characterized by obstruction to left ventricular inflow at the level of mitral valve due to structural abnormality of the mitral valve apparatus. The most common cause of mitral stenosis is rheumatic fever. Other less common etiologies include congenital mitral stenosis, malignant carcinoid disease, systemic lupus erythematosus, rheumatoid arthritis, mucopolysaccharidoses of the Hunter-Hurler phenotype, Fabry disease, Whipple disease, and methysergide therapy.
Mitral stenosis (MS) is characterized by obstruction to left ventricular inflow at the level of mitral valve due to structural abnormality of the mitral valve apparatus. The most common cause of mitral stenosis is rheumatic fever. Other less common etiologies include congenital mitral stenosis, malignant carcinoid disease, systemic lupus erythematosus, rheumatoid arthritis, mucopolysaccharidoses of the Hunter-Hurler phenotype, Fabry disease, Whipple disease, and methysergide therapy.Question 36 |
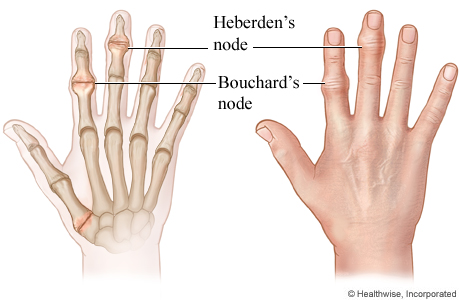
A 78 year-old male presents stating that his last clinician told him he has Heberden's nodes. You tell him that Herbeden's nodes are:
a classic sign of scarlet fever | |
commonly discovered in patients with colon cancer | |
often misdiagnosed as basal cell carcinomas | |
a common finding in patients with osteoarthritis | |
often a precursor to prostatic hypertrophy. |
Question 37 |
Which of the following occupations places the patient at the greatest risk for developing bladder carcinoma?
abattoir worker | |
dentist | |
rubber industry worker | |
gardener | |
ceramics industry worker |
Question 37 Explanation:
Excess deaths from bladder, stomach, lung, hematopoietic, and other cancers have occurred among workers involved in the manufacture of rubber products. These workers may also risk adverse respiratory effects, dermatologic effects, reproductive effects, injuries, and repetitive trauma disorders. The adverse health effects cannot be attributed to a single chemical or group of chemicals because workplace exposures vary greatly and chemical formulations change frequently. Epidemiologic, toxicologic, and industrial hygiene studies are needed to assess the risk of cancer and other adverse health effects for rubber products workers.
Learn More
Question 38 |
A 16-year-old female presents with a two-day history of coughing, productive of small quantities of "yellow phlegm." Her BP is 114/78 mm Hg, heart rate is 84, respiratory rate is 16, and temperature is 99.7"F (orally). Her peak expiratory flow rate is 550 L/min. Her lungs are clear to auscultation. Which of the following is the most appropriate therapeutic recommendation?
ample fluids, rest and acetaminophen as needed | |
penicillin VK 500 mg po BID | |
amoxicillin 500mg po TID | |
azithromycin - 5 day dose pack | |
amantadine 100 mg po BID |
Question 38 Explanation:
This patient has a common viral syndrome. Antibiotics or amantadine are not warranted.
Question 39 |
Six months after "sticking a cotton-tipped applicator" too far into his ear, a 41 year-old male presents for evaluation of persistent hearing loss. During the examination, you note a cholesteatoma. You recommend:
ten days of therapy with second generation cephalosporin. | |
fourteen days of therapy with an otic solution of antimicrobials and acorticosteroid. | |
close observation and follow-up in four weeks. | |
close observation and referral to an otologist for custom-made ear plugs. | |
referral to an otolaryngologist for surgical intervention. |
Question 39 Explanation:
 Cholesteatoma is a destructive and expanding growth consisting of keratinizing squamous epithelium in the middle ear and/or mastoid process. Although these are not strictly speaking tumours or cancers they can still cause significant problems because of their erosive and expansile properties resulting in the destruction of the ossicles as well as their possible spread through the base of the skull into the brain. They are also often infected and result in chronically draining ears.
Cholesteatoma is a destructive and expanding growth consisting of keratinizing squamous epithelium in the middle ear and/or mastoid process. Although these are not strictly speaking tumours or cancers they can still cause significant problems because of their erosive and expansile properties resulting in the destruction of the ossicles as well as their possible spread through the base of the skull into the brain. They are also often infected and result in chronically draining ears.Question 40 |
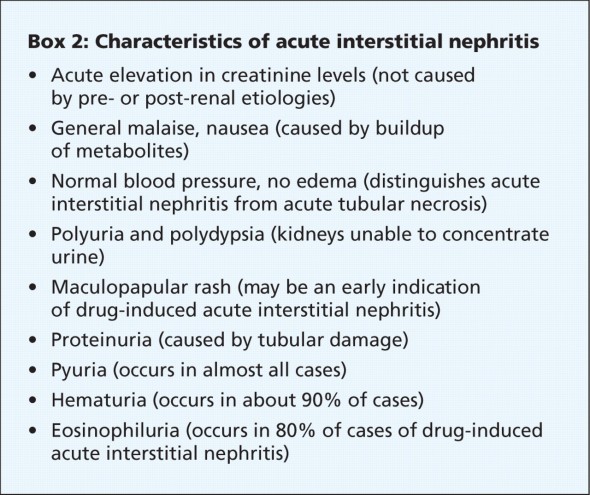
A 22 year-old male presents with a fever, and a maculopapular rash. His serum creatine and BUN are elevated. The urinalysis is significant for hematuria, pyuria, white blood cell casts and eosinophiluria. The most likely diagnosis is
Acute tubular necrosis | |
Diabetic nephropathy | |
Hypertensive nephrosclerosis | |
interstitial nephritis | |
Lupus nephritis |
Question 41 |
The laboratory finding most consistent with a clinical diagnosis of rheumatoid arthritis is:
urate crystals in the joint aspirate. | |
an erythrocyte sedimentation rate <20 mmlhr. | |
a positive rheumatoid factor in the serum | |
synovial fluid with less than 1. 0 WBC's per cubic milliliter on joint fluid analysis. | |
an elevated serum amylase level. |
Question 41 Explanation:
Immunologic parameters include autoantibodies (eg, RF, anti-CCP antibodies, and ANAs). RF is an immunoglobulin (Ig) M antibody directed against the Fc fragment of IgG that is present in approximately 60-80% of patients with RA over the course of their disease (but in fewer than 40% of patients with early RA). RF values fluctuate somewhat with disease activity, though titers of RF generally remain high even in patients with drug-induced remissions.
RF is not specific for RA but is also present in other connective tissue diseases, infections, and autoimmune disorders, as well as in 1-5% of healthy people. The presence of RF predicts radiographic progression of bone erosions, independent of disease activity.
Learn More
Question 42 |
A newborn infant begins vomiting within hours of birth. You note progressive distention of the abdomen. An abdominal X-RAY demonstrates a "double-bubble" gas shadow. What is the most likely diagnosis?
an elevated serum amylase level. | |
congenital megacolon | |
esophageal atresia | |
duodenal atresia | |
tracheoesophageal fistula |
Question 42 Explanation:
 Duodenal atresia is the congenital absence or complete closure of a portion of the lumen of the duodenum. It causes increased levels of amniotic fluid during pregnancy (polyhydramnios) and intestinal obstruction in newborn babies. Radiography shows a distended stomach and distended duodenum, which are separated by the pyloric valve, a finding described as the "double-bubble sign."
Duodenal atresia is the congenital absence or complete closure of a portion of the lumen of the duodenum. It causes increased levels of amniotic fluid during pregnancy (polyhydramnios) and intestinal obstruction in newborn babies. Radiography shows a distended stomach and distended duodenum, which are separated by the pyloric valve, a finding described as the "double-bubble sign." 
Question 43 |
In a classic case, the earliest manifestation of mitral valve stenosis is:
orthopnea. | |
angina. | |
palpitations | |
dyspnea on exertion | |
lower extremity swelling |
Question 43 Explanation:
Symptoms of mitral stenosis usually manifest during the third or fourth decade of life and nearly half of the patients do not recall a history of acute rheumatic fever.
Patients are generally asymptomatic at rest during the early stage of the disease. However, factors that increase heart rate such as fever, severe anemia, thyrotoxicosis, exercise, excitement, pregnancy, and atrial fibrillation may result in dyspnea.
Nearly 15% of patients develop embolic episodes that are usually associated with atrial fibrillation. Rarely, embolic episodes may occur even in the patient with sinus rhythm. Systemic embolization may lead to stroke, renal failure, or myocardial infarction.
Hoarseness can develop from compression of the left recurrent laryngeal nerve against the pulmonary artery by the enlarged left atrium. Also, compression of bronchi by the enlarged left atrium can cause persistent cough.
Hemoptysis may occur and is usually not fatal.
Pregnant women with mild mitral stenosis may become symptomatic during their second trimester because of the increase in blood volume and cardiac output.
Learn More
Question 44 |
A 28 year-old African-American presents to your facility for an evaluation of a nonproductive cough and mild dyspnea. A chest x-ray demonstrates a right hilar "mass." A pulmonologist consults and performs a biopsy during a bronchoscopy. The report reveals that the mass is a noncaseating granuloma. Which of the following therapeutics do you prescribe?
cisplatin | |
radiation | |
amphotericin B | |
inhaled beta agonists | |
corticosteroids |
Question 44 Explanation:
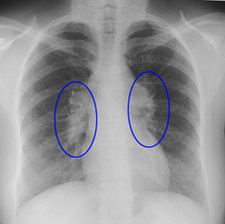 Sarcoidosis is a multisystem inflammatory disease of unknown etiology that manifests as noncaseating granulomas, predominantly in the lungs and intrathoracic lymph nodes. The age-adjusted incidence is 11 cases per 100,000 population in whites but 34 cases per 100,000 population in African Americans. Corticosteroids are the mainstay of therapy.
Generally, prednisone given daily and then tapered over a 6-month course is adequate for pulmonary disease. Earlier recommendations suggested an initial dose of 1 mg/kg/d of prednisone; however, more recent expert opinions endorse a lower dose (eg, 40 mg/d), which is tapered to every-other-day long-term therapy over several weeks. In one study, treatment of acute exacerbations of pulmonary sarcoidosis with steroid doses as low as 20 mg of prednisone for a median of 21 days improved spirometry back to baseline and improved clinical symptoms.
Sarcoidosis is a multisystem inflammatory disease of unknown etiology that manifests as noncaseating granulomas, predominantly in the lungs and intrathoracic lymph nodes. The age-adjusted incidence is 11 cases per 100,000 population in whites but 34 cases per 100,000 population in African Americans. Corticosteroids are the mainstay of therapy.
Generally, prednisone given daily and then tapered over a 6-month course is adequate for pulmonary disease. Earlier recommendations suggested an initial dose of 1 mg/kg/d of prednisone; however, more recent expert opinions endorse a lower dose (eg, 40 mg/d), which is tapered to every-other-day long-term therapy over several weeks. In one study, treatment of acute exacerbations of pulmonary sarcoidosis with steroid doses as low as 20 mg of prednisone for a median of 21 days improved spirometry back to baseline and improved clinical symptoms.Question 45 |
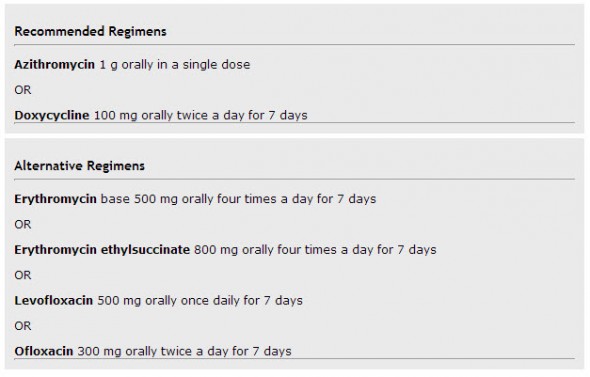
A 19 year old female complains of a mucoid vaginal discharge. A Gram stain identifies several WBC's but no organisms are identified. What treatment is most appropriate?
procaine penicillin IM | |
benzathine penicillin M | |
azithromycin 1 gram orally | |
metronidazole 500 mg BID for 7 days | |
ceftriaxone 125 mg IM |
Question 46 |
All of the following are risk factors for pelvic inflammatory disease (PID) EXCEPT:
multiple sexual partners | |
history of previous PID | |
barrier contraceptive method use | |
intrauterine device use Hint: Pelvic inflammatory disease (PID) concerns have been linked to the IUD for years. But it is now known that the IUD itself does not cause PID. | |
age < 25 years old |
Question 46 Explanation:
Pelvic inflammatory disease (PID) is an infectious and inflammatory disorder of the upper female genital tract, including the uterus, fallopian tubes, and adjacent pelvic structures. There are several risk factors, including previous history of PID, multiple sexual partners, and younger age.
Learn More
Question 47 |
A 23 year-old male complains of intermittent bloody diarrhea. He has noted occasional paroxysms of abdominal discomfort. A lower GI study demonstrates a normal small bowel, but a loss of haustral markings in the colon. What is the most likely diagnosis?
ulcerative colitis | |
Crohn's disease | |
irritable bowel syndrome | |
diverticulosis | |
diverticulitis |
Question 48 |
Which of the following viral infections is LEAST teratogenic in pregnancy?
herpes simplex | |
cytomegalovirus | |
rhinovirus | |
varicella | |
rubella |
Question 49 |
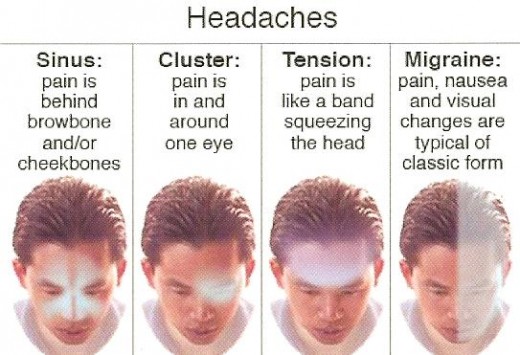
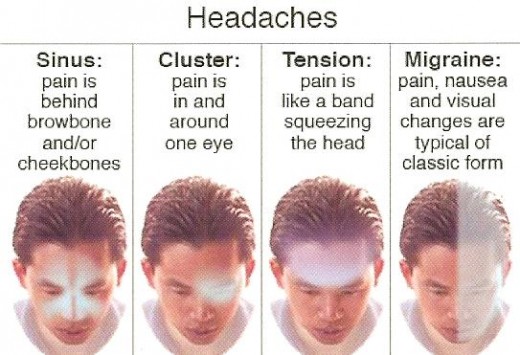
A 23 year-old female describes a history of recurrent headaches, occurring above her left eye. She describes them as "throbbing" in quality. She often suffers from nausea and vomiting. Commonly, after a nap, she awakens feeling better. The headaches usually last a few hours. She experiences the cephalgia about twice a month. What is the most likely diagnosis?
sinusitis | |
intracranial mass | |
migraine | |
muscle contraction | |
cluster |
Question 49 Explanation:
This is the classic presentation of a common migraine headache.
Question 50 |
Which of the following causes of untreated anemia is expected to have the highest reticulocyte count on presentation?
iron deficiency | |
chronic renal disease | |
thalassemia | |
folate deficiency | |
intravascular hemolysis |
Question 51 |
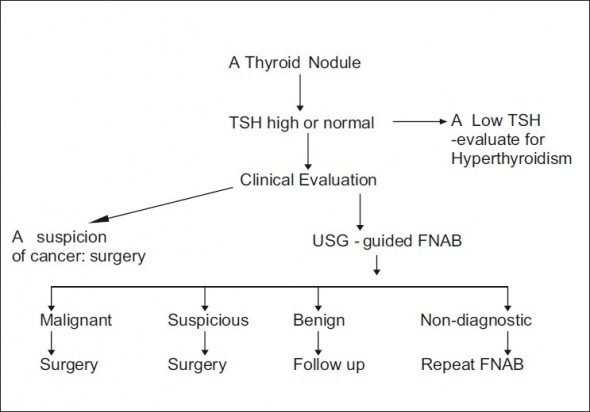
A patient is noted to have a nodular mass in the right lobe of his thyroid gland. His TSH and free T4 levels are normal. Which of the following should be the next steps in his evaluation and management?
thyroid scan - if hot - surgery | |
thyroid scan - if hot - thyroxine therapy | |
thyroid scan - if cold - surgery | |
thyroid scan - if cold - thyroxine therapy | |
fine needle aspiration - treatment based upon results |
Question 52 |
A patient with a history of heavy alcohol use presents complaining that they appear "yellow." Which of the following is least compatible with a diagnosis of alcohol-induced hepatitis?
fever | |
liver tenderness | |
elevated serum bilirubin | |
a history of "light-colored" stools | |
serum AST:ALT < 0.5 |
Question 52 Explanation:
The diagnosis of alcoholic hepatitis is straightforward and requires no further diagnostic studies in patients presenting with a history of alcohol abuse, typical symptoms and physical findings, evidence of liver functional impairment, and compatible liver enzyme levels. In milder cases of alcoholic hepatitis, a mild elevation of the aspartate aminotransferase (AST) level may be the only diagnostic clue.
Learn More
Question 53 |
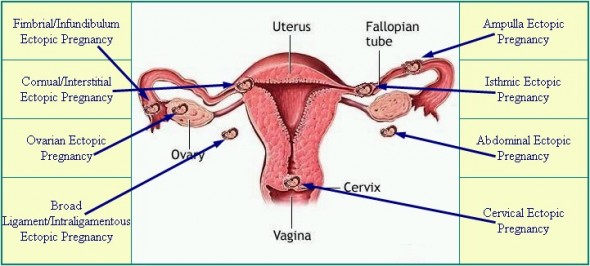
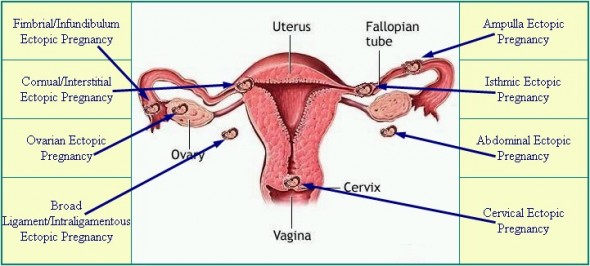
What is the most common site for implantation of an ectopic pregnancy?
cervix | |
ovary | |
peritoneal cavity | |
fallopian tube | |
pelvic interstitial |
Question 53 Explanation:
The classic clinical triad of ectopic pregnancy is pain, amenorrhea, and vaginal bleeding; unfortunately, only about 50% of patients present with all 3 symptoms. About 40-50% of patients with an ectopic pregnancy present with vaginal bleeding, 50% have a palpable adnexal mass, and 75% may have abdominal tenderness.
Question 54 |
What two valves are most commonly involved in cases of rheumatic heart disease?
aortic and pulmonic | |
aortic and mitral | |
aortic and tricuspid | |
pulmonic and tricuspid | |
tricuspid and mitral |
Question 54 Explanation:
Rheumatic heart disease is the most serious complication of rheumatic fever. Acute rheumatic fever follows 0.3% of cases of group A beta-hemolytic streptococcal pharyngitis in children. As many as 39% of patients with acute rheumatic fever may develop varying degrees of pancarditis with associated valve insufficiency, heart failure, pericarditis, and even death. With chronic rheumatic heart disease, patients develop valve stenosis with varying degrees of regurgitation, atrial dilation, arrhythmias, and ventricular dysfunction. Chronic rheumatic heart disease remains the leading cause of mitral valve stenosis and valve replacement in adults in the United States.
Acute rheumatic fever and rheumatic heart disease are thought to result from an autoimmune response, but the exact pathogenesis remains unclear. Although rheumatic heart disease was the leading cause of death 100 years ago in people aged 5-20 years in the United States, incidence of this disease has decreased in developed countries, and the mortality rate has dropped to just above 0% since the 1960s. Worldwide, rheumatic heart disease remains a major health problem. Chronic rheumatic heart disease is estimated to occur in 5-30 million children and young adults; 90,000 individuals die from this disease each year. The mortality rate from this disease remains 1-10%.
Question 55 |
Secondary to a football forcibly flexing a patient's finger, the patient cannot actively extend the digit at the distal interphalangeal joint. What is the most likely diagnosis?
felon | |
subungual hematoma | |
flexor profundus disruption | |
mallet finger | |
flexor superficialis tendon avulsion |
Question 55 Explanation:
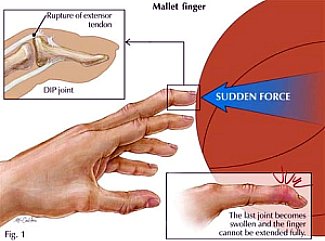 The term mallet finger has long been used to describe the deformity produced by disruption of the terminal extensor mechanism at the distal interphalangeal (DIP) joint. Mallet finger is the most common closed tendon injury that is seen in athletes; this injury is also common in nonathletes after "innocent" trauma. Mallet finger has also been referred to as drop, hammer, or baseball finger (although baseball accounts for only a small percentage of such injuries).
The term mallet finger has long been used to describe the deformity produced by disruption of the terminal extensor mechanism at the distal interphalangeal (DIP) joint. Mallet finger is the most common closed tendon injury that is seen in athletes; this injury is also common in nonathletes after "innocent" trauma. Mallet finger has also been referred to as drop, hammer, or baseball finger (although baseball accounts for only a small percentage of such injuries).Question 56 |
A young female presents with several extremely tender, symmetrical red spots on her lower extremities, distal to the knees. She states she can't sleep with a blanket on her bed, secondary to the discomfort caused when the blanket rubs on her legs. What is the most likely diagnosis?
erythema multiforme | |
erythema nodosum | |
erysipelas | |
pleurodynia | |
diabetes insipidus |
Question 56 Explanation:
 Erythema nodosum (EN) is an acute, nodular, erythematous eruption that usually is limited to the extensor aspects of the lower legs. Chronic or recurrent erythema nodosum is rare but may occur. Erythema nodosum is presumed to be a hypersensitivity reaction and may occur in association with several systemic diseases or drug therapies, or it may be idiopathic. The inflammatory reaction occurs in the panniculus.
Classic presentation of erythema nodosum with nodular red swellings over the shins.
Erythema nodosum (EN) is an acute, nodular, erythematous eruption that usually is limited to the extensor aspects of the lower legs. Chronic or recurrent erythema nodosum is rare but may occur. Erythema nodosum is presumed to be a hypersensitivity reaction and may occur in association with several systemic diseases or drug therapies, or it may be idiopathic. The inflammatory reaction occurs in the panniculus.
Classic presentation of erythema nodosum with nodular red swellings over the shins.Question 57 |
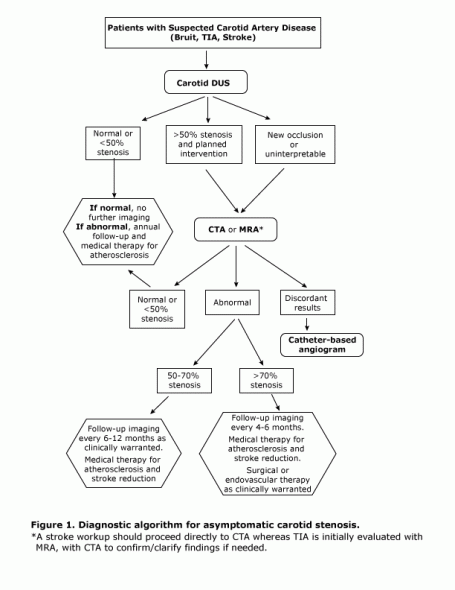
During the annual physical examination of an asymptomatic 72 year-old female, a bruit is auscultated in the left carotid artery. Which of the following is the most appropriate next step in this patient's evaluation?
aortic arch angiogram | |
thyroid ultrasound | |
lipid profile | |
Doppler ultrasound of the carotid arteries | |
schedule a follow-up visit in 6 months |
Question 58 |
All of the following are commonly associated with prerenal renal failure EXEPT:
renal artery stenosis | |
septic shock | |
ureteral stenosis | |
hypovolemia | |
a reduction in the cardiac ejection fraction |
Question 58 Explanation:
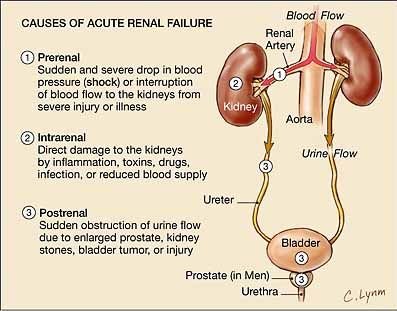 There are five different types of kidney failure:
Acute Prerenal Kidney Failure
This is caused by insufficient blood flow to the kidneys. Without enough blood flow, the kidneys cannot filter toxins from the blood. This type is usually curable by resolving the cause of inadequate blood flow.
Acute Intrinsic Kidney Failure
This can be caused by direct trauma to the kidneys, such as physical impact, accidents, toxin overload, or ischemia (a lack of oxygen to the kidneys). Severe bleeding, shock, renal blood vessel obstruction, or glomerulonephritis (inflammation of the tiny filters in your kidneys) can all cause ischemia.
Chronic Pre-Renal Kidney Failure
When low blood flow to the kidneys is not treated and the condition remains for an extended period of time, chronic pre-renal kidney failure can occur. The kidneys begin to shrink and lose the ability to function.
Chronic Intrinsic Kidney Failure
Damage to the kidneys over an extended period due to intrinsic kidney disease can develop into chronic intrinsic kidney failure.
Chronic Post-Renal Kidney Failure
This happens when a long-term blockage of the urinary tract prevents urinary waste elimination, which causes pressure and eventual kidney damage.
There are five different types of kidney failure:
Acute Prerenal Kidney Failure
This is caused by insufficient blood flow to the kidneys. Without enough blood flow, the kidneys cannot filter toxins from the blood. This type is usually curable by resolving the cause of inadequate blood flow.
Acute Intrinsic Kidney Failure
This can be caused by direct trauma to the kidneys, such as physical impact, accidents, toxin overload, or ischemia (a lack of oxygen to the kidneys). Severe bleeding, shock, renal blood vessel obstruction, or glomerulonephritis (inflammation of the tiny filters in your kidneys) can all cause ischemia.
Chronic Pre-Renal Kidney Failure
When low blood flow to the kidneys is not treated and the condition remains for an extended period of time, chronic pre-renal kidney failure can occur. The kidneys begin to shrink and lose the ability to function.
Chronic Intrinsic Kidney Failure
Damage to the kidneys over an extended period due to intrinsic kidney disease can develop into chronic intrinsic kidney failure.
Chronic Post-Renal Kidney Failure
This happens when a long-term blockage of the urinary tract prevents urinary waste elimination, which causes pressure and eventual kidney damage.Question 59 |
Animal bite wound infections that occur greater than 48 hours after the bite are commonly mixed infections with Staphylococcal and Streptococcal organisms. When the infection develops in less than 48 hours from the time of the bite, the causal agent that should be considered most likely is:
Pasteurella multocida. | |
Pseudomonas species. | |
Clostridial species. | |
Escherichia coli. | |
Bacteroides species. |
Question 59 Explanation:
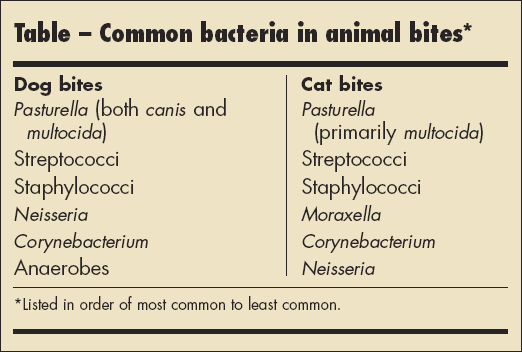 Injuries to the head and neck region have a lower risk of infection than injuries to the extremities. The risk of infection is increased with puncture wounds, treatment delay (6-12 h), and in patients older than 50 years. Likewise, patients who are immunocompromised are at increased risk.
The most common organisms are Staphylococcus species, Streptococcus species, Pasteurella multocida, and anaerobic organisms. When the infection develops in less than 48 hours from the time of the bite think Pasteurella. Most Pasteurella isolates are susceptible to oral antimicrobials such as amoxicillin, amoxicillin/clavulanic acid, minocycline, fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin), and trimethoprim-sulfamethoxazole.
Injuries to the head and neck region have a lower risk of infection than injuries to the extremities. The risk of infection is increased with puncture wounds, treatment delay (6-12 h), and in patients older than 50 years. Likewise, patients who are immunocompromised are at increased risk.
The most common organisms are Staphylococcus species, Streptococcus species, Pasteurella multocida, and anaerobic organisms. When the infection develops in less than 48 hours from the time of the bite think Pasteurella. Most Pasteurella isolates are susceptible to oral antimicrobials such as amoxicillin, amoxicillin/clavulanic acid, minocycline, fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin), and trimethoprim-sulfamethoxazole.Question 60 |
A 38 year-old male complains of a three-week history of daily headaches that awaken him from sleep. The headaches occur around the right eye. He notes that the right eye waters and his right nostril gets stuffy with each headache. you suspect:
a subarachnoid hemorrhage. | |
central serous choroidopathy. | |
cluster headaches. | |
a lacunar cerebrovascular infarction. | |
normal pressure hydrocephalus. |
Question 60 Explanation:
Cluster headache (CH), also known as histamine headache, is a primary neurovascular primary headache disorder, the pathophysiology and etiology of which are not well understood. As the name suggests, CH involves a grouping of headaches, usually over a period of several weeks. According to the diagnostic criteria developed by the International Headache Society (IHS), CH has the following characteristics:
The patient experiences attacks of severe or very severe, strictly unilateral pain (orbital, supraorbital, or temporal pain) that last 15-180 minutes and occur from once every other day to 8 times a day.
The attacks are associated with 1 or more of the following (all ipsilateral): conjunctival injection, lacrimation, nasal congestion, rhinorrhea, forehead and facial sweating, miosis, ptosis, or eyelid edema.
Once you are finished, click the button below. Any items you have not completed will be marked incorrect.
There are 60 questions to complete.
|
List |