Neoplasms of the breast and reproductive tract (PEARLS)
| Breast Cancer |
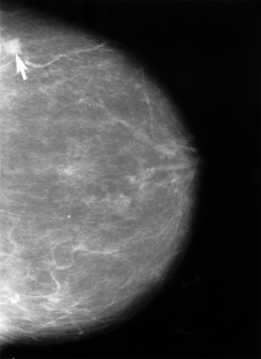
Patient will present as → a 66-year-old female with concern over a mass she felt in her left breast on recent breast self-examination. She denies any nipple discharge and reports a negative family history of breast or other cancers. Physical examination confirms the presence of a painless, firm, irregular, and immobile lump in the superolateral quadrant of the left breast; there are no evident overlying skin changes, and there is no notable axillary lymphadenopathy on palpation. A mammogram is performed, with results seen here. Breast Cancer is the most common malignancy in women
- Risk factors (increased exposure to estrogen):
- Menarche before age 12
- Advanced maternal age of first full-term pregnancy, no pregnancies
- Menopause after age 52
- Breast mass- immobile, irregular
- Nipple retraction, bloody nipple discharge
The most common type is infiltrating intraductal carcinoma (IIC) 80%
- Infiltrating lobular (10%) frequently bilateral
- Paget's disease of the nipple (1%) chronic eczematous itchy, scaling rash on the nipples and areola
- Inflammatory breast cancer (2%) red swollen, warm and itchy breast often with nipple retraction and peau d'orange (NO LUMP)
Tumors may be Estrogen receptor (ER) positive 75%, Progesterone receptor (PR) positive 65% as well as HER2 positive 25%
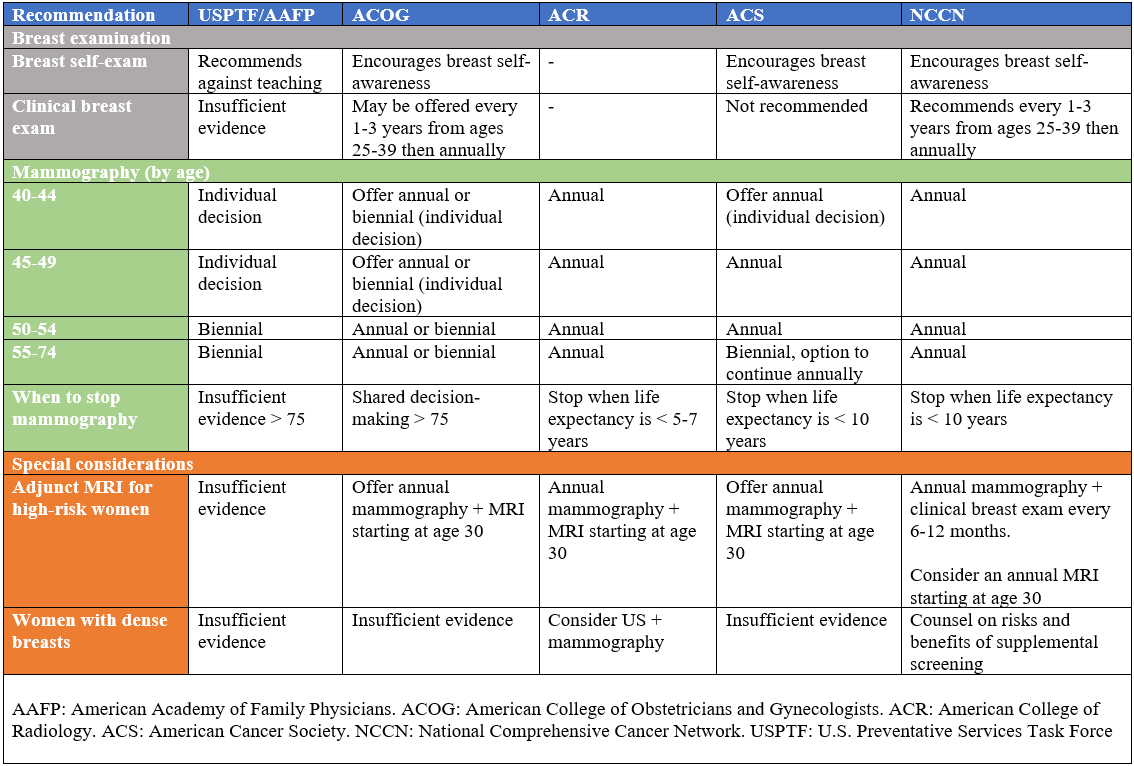
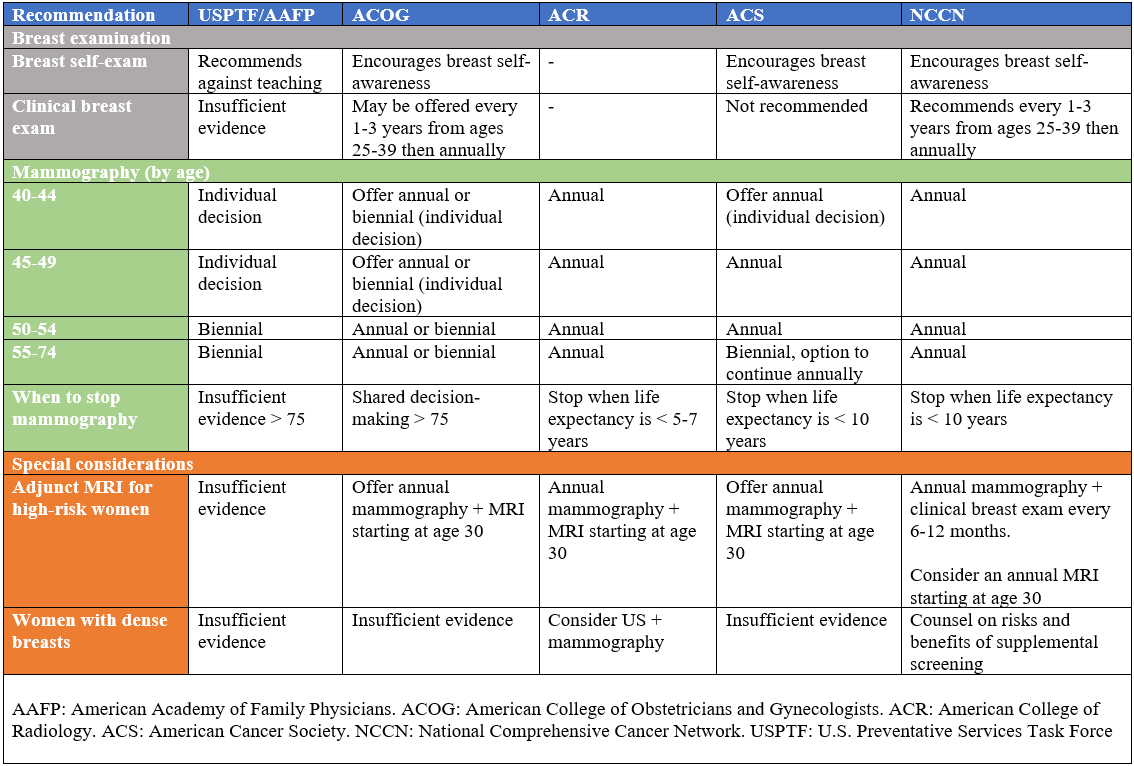
Average risk breast cancer screening guidelines:
Risk calculators for the average woman include:
TX:
- Segmental mastectomy (lumpectomy) followed by breast irradiation in all patients and adjunctive chemotherapy in women with positive nodes stage I and stage II with tumors less than 4 cm in diameter
- Anti-estrogen Tamoxifen is useful in tumors that are ER-positive – binds and blocks the estrogen receptor in the breast tissue
- Aromatase inhibitors are useful in postmenopausal ER-positive patients with breast cancer – reduces the production of estrogen
- Monoclonal AB treatment is useful in patients with HER2 positivity (Human Epidermal Growth Factor Receptor)
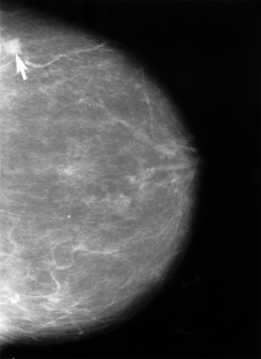 Mammogram showing breast cancer |
| Cervical cancer |
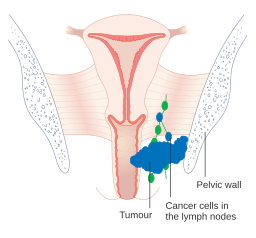
Patient will present as → a 45-year-old female with post-coital bleeding and painful intercourse. On exam, you notice a friable, bleeding cervical lesion. The cytological evaluation shows a high-grade squamous intraepithelial lesion (HSIL/CIN2/3). She is referred for colposcopy and directed biopsies. What clinical triad is strongly indicative of cervical cancer extension to the pelvic wall? Unilateral leg edema, sciatic pain, ureteral obstruction Cervical cancer is the third most common type of cancer
- Up to 80% of patients present with abnormal vaginal bleeding, most commonly postmenopausal
- Only 10% note postcoital bleeding
- Less frequent symptoms include vaginal discharge and pain
- 80% are squamous cells and arise from the squamocolumnar junction of the cervix (transformational zone)
- Risk factors for carcinoma of the cervix ⇒ Multiple sexual partners, early age at first intercourse, early first pregnancy, and HPV positive
- HPV is 99% of the reason for cervical cancer, types that cause cancer are 16,18,31 and 33. Especially types 16, 18
- Associated with cigarette smoking
USPSTF guidelines for cervical cancer screening
- Screening for cervical cancer every 3 years with cervical cytology alone in women aged 21 to 29 years
- For women aged 30 to 65 years, the USPSTF recommends screening every 3 years with cervical cytology alone, every 5 years with high-risk human papillomavirus (hrHPV) testing alone, or every 5 years with hrHPV testing in combination with cytology (cotesting)
- Do not screen women younger than 21 years
- Do not screen women who have had a hysterectomy with removal of the cervix and do not have a history of a high-grade precancerous lesion (ie, cervical intraepithelial neoplasia [CIN] grade 2 or 3) or cervical cancer
- Do not screen women > 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer
DX: Friable, bleeding cervical lesion on exam
- Biopsy of gross lesions and colposcopically directed biopsies are the definitive means of diagnosis
- The majority of cases (80%) are invasive squamous cell types usually arising from the ectocervix
TX: Resect and/or chemotherapy and radiation
- Stage 1: conservative, simple, or radical hysterectomy
- Stage 2 +: chemo +/– radiation
- 5-y survival– Stage 1: 85%-90% Stage 2: 65% Stage 3: 29% Stage 4: 21%
 Adenocarcinoma of the cervix |
| Ovarian Cancer |
Patient will present as → a 66-year-old woman who complains of abdominal fullness, bloating, fatigue, and weight loss. She underwent menopause 17 years ago and has never had children. She had a pelvic mass but her PAP smear is atrophic. CA-125 levels are elevated. A transvaginal ultrasound demonstrates an ovarian mass concerning for malignancy. Ovarian cancer is the second most common type of GYN cancer in women (the first is endometrial cancer)
- Population: 40-60 years of age, ascites, abdominal pain ⇒ 75% diagnosed at an advanced stage
- If a woman has ascites ovarian cancer is the most likely tumor to be found
- Protective factors for the risk of ovarian cancer include multiparity, OCP use, and breast-feeding
- Use of oral contraceptives: 5 years of use decreases risk by 20%; 15 years by 50%
- Risk factors: nulligravidity (or infertility), early menarche, late menopause, endometriosis
- 90% are epithelial tumors ⇒ germ cell tumors are more common in patients < 10 years old
DX: Diagnose with transvaginal ultrasound, then biopsy
- Serum tumor marker CA-125 ⇒ BRCA1 gene is associated with 5% of cases
TX: Stage 1A or 1B—Surgical excision alone (abdominal hysterectomy and bilateral salpingo-oophorectomy)
- Other stages—Surgical resection followed by adjuvant chemotherapy or radiation
- Monitor CA-125 afterward to assess disease progress
|
| Endometrial cancer |
Patient will present as → a 53-year-old woman with no period for four years and is now having abnormal bleeding and bleeding after intercourse. She has lower abdominal pain, pelvic heaviness, and bloating, and feels as though she may have her menses. A transvaginal ultrasound shows endometrial thickness of 12 mm. An endometrial biopsy is performed and confirms endometrial adenocarcinoma. Endometrial cancer is the most common GYN malignancy and the fourth most common malignancy in women in the US
- The cardinal symptom is postmenopausal vaginal bleeding ⇒ One-third of women with postmenopausal bleeding have endometrial CA
- Bleeding in postmenopausal women is CA until proven otherwise
- Most often adenocarcinoma
- Risk factors for endometrial cancer: Obesity, nulliparity, early menarche, late menopause, unopposed estrogen stimulation, hypertension, gallbladder disease, DM, prior ovarian, endometrial, or breast cancer
- 50% of women with endometrial cancer will have an abnormal PAP smear
Diagnosis: Endometrial biopsy is the gold standard definitive diagnostic test
- Endometrial biopsy is indicated in all postmenopausal women vaginal bleeding
TX: Usually total hysterectomy and bilateral salpingo-oophorectomy, pelvic radiation therapy with or without chemotherapy for stage II or III cancer

|
| Vaginal and Vulvar cancer |
Patient will present as → a 65-year-old African American woman, gravida 4, para 4, with a smoking history and past HPV infection, presents with 3 months of postmenopausal vaginal bleeding, pelvic pain, and dyspareunia. She states that the bleeding is usually light and intermittent but has recently increased in frequency and volume. She hasn’t had a Pap smear in over a decade. On examination, a 2cm firm, irregular mass is found on the anterior vaginal wall. Biopsy reveals poorly differentiated squamous cell carcinoma and CT scan indicates local invasion into the bladder wall. (vaginal neoplasms)
Patient will present as → a 50-year-old female with vaginal itching and irritation red/white ulcerative crusted lesions on the vulva (vulvar cancer)
What are the known risk factors for vulvar/vaginal carcinoma? HPV infection, Smoking, Coexisting cervical carcinoma, In utero exposure to DES Vaginal Cancer
- Rare: 1% of gynecological malignancies and is usually secondary to other cancer
- Peak incidence at 60-65 years of age
- Squamous cell represents 95% caused by HPV
- Adenocarcinoma caused by DES exposure
- The most common location of vaginal carcinoma is the upper one-third of the posterior vaginal wall
- Usually presents as changes in menstrual period and/or abnormal vaginal bleeding
TX: with radiation therapy
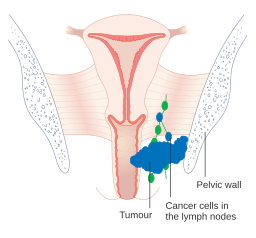 Diagram showing stage 3 vaginal cancer.
Patient will present as → a 50-year-old female with vaginal itching, and irritation red/white ulcerative crusted lesions on the vulva Vulvar Cancer
- Peak incidence is at 50 years old
- Vaginal pruritus is the most common presentation (70% will present with this symptom)
- 90% are squamous cell cancers and melanoma. Risks include HPV subtypes 16, 18, and 31 – pruritic black lesions
DX: Application of acetic acid or staining with toluidine blue may help direct optimal biopsy location
TX: Vulvectomy and lymph node dissection
Paget’s – pruritic red lesions
TX: Local resection
 Vulvar carcinoma on CT |
Back to PANCE Blueprint Reproductive System (7%)