60 y/o with abdominal pain, vomiting, and altered mental status
Patient will present as → a 45-year-old female with a long history of a heart murmur with one week of increasing fatigue and low-grade fevers. She had a dental cleaning two weeks ago. She denies any hematuria, neurological symptoms, or changes in the appearance of her hands and fingernails. Her past medical history is otherwise insignificant. On physical exam, her temperature is 38.1 C (100.6 F), heart rate is 92/min, blood pressure is 118/67, and respiratory rate is 16/min. She appears fatigued but in no acute distress. Cardiac auscultation reveals a grade III/VI holosystolic murmur heard best at the cardiac apex in the left lateral decubitus position. Pulmonary, abdominal, and extremity exams are within normal limits. An echocardiogram is performed and is shown here. The patient is admitted and started on empiric IV antibiotics. Three days later, 4/4 blood cultures grow Streptococcus viridans which is highly sensitive to penicillin.
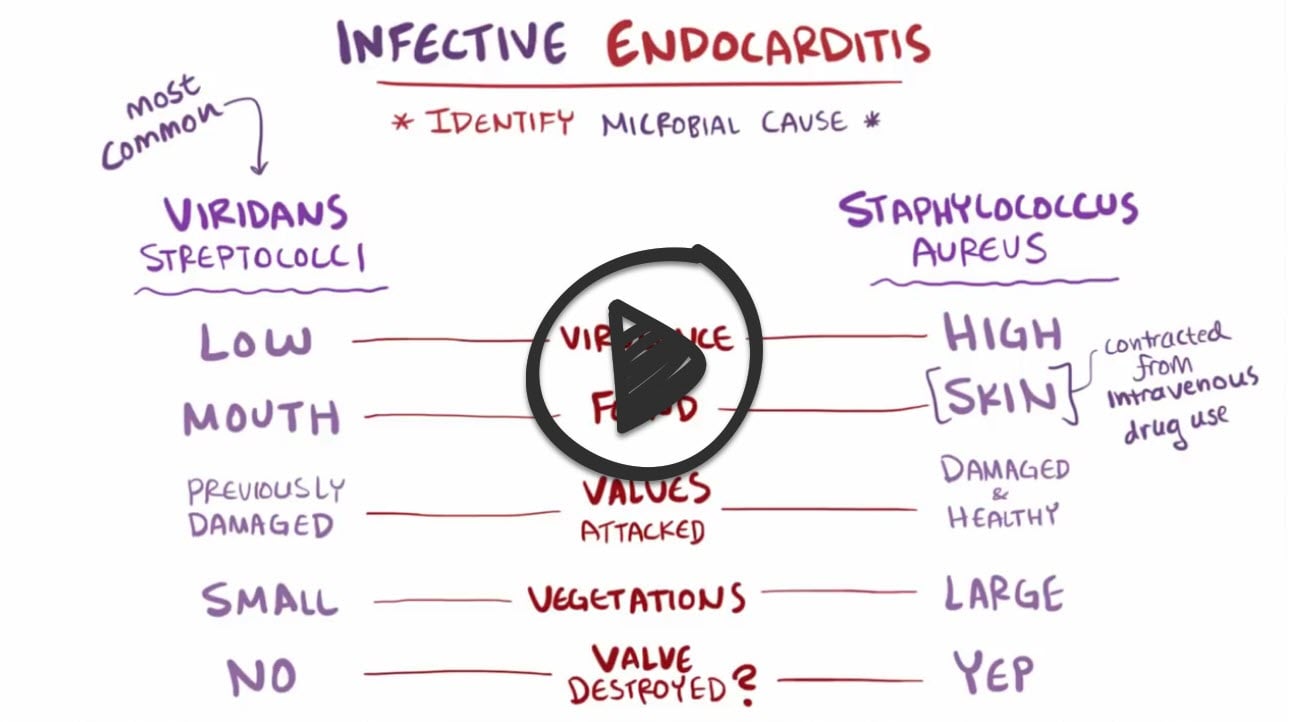
Infective endocarditis is an infection of the inner surface of the heart (endocardium) or heart valves due to an infection in the bloodstream, usually with bacteria (commonly, streptococci or staphylococci) or fungi
It causes fever, heart murmurs, petechiae, anemia, embolic phenomena, and endocardial vegetations
- Acute bacterial endocarditis: Infection of normal valves with a virulent organism (S. aureus)
- Subacute bacterial endocarditis: Indolent infection of abnormal valves with less virulent organisms (S. viridans)
- Endocarditis with intravenous drug users - Staphylococcus aureus
- Prosthetic valve endocarditis - Staphylococcus epidermidis
"Differentiate bacterial endocarditis from acute rheumatic fever which is a multi-system autoimmune response and may also affect the heart and valves - diagnosed by Jones criteria"
Vegetations may result in valvular incompetence or obstruction, myocardial abscess, or mycotic aneurysm.
- Candida is a slow-growing organism. The most common source is a contaminated line. It typically causes large vegetations in endocarditis.
- Large vegetation endocarditis in the early post–valve replacement period (2 months post-surgery) is most likely due to fungus, that is, Candida infection. Amphotericin B is recommended, followed by several weeks of antifungals that carry fewer adverse events.
- HACEK organisms tend to grow on native valves
- Staphylococcus aureus causes smaller vegetations; it is more common in injection drug users
- Streptococcus viridans is the most common cause of endocarditis. It typically occurs as a late complication of valve replacement and presents as small vegetations and embolic events.
- Endocarditis can occur at any age. Men are affected about twice as often as women. IV drug abusers and immunocompromised patients are at the highest risk.
- Most patients with a new murmur or change in an existing murmur; signs of heart failure (rales, edema) if valve function compromised
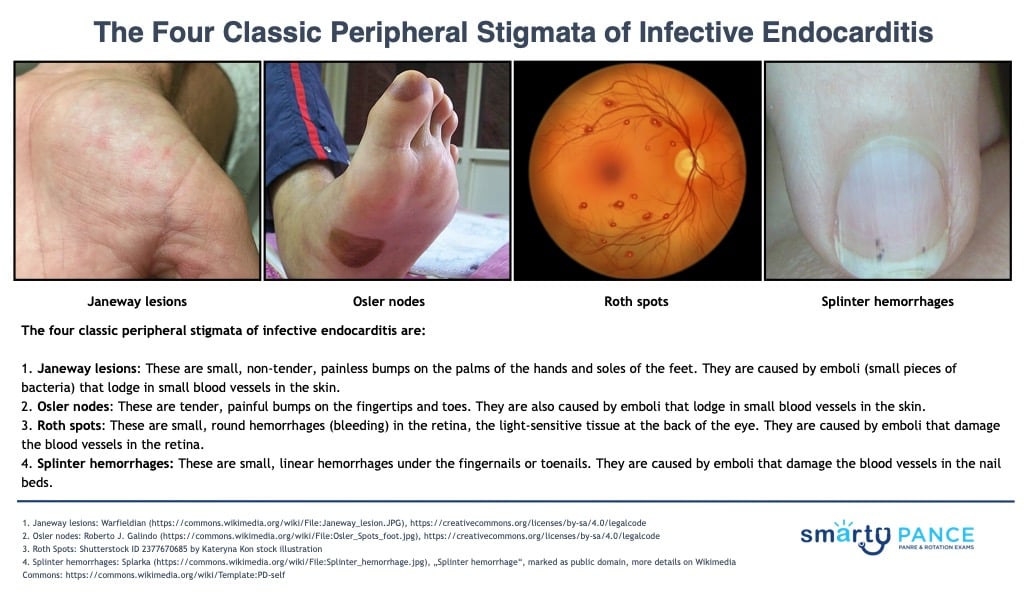
- Janeway lesions: These are small, non-tender, painless bumps on the palms of the hands and soles of the feet. They are caused by emboli (small pieces of bacteria) that lodge in small blood vessels in the skin.
- Osler nodes (remember “O” for “ouchy”: These are tender, painful bumps on the fingertips and toes. They are also caused by emboli that lodge in small blood vessels in the skin.
- Roth spots: These are small, round hemorrhages (bleeding) in the retina. They are caused by emboli that damage the blood vessels in the retina.
- Splinter hemorrhages: These are small, linear hemorrhages under the fingernails or toenails. They are caused by emboli that damage the blood vessels in the nail beds.
The peripheral stigmata of infective endocarditis are not always present, and they can be seen in other conditions, such as rheumatic fever and systemic lupus erythematosus. However, they can be a valuable clue to the diagnosis of infective endocarditis, especially if they are present in conjunction with other symptoms of the condition, such as fever, chills, and a heart murmur.
In addition to the four classic peripheral stigmata, there are several other physical signs that can be seen in people with infective endocarditis. These include:
- Petechiae: These are small, flat hemorrhages on the skin. They are caused by bleeding from small blood vessels.
- Purpura: These are larger, raised hemorrhages on the skin. They are also caused by bleeding from small blood vessels.
- Clubbing: This is a thickening of the fingertips and/or toenails. It is caused by a decrease in the amount of oxygen in the blood.
- Splenomegaly: This is an enlargement of the spleen. It is caused by an increased number of white blood cells in the spleen.
- Hepatomegaly: This is an enlargement of the liver. It is caused by inflammation or infection of the liver.
- Hematuria: Due to emboli or glomerulonephritis.
- Neurologic findings consistent with CVA, such as visual loss, motor weakness, and aphasia
Diagnosis requires demonstration of microorganisms in blood and usually echocardiography
- Blood cultures (before antibiotics are started) 3 sets at least 1 hour apart
- EKG at regular intervals
- LABS: CBC, ESR, RF
A transesophageal echocardiogram is the gold standard
Modified Duke Criteria for Diagnosis of Infectious Endocarditis
Definite: 2 major criteria, or 1 major and 3 minor criteria, or 5 minor criteria
Possible: 1 major and 1 minor criteria, or 3 minor criteria
- Major clinical criteria
- Positive blood culture: isolation of typical microorganism for IE from 2 separate blood cultures or persistently positive blood culture
- Single positive blood culture for C. burnetii or antiphase-1 IgG antibody titer >1:800
- Positive echocardiogram: presence of vegetation, abscess, or new partial dehiscence of a prosthetic valve; must be performed rapidly if IE is suspected
- New valvular regurgitation (change in preexisting murmur not sufficient)
- Minor criteria
- Predisposing heart condition or IV drug use
- Fever ≥38.0°C (100.4°F)
- Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, Janeway lesions
- Immunologic phenomena: glomerulonephritis, Osler nodes, Roth spots, rheumatoid factor (RF). Microbiologic evidence: positive blood culture, but not a major criterion (excluding single positive cultures for coagulase-negative staphylococci and organisms that do not cause endocarditis) or serologic evidence of infection likely to cause IE
Management - treatment consists of prolonged antimicrobial treatment and sometimes surgery
- IV antibiotics (based on the organism and its susceptibility)
- Sometimes, valve debridement, repair, or replacement
- Initial therapy before organism identification (but after adequate blood cultures have been obtained) should be broad-spectrum to cover all likely organisms.
- Typically, patients with native valves and no IV drug abuse receive IV ampicillin + nafcillin + gentamicin
- Patients with a prosthetic valve receive IV vancomycin + gentamicin + rifampin
- IV drug abusers receive IV nafcillin
- In all regimens, penicillin-allergic patients require a substitution of vancomycin
Antibiotic prophylaxis to prevent recurrent endocarditis is recommended: 2 g of Amoxicillin 30-60 minutes before the procedure
 Osmosis Osmosis |
|
 |
Bacterial endocarditis is an infection of the inner surface of the heart or heart valves due to bacteria in the bloodstream, typically introduced via dental or medical procedures in the mouth, intestinal tract, or urinary tract. The bacteria can grow on the edges of a heart defect or surface of an abnormal valve and continue to grow to produce large particles called vegetations. These particles can then break off and embolize to the lungs, brain, kidneys, and skin. Symptoms and signs of endocarditis vary but include prolonged fever, a new or changing heart murmur, and specific vascular and immunologic phenomena. Vascular phenomena include septic emboli, Janeway lesions, splinter hemorrhages, and renal and splenic infarcts. Immunologic phenomena include Osler’s nodes and Roth’s spots.
Play Video + QuizDuke’s Criteria
The Duke criteria are a set of clinical criteria set forward for the diagnosis of infective endocarditis. Fulfilling the criteria includes either having 2 major criteria, 1 major and 3 minor criteria, or 5 minor criteria. The two major criteria are positive blood cultures for infective endocarditis and evidence of endocardial involvement. The five minor criteria are having a predisposing heart condition or intravenous drug use, fever, vascular phenomena, or having microbiologic evidence or echocardiographic evidence that does not meet the major criteria.
Play Video + QuizQuestion 1 |
True | |
False |
Question 2 |
True | |
False |
Question 3 |
True | |
False |
Question 4 |
True | |
False |
Question 5 |
Bicuspid aortic valve | |
Prosthetic heart valve | |
Congenital heart disease | |
History of endocarditis |
Question 6 |
Amoxicillin 2g 30-60 minutes before the procedure | |
Amoxicillin 1g 30-60 minutes before the procedure | |
Amoxicillin 2g three hours before the procedure | |
Clindamycin 600 mg 30-60 minutes before the procedure |
Question 7 |
Fever greater than 100.4 | |
Sustained bacteremia (2 + blood cultures by organism known to cause endocarditis) | |
Predisposing condition (abnormal valves, IVDA, indwelling catheters) | |
Immunologic phenomena: Osler's nodes, Roth spots | |
Vascular and Embolic phenomena: Janeway lesions, pulmonary emboli |
Question 8 |
Candida albicans | |
HACEK organisms Hint: HACEK organisms tend to grow on native valves. | |
Staphylococcus aureus Hint: Staphylococcus causes smaller vegetations; it is more common in injection drug users. | |
Streptococcus viridans Hint: Streptococcus viridans is the most common cause of endocarditis. It typically occurs as late complication of valve replacement and presents as small vegetations and embolic events. |
Question 9 |
Electrocardiogram Hint: This patient's signs and symptoms are consistent with infective endocarditis. The diagnostic study of choice would be a transesophageal echocardiogram. | |
CT angiogram of the chest Hint: This patient's signs and symptoms are consistent with infective endocarditis. The diagnostic study of choice would be a transesophageal echocardiogram. | |
Cardiac catheterization Hint: This patient's signs and symptoms are consistent with infective endocarditis. The diagnostic study of choice would be a transesophageal echocardiogram. | |
Transesophageal echocardiogram |
Question 10 |
This patient does not require antibiotic prophylaxis for a routine dental cleaning. | |
This should receive Pen VK 250 mg p.o. QID for 10 days after the procedure. | |
This patient should receive Amoxicillin 2 grams 30-60 minutes before the procedure Hint: This would be the preferred regimen for a patient requiring antibiotic prophylaxis. See A for explanation. | |
This patient should receive Erythromycin 250 mg QID for 1 day before the procedure and then 10 days after the procedure. |
Question 11 |
Metabolic acidosis Hint: See B for explanation. | |
Systemic arterial embolization of vegetation | |
Hypotension and tachycardia Hint: See B for explanation. | |
Activation of the immune system Hint: Glomerulonephritis and arthritis result from activation of the immune system. |
Question 12 |
Acute myocardial infarction Hint: Acute MI presents with complaint of chest pain, SOB, not with fever and myalgias. | |
Bacterial endocarditis | |
Acute pericarditis Hint: Pericarditis does not present with systolic or diastolic murmur or vegetation, more commonly pericardial friction rub would be noted. | |
Restrictive cardiomyopathy Hint: Restrictive cardiomyopathy will show impaired diastolic filling on echocardiogram and is not associated with fever. |
|
List |
References: Merck Manual · UpToDate