Patient with acute lymphocytic leukemia (ALL) will present as → a 5 y/o child with bone pain, bleeding, and fever. His mom notes that the patient has been less active and has had recurrent upper respiratory infections over the past several months. Clinical examination reveals diffuse lymphadenopathy. His CBC demonstrates anemia and leukopenia, and the blood smear shows peripheral blasts. Bone marrow biopsy demonstrates 30% lymphoblasts.
Patient with chronic lymphocytic leukemia (CLL) will present as → a 60-year-old male complains of fatigue. On physical exam, he has painless cervical lymphadenopathy and hepatosplenomegaly. His blood tests demonstrate severe anemia, decreased neutrophil count, and immature B cells that broke apart during the peripheral smear.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Acute lymphocytic leukemia (ALL): CHILD + lymphadenopathy + bone pain + bleeding + fever in a CHILD, bone marrow > 20% blasts in bone marrow
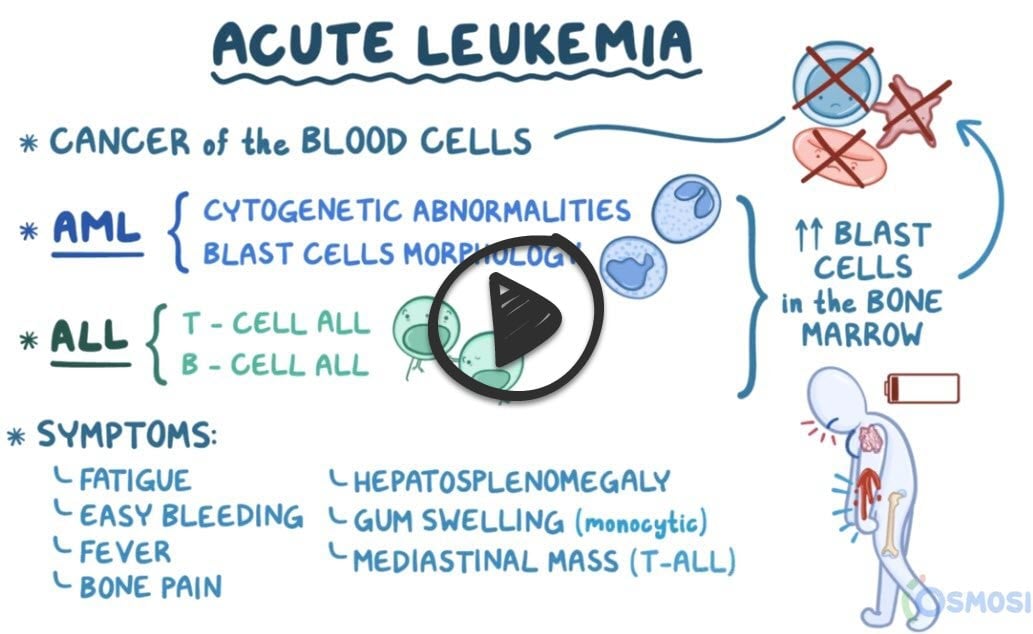
- In acute leukemia, there’s uncontrolled proliferation of partially developed WBCs (blast cells), which build up in the blood over a brief period of time
- ALL results from a proliferation of cells from the lymphoid line (vs. the myeloid line in AML) and is classified into T-cell ALL, where there’s proliferation of T-cell precursors, and B-cell ALL (70-80% of cases), where there’s proliferation of B-cell precursors
- Caused by chromosomal translocations (12,21) and (9,22)
- Population: Children - most common childhood malignancy peak age 3-7
- Symptoms of ALL include fatigue because of the anemia, easier bleeding (gingival bleeding, bruising, and nosebleeds) because of thrombocytopenia, and more frequent infections because of the leukopenia
- Abnormal lymphoblasts in ALL can also infiltrate the lymph nodes and other lymphatic tissue, so it’s also called acute lymphoblastic lymphoma
- A key clinical symptom in T-cell ALL is that the abnormal lymphoblasts migrate to the thymus like normal T-cells do and cause thymus enlargement, which can present as a mass or growth in the mediastinum.
- Highly responsive to chemotherapy (remission > 90%)
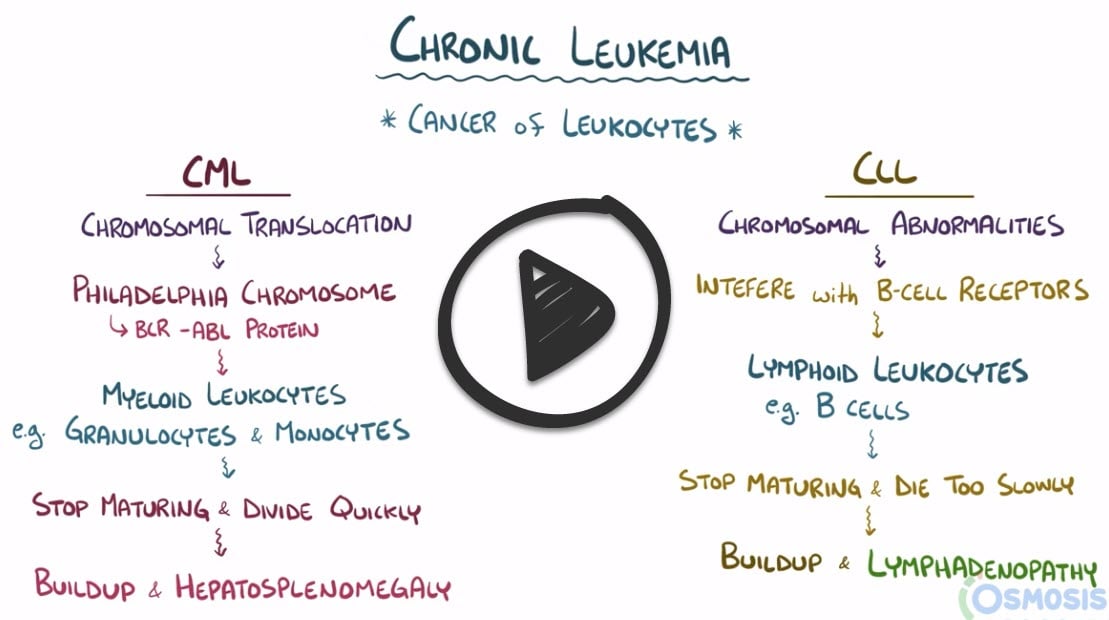
Chronic Lymphocytic Leukemia (CLL): Middle age/elderly patient, often asymptomatic (seen on blood tests), fatigue, lymphadenopathy, and splenomegaly
- Population: Adults - peak age 50 y/o
- It is not caused by one particular mutation but results from a variety of chromosomal mutations that affect lymphocytes, in particular B cells
- Just like with the blast cells in ALL, partially mature B-cells can move into the lymphatic tissues and cause lymphadenopathy. B cells in these nodes will accumulate to form “lymphomas,” which is why CLL is sometimes called small lymphocytic lymphoma
- These abnormal B Cells are likely to produce autoantibodies, resulting in immune thrombocytopenia and autoimmune hemolytic anemia
- Hairy cell leukemia is a special but rare type of CLL linked with a mutation in the BRAF gene. The affected B-cells have hair-like projections, giving them a fuzzy appearance
- Up to 70% of persons with CLL are asymptomatic at diagnosis, and when symptoms do appear, they are typically nonspecific and include easy fatigability and weight loss. Some patients can present with lymphadenopathy and hepatosplenomegaly
- Diagnostic studies: SMUDGE CELLS on peripheral smear, mature lymphocytes
- Treatment with observation: if lymphocytes are > 100,000 or symptomatic, treat with chemo
ALL
- CBC: pancytopenia (anemia, thrombocytopenia, leukopenia)
- Peripheral blood smear demonstrates peripheral blasts. Blast cells in the peripheral smear may approach 90% of the white blood cell (WBC) count
- Bone marrow aspiration and biopsy: with > 20% blasts
- Histochemical studies, cytogenetics, and immunophenotyping studies help distinguish the blasts of ALL from those of AML or other disease processes
CLL
- CBC: pancytopenia (anemia, thrombocytopenia, leukopenia) with an increase in the absolute number (>5,000) of lymphocytes in the peripheral blood
- The peripheral blood smear of patients with CLL demonstrates lymphocytosis (small mature lymphocytes) and often shows “smudge” cells, which are immature B cells that have broken apart during the smear
- Evaluation of the bone marrow is not usually necessary
Acute Lymphoblastic Leukemia (ALL): Chemotherapy
- Highly responsive to combination chemotherapy with a remission of > 90%.
- Stem cell transplant if relapse.
Chronic Lymphoblastic Leukemia (CLL): Observation if indolent
- Chronic - treat with chemo
 Osmosis Osmosis |
|
| Acute leukemia | |
 |
|
| Chronic leukemia | |
|
Chronic lymphocytic leukemia (CLL) is the most common adult leukemia in the United States. Most patients are older than 60 years of age and there is a 2 to 1 male predominance. In CLL, lymph nodes are diffusely effaced by an infiltrate of small lymphocytes. The peripheral blood also contains large numbers of small round lymphocytes with minimal cytoplasm. Some of these cells often come disrupted in the process of making smears and produce smudge cells that are characteristic of CLL. The bone marrow is almost always involved. Unlike most other lymphoid malignancies, chromosomal translocations are relatively rare. Patients are often asymptomatic at diagnosis and when symptoms do appear, they are typically nonspecific and include easy fatigability and weight loss. Some patients can present with lymphadenopathy and hepatosplenomegaly. Hypogammaglobulinemia is also common and contributes to disruption of normal immune function. CLL is also associated with warm autoimmune hemolytic anemia, which is often caused by the attachment of IgG antibodies to red blood cells.
Play Video + QuizAcute Lymphoblastic Leukemia (ALL)
Acute lymphoblastic leukemia (ALL) is a neoplasm of immature B and T cells (pre B and pre T cells), which are referred to as lymphoblasts. About 85% of ALLs are B cell tumors and typically manifest in children less than 15 years of age. The less common T cell ALLs tend to present in adolescents as a thymic lymphoma in the mediastinum. In these cancers, the bone marrow is typically hypercellular and packed with lymphoblasts, which replace the normal elements within the bone marrow. Therefore, common symptoms include fatigue due to anemia and bleeding due to thrombocytopenia. Neoplastic infiltration of bone marrow can also cause bone pain from marrow expansion and infiltration of the subperiosteum. Immunostaining for terminal deoxynucleotidyl transferase (TdT), a specialized DNA polymerase that is expressed only in pre B and pre T lymphoblasts is positive in more than 95% of cases. Majority of these B-cell tumors also express the common acute lymphoblastic leukemia antigen (CALLA). Approximately 90% of ALLs demonstrate chromosomal changes, most commonly hyperploidy of chromosomes. These chromosomal aberrations are thought to cause the dysregulation of the expression and function of transcription factors that are required for normal B and T cell development. A fraction of B cell tumors contain a translocation of genes 12;21 involving the genes TEL and AML1, two genes required in very early hematopoiesis. This translocation is associated with better prognosis. This tumor is known to spread to the CNS and testes. With aggressive chemotherapy, about 95% of children with ALL obtain complete remission.
Question 1 |
Acute lymphocytic leukemia Hint: Acute lymphocytic leukemia is more common in children and presents with blasts in the peripheral blood | |
Acute myelogenous leukemia Hint: Acute myelogenous leukemia presents with pancytopenia and presence of blasts in the peripheral blood. | |
Chronic lymphocytic leukemia | |
Chronic myelogenous leukemia Hint: Chronic myelogenous leukemia presents with elevated WBC count, marked left shift in the myeloid series of cells, and positive for Philadelphia chromosome. |
Question 2 |
acute myelogenous leukemia (AML) Hint: AML is the most common leukemia in adults, but it is less common in children. | |
acute lymphocytic leukemia (ALL) | |
chronic myelogenous leukemia (CML) Hint: CML is very rare in children, occurring in approximately 2% of childhood leukemia cases. | |
chronic lymphocytic leukemia (CLL) Hint: CLL is also unusual in children. | |
equal numbers of AML and ALL |
Question 3 |
birth and 2 years Hint: See B for explanation | |
2 and 3 years | |
12 and 15 years Hint: See B for explanation | |
8 and 12 years Hint: See B for explanation | |
5 and 15 years Hint: See B for explanation |
Question 4 |
white Hint: The frequency for whites is 30 to 40 per 1 million, | |
Hispanic | |
African American Hint: African Americans is approximately one-third the rate of whites. | |
Asian | |
no ethnic variation |
Question 5 |
the peak age at onset is 12 years Hint: The peak incidence for ALL is between 2 and 3 years of age. | |
at the time of diagnosis, most patients have a thrombocytosis Hint: Most patients with ALL will have a decreased hemoglobin level and platelet count at the time of diagnosis | |
CBC with differential is the most useful initial test | |
a chest radiograph is the most useful initial test Hint: A chest radiograph should be obtained to search for a possible mediastinal mass. |
|
List |
References: Merck Manual · UpToDate (ALL) (CLL)


 Lecture
Lecture