To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
MS is an autoinflammatory disease causing demyelination, neuronal loss, and scarring within the white matter of the brain and spinal cord.
- Usually present with visual disturbances often over many years.
- Recurrent visits for different neurologic symptoms, often the first visit is for visual problems, followed by weakness in distal limb, ataxia, or paresthesias over several years. Distal to proximal muscle weakness.
- Most common symptoms:
- Sensory loss
- Optic neuritis
- Weakness
- Paresthesias
- Lhermitte's sign (patient in the video above) refers to an electrical shock sensation in the limbs and torso, brought on by movement (mostly flexion) of the neck. It is due to pathology of the cervical spinal cord and a common finding in early MS
Four recognized forms of multiple sclerosis (MS):
-
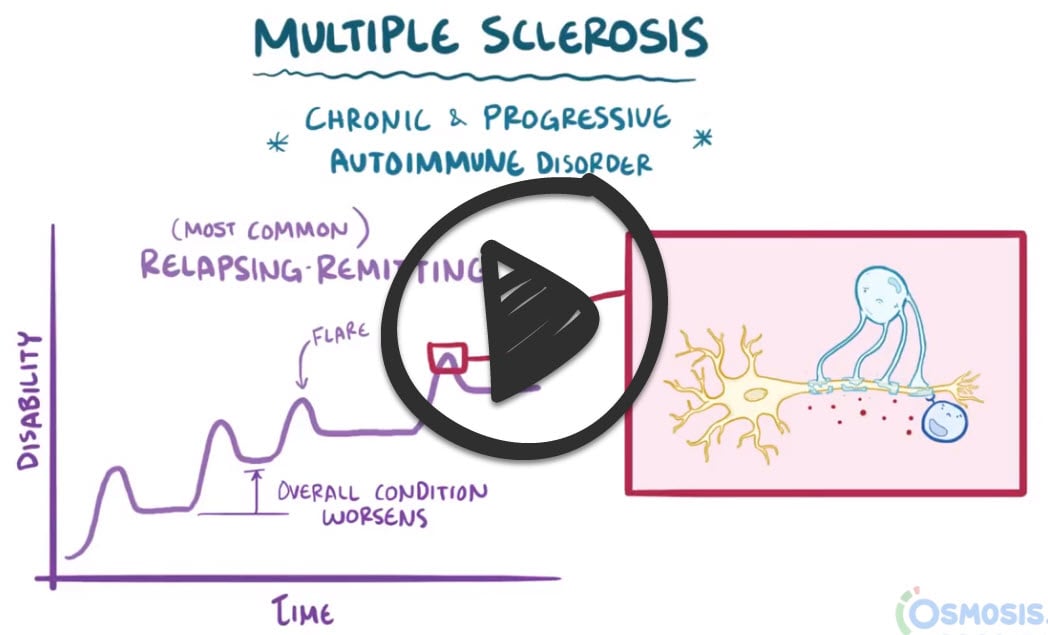
Relapsing-remitting multiple sclerosis (RRMS) (85% MOST COMMON TYPE) episodic flare-ups occurring over days to weeks between periods of neurologic stability. During attacks, new symptoms may present, whereas previous symptoms may worsen. Complete recovery or residual deficits may ensue following each bout.
-
Secondary progressive multiple sclerosis (SPMS) beginning as RRMS, progressive deterioration in neurologic function, unassociated with attacks, eventually ensues (progression may continue or halt). ∼2% risk per year of RRMS becoming SPMS
-
Primary progressive multiple sclerosis (PPMS) (∼15%): a steady decline of neurologic function from the onset of disease without episodic flares
-
Progressive relapsing multiple sclerosis (PRMS) (∼5%): a steady decline of neurologic function from the onset of disease with episodic flare-ups
DX with MRI looking for plaques associated with MS (McDonald Diagnostic Criteria)
- The most sensitive and specific investigation for this disorder is an MRI of the brain and spinal cord
- The MRI scan will reveal plaque formation (a subsequent stage that results from the loss of the myelin sheath in different parts of the CNS) and spotty and irregular demyelination in the affected areas in a patient with MS
- If an MRI is non-diagnostic in a patient with multiple sclerosis, the next best test is a lumbar puncture, which should demonstrate oligoclonal bands
- Visual evoked potentials and/or optical coherence tomography can also be used to support the diagnosis
"The targeted cells in the MS disease process are the oligodendrocytes of the CNS. These cells fabricate and maintain the myelin sheaths, the material covering the axons that is necessary for the normal conduction of nerve impulses."
McDonald diagnostic criteria for multiple sclerosis are clinical, radiographic, and laboratory criteria used in the diagnosis of multiple sclerosis
| Number of lesions with objective clinical evidence | Additional data needed for a diagnosis of multiple sclerosis | |
| ≥ 2 clinical attacks | ≥ 2 | None |
| 1 (as well as clear-cut historical evidence of a previous attack involving a lesion in a distinct anatomical location) | None | |
| 1 | Dissemination in space demonstrated by an additional clinical attack implicating a different CNS site or by MRI | |
| 1 clinical attack | ≥ 2 | Dissemination in time demonstrated by an additional clinical attack or by MRI◊ OR demonstration of CSF-specific oligoclonal bands |
| 1 | Dissemination in space demonstrated by an additional clinical attack implicating a different CNS site or by MRIΔ
AND Dissemination in time demonstrated by an additional clinical attack or by MRI◊ OR demonstration of CSF-specific oligoclonal bands§ |
Recommended medications include corticosteroids (for acute attacks), interferon betas (Avonex), fingolimod (Gilenya), natalizumab (Tysabri), dimethyl fumarate (Tecfidera), and mitoxantrone (Novantrone).
- Physical therapy and exercise may help increase coordination and decrease spasticity.
- Modafinil, amantadine, pemoline, and methylphenidate to treat fatigue
- Urge incontinence can be treated with Oxybutynin
- Drugs are useful in treating spasticity - Baclofen, tizanidine, diazepam, and dantrolene
- Identifying factors that trigger symptoms is critical for avoiding exacerbations of the disease.
 Osmosis Osmosis |
|
 |
Multiple sclerosis (MS) is a demyelinating disorder that demonstrates unclear pathogenesis but has significant evidence of autoimmune involvement. Clinical presentation is variable with subtypes delineated by symptom exacerbation, but it classically presents with Charcot’s neurologic triad, which consists of scanning speech, internuclear ophthalmoplegia, and nystagmus, with symptoms characteristically worsening after a hot shower. However, a wide range of clinical manifestations may be seen including optic neuritis, urinary, and fecal incontinence, motor abnormalities such as trembling and paresis, sensory changes ranging from pain to numbness and depression, all of which typically, though not exclusively, display a relapsing pattern. Diagnosis of MS includes the gold standard presence of simultaneous periventricular plaques on MRI, as well as elevated CSF immunoglobulins, most commonly IgG, and finally identification of oligoclonal IgG bands on immunoelectrophoresis.
| MS Symptoms and Diagnosis | Play Video + Quiz |
| MS Features and Mechanisms | Play Video + Quiz |
| MS Interventions | Play Video + Quiz |
Question 1 |
Multiple sclerosis | |
Huntington’s disease | |
Parkinson’s disease | |
Neurofibromatosis | |
Amyotrophic lateral sclerosis (ALS) |
Question 2 |
relapsing-remitting | |
secondary progressive Hint: In the secondary progressive category, gradual neurologic deterioration occurs with or without superimposed acute relapses in patients who previously had relapsing-remitting MS. | |
primary progressive Hint: In primary progressive MS, gradual continuous deterioration occurs from the onset of symptoms. | |
progressive relapsing Hint: In progressive relapsing MS, gradual neurologic deterioration occurs from the onset of symptoms but with subsequent superimposed relapses. | |
none of the above |
Question 3 |
computed tomography scan of the head and spinal cord | |
magnetic resonance imaging (MRI) scan of the brain and spinal cord | |
serum vitamin B12 levels | |
Beck depression scale | |
Venereal Disease Research Laboratory test for syphilis |
Question 4 |
racial predilection: whites more often than African Americans | |
sex predilection: females more often than males | |
high socioeconomic status | |
environmental exposure | |
all of the above |
Question 5 |
in 80% to 90% of all cases, the first episode is followed by a cycle of relapses and remissions Hint: This is a true statement | |
50% of those with relapsing-remitting cases switch to a progressive course approximately 5 years after the onset of the first symptoms Hint: This is a true statement | |
10% of patients have progressive disease from the onset of symptoms Hint: This is a true statement | |
up to 10% of patients with this disease have a relatively “benign” course Hint: This is a true statement | |
all of the above |
Question 6 |
the neurotransmitter balance in the CNS | |
the oligodendrocytes of the CNS | |
the peripheral nerves in the posterior columns of the spinal cord | |
the cerebral hemispheres | |
the cerebellum |
Question 7 |
adrenocorticotropic hormone (ACTH) | |
corticosteroids | |
mitoxantrone (Novantrone) | |
interferon beta | |
natalizumab (Tysabri) | |
all of the above |
- Corticosteroids are the mainstay for treatment of initial and acute relapses of MS. Although corticosteroid therapy can shorten the duration of a relapse, it is uncertain whether the long-term course of the disease will be altered with their use.
- ACTH has been replaced by high-dose intravenous methylprednisolone.
- Interferon beta has been the most common long-term treatment for patients with relapsing-remitting MS. Interferon beta is available in two forms, 1a and 1b. Both types are generally well tolerated by most patients. Influenza-like symptoms are common after each injection, and questions about different responses in different people remain. Therefore, interferon beta doses should be individualized.
- Newer treatments are becoming more common and are usually administered in special clinics by experts in multiple sclerosis. Glatiramer acetate is an alternative for those who have failed to respond to interferon beta. Glatiramer helps prevent the body’s immune system from attacking nerve fibers. Mitoxantrone slows disability and reduces the relapse rate. Natalizumab reduces the relapse rate.
Question 8 |
interferon has been shown to reduce the rate of relapse | |
interferon may delay the progression to disability | |
interferon reduces the development of new lesions as seen by MRI | |
interferon delays the increase in volume of lesions as seen by MRI | |
all of the above |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture


