17 y/o with difficulty breathing and tingling fingers
Patient will present as → a 30-year-old male who arrives at your ED in distress stating that he had " a heart attack." The event started suddenly and was associated with diaphoresis, chest pain, tachycardia, and tachypnea. Troponins and ECG are within normal limits. Upon further questioning, he reports some numbing around his lips and that he has such episodes every few days for the past three months. The attacks have become so severe that he has been missing work and didn't go to last week's Christmas party. He denies recreational or illicit drug use. He further shares that he recently divorced and has had no social support. Recent lab results have all been normal or within standard limits, including TSH and vitamin B12.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Key Points
Panic disorder can occur with or without agoraphobia. It is characterized by the occurrence of panic attacks - sudden unexpected periods of intense fear or discomfort. Symptoms develop abruptly and reach a peak within 10 minutes.
- About 15% of the general population experiences panic attacks. 3% of women and 1.7% of men have panic disorder
- To be considered panic disorder one must experience: recurrent, unexpected panic attacks with at least a month or more of worry or avoidant behavior
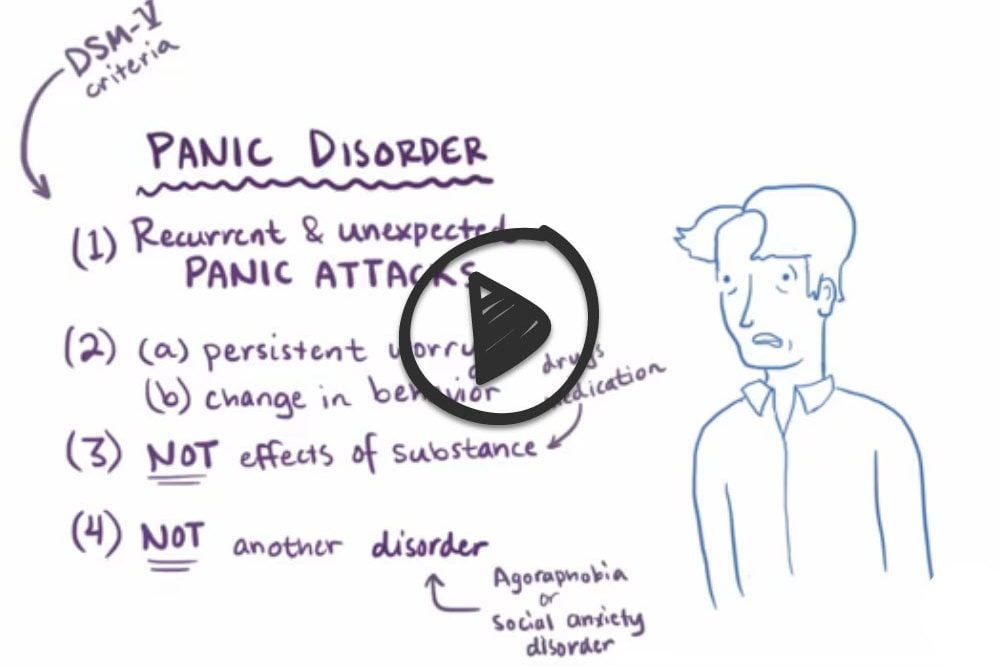
DSM-5 Diagnostic Criteria
A. Recurrent unexpected panic attacks. A panic attack is an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time four (or more) of the following symptoms occur: Note: The abrupt surge can occur from a calm state or an anxious state.
- Palpitations, pounding heart, or accelerated heart rate.
- Sweating.
- Trembling or shaking.
- Sensations of shortness of breath or smothering.
- Feelings of choking.
- Chest pain or discomfort.
- Nausea or abdominal distress.
- Feeling dizzy, unsteady, lightheaded, or faint.
- Chills or heat sensations.
- Paresthesias (numbness or tingling sensations).
- Derealization (feelings of unreality) or depersonalization (being detached from oneself).
- Fear of losing control or “going crazy.”
- Fear of dying.
Note: Culture-specific symptoms (e.g., tinnitus, neck soreness, headache, uncontrollable screaming, or crying) may be seen. Such symptoms should not count as one of the four required symptoms.
B. At least one of the attacks has been followed by 1 month (or more) of one or both of the following:
- Persistent concern or worry about additional panic attacks or their consequences (e.g., losing control, having a heart attack, “going crazy”).
- A significant maladaptive change in behavior related to the attacks (e.g., behaviors designed to avoid having panic attacks, such as avoidance of exercise or unfamiliar situations).
C. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hyperthyroidism, cardiopulmonary disorders).
D. The disturbance is not better explained by another mental disorder (e.g., the panic attacks do not occur only in response to feared social situations, as in social anxiety disorder; in response to circumscribed phobic objects or situations, as in specific phobia; in response to obsessions, as in obsessive-compulsive disorder; in response to reminders of traumatic events, as in posttraumatic stress disorder; or in response to separation from attachment figures, as in separation anxiety disorder).
At least a month or more of worry or avoidant behavior
- > 1 panic attack that reoccurs w/o warning and patients need to experience the abrupt onset of at least 4 of the following 13 symptoms:
- pounding heart or fast heart rate
- chest pain or discomfort
- sweating
- trembling
- shortness of breath
- nausea
- dizziness
- chills
- numbness
- feelings of choking
- feelings of being detached from oneself
- fear of losing control
- fear of dying
Treat with benzodiazepines if unable to wait for the SSRI to work, although be aware of abuse potential.
The mainstay of long-term treatment includes:
- SSRIs are 1'st line for long term treatment: Paroxetine, Sertraline, Fluoxetine
- Benzodiazepines: for acute attacks (watch for abuse)
- If panic disorder is very severe, anti-seizure medications may sometimes be prescribed
- CBT (relaxation, desensitization, examining behavior consequences)
- First, the person simply learns about panic disorder and how to identify certain symptoms
- Second, they monitor their panic attacks by keeping track of them using a diary
- Third, they work on breathing and relaxation techniques
- Fourth, they start rethinking and changing their beliefs about the severity of a panic attack with the goal of moving from catastrophic thinking to realistic thinking about the nature of their panic attacks
- Fifth, they allow themselves to be exposed to situations that provoke fear and anxiety
Question 1 |
Benzodiazepines Hint: Are appropriate for short term and/or episodic treatment | |
TCAs Hint: Not as likely to be used | |
SSRIs | |
Wellbutrin |
Question 2 |
diazepam (Valium) Hint: See D for explanation | |
chlordiazepoxide (Librium) Hint: See D for explanation | |
clorazepate (Tranxene) Hint: See D for explanation | |
alprazolam (Xanax) | |
clonazepam (Klonopin) Hint: See D for explanation |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture