Patient will present as → a 60-year-old woman with a severe drug-induced reaction on both lower limbs with few lesions elsewhere in addition to mucosal involvement of the mouth of two days duration. The insulting drug was sulfonamide, and the onset of the rash was within 48 hours of taking the drug. The rash is comprised of bilateral symmetrical bullae on a background of erythematous macules and patches in addition to erosions and peeling.
Stevens-Johnson syndrome (SJS) is a milder form of toxic epidermal necrolysis (TEN) with LESS THAN 10% of body surface area detachment
- Stevens-Johnson syndrome, toxic epidermal necrolysis, and SJS/TEN overlap. All three are part of a spectrum of severe cutaneous reactions (SCAR) which affect the skin and mucous membranes
The distinction between SJS, SJS/TEN overlap, and TEN is based on the type of lesions and the amount of the body surface area with blisters and erosions
- Blisters and erosions cover between 3% and 10% of the body in SJS
- 11–30% in SJS/TEN overlap
- over 30% in TEN
- Severe, potentially fatal, mucocutaneous drug reactions characterized by epidermal necrosis involving skin and at least 2 mucous membranes
- Most common with drug eruptions: Over 100 medications have been implicated in causing SJS especially sulfa and anticonvulsant medications
- Prodromal period for 1–7 days of low-grade fever, sore throat or upper respiratory infection or dysphagia, and general malaise; the patient may also complain of pain or stinging in the eyes
- Subsequent development of targetoid red papules and plaques with dusky, blistered, or eroded center as well as mucosal (lip, intraoral, conjunctival, urethral, anal) pain with blistering and erosions.
- The progression of the disease to sheets of widespread epidermal necrosis and sloughing may be hours. This is a medical emergency.
- Eye symptoms may be severe
- (+) Nikolsky's sign: skin peels away in sheets when pressure applied and rubbed.
Clinical evaluation and skin biopsy - shows necrotic epithelium
- If the test is available, elevated levels of serum granulysin taken in the first few days of a drug eruption may be predictive of SJS/TEN.
- Diagnosis is often obvious from the appearance of lesions and rapid progression of symptoms. Histologic examination of sloughed skin shows necrotic epithelium, a distinguishing feature.
- Differential diagnosis in SJS and early TEN include erythema multiforme, viral exanthems, and other drug rashes; SJS/TEN can usually be differentiated clinically as the disorder evolves and is characterized by significant pain and skin sloughing.
Mortality prediction scoring:
SCORTEN Scale
SCORTEN is an illness severity score that has been developed to predict mortality in SJS and TEN cases. One point is scored for each of the seven criteria present at the time of admission. The SCORTEN criteria are:
|
The risk of dying from SJS/TEN depends on the score.
|
ABCD 10 Mortality prediction model score
A: Age over 50 years (one point) B: Bicarbonate level < 20 mmol/L (one point) C: Cancer present and active (two points) D: Dialysis prior to admission (3 points) 10: Epidermal detachment ≥ 10% of body surface area on admission (one point)
| ABCD-10 Score | Predicted Mortality Rate,% (95% CI) |
|---|---|
| 0 | 2.3 (1.1-4.6) |
| 1 | 5.4 (3.2-8.7) |
| 2 | 12.3 (8.9-16.6) |
| 3 | 25.5 (19.6-32.5) |
| 4 | 45.7 (34.2-57.8) |
| 5 | 67.4 (50.8-80.6) |
| 6 | 83.6 (66.7-92.8) |
Stop all potentially offending medications
- Early admission to burn unit or pediatric intensive care unit for initial stabilization and management of fluid, electrolytes, and nutrition; airway stability; and eye care
- Prompt ophthalmology and dermatology consultation
- Intravenous immunoglobulin (IVIG)
- Steroids used to be the treatment of choice are now thought to be an increased risk for sepsis
 Osmosis Osmosis |
|
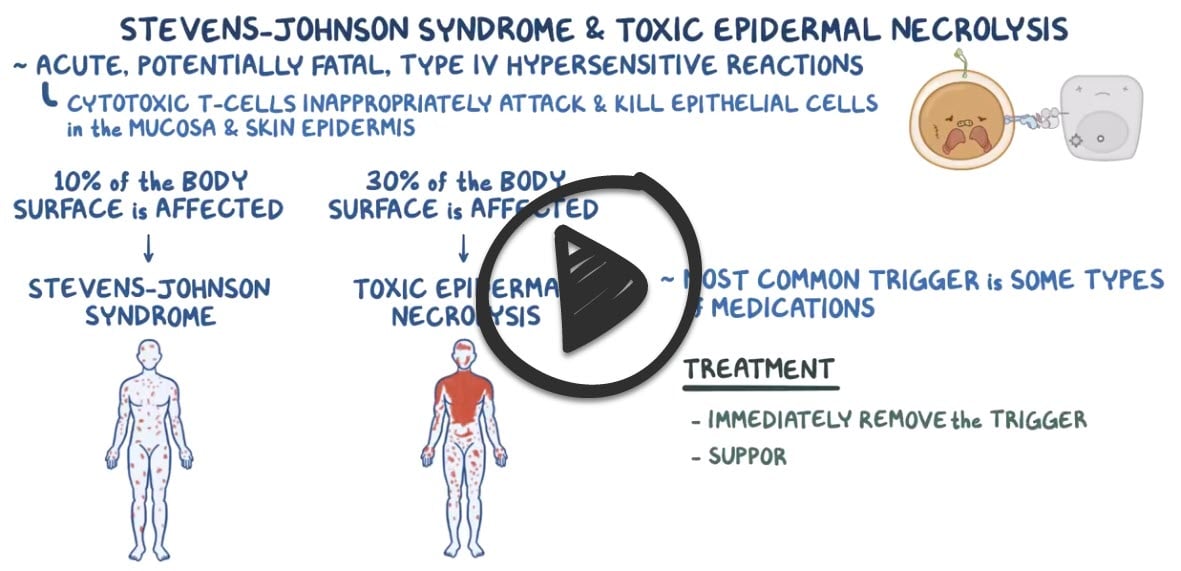 |
 Stevens-Johnson syndrome is a blistering skin disorder most often caused by drug reactions. It initially begins as a fever, but later involves the mucosa and skin, leading to blistering, necrolysis and skin sloughing. An important distinction to realize is that Stevens-Johnson syndrome (SJS) involves less than 30% of the body surface area. If more than 30% of the body surface area is involved, it is classified as Toxic Epidermal Necrolysis (TEN). This syndrome has a high mortality rate, but interventions include supportive care and intravenous immunoglobulin (IVIG) administration.
Stevens-Johnson syndrome is a blistering skin disorder most often caused by drug reactions. It initially begins as a fever, but later involves the mucosa and skin, leading to blistering, necrolysis and skin sloughing. An important distinction to realize is that Stevens-Johnson syndrome (SJS) involves less than 30% of the body surface area. If more than 30% of the body surface area is involved, it is classified as Toxic Epidermal Necrolysis (TEN). This syndrome has a high mortality rate, but interventions include supportive care and intravenous immunoglobulin (IVIG) administration.
| Stevens-Johnson syndrome | Play Video + Quiz |
| Lamotrigine | Play Video + Quiz |
| Ethosuximide | Play Video + Quiz |
| Carbamazepine (Tegretol) | Play Video + Quiz |
| Sulfa drug allergies | Play Video + Quiz |
Question 1 |
Phenytoin Hint: Antiepileptic and known SJS trigger | |
Allopurinol Hint: Frequent trigger for SJS | |
Sulfamethoxazole Hint: Sulfonamide antibiotic known for causing SJS | |
Ibuprofen | |
Carbamazepine Hint: Antiepileptic with SJS risk |
Question 2 |
It is a milder form of toxic epidermal necrolysis with less than 20% body surface area detachment | |
Nevirapine is a trigger | |
Loss of vision could be a complication | |
Corticosteroid may be used in the treatment of patients with SJS |
Question 3 |
High-dose systemic corticosteroids Hint: Their use in SJS is controversial and not universally recommended as an initial step. | |
Intravenous immunoglobulin (IVIG) Hint: May be used in treatment, but the priority is to stop the offending agent. | |
Immediate discontinuation of all non-essential medications | |
Start of broad-spectrum antibiotics Hint: Antibiotics are not routinely started unless there is evidence of secondary infection. | |
Cyclosporine therapy Hint: Used in some cases, but not before discontinuing the causative medication. |
|
List |
References: Merck Manual · UpToDate




