The NCCPA™ PANCE Dermatology Content Blueprint covers four disorders under the category of skin integrity
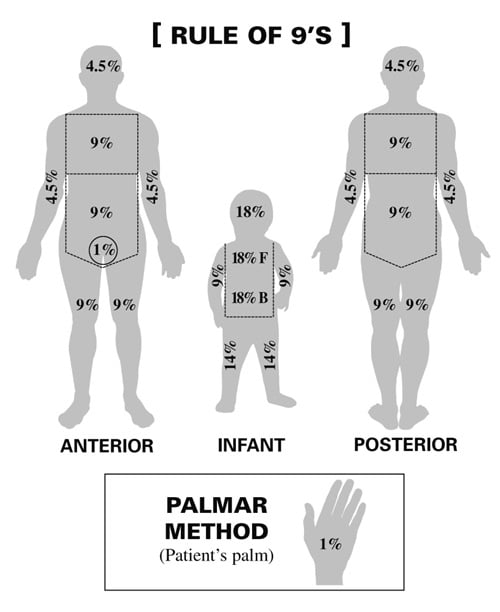
Body percentage:
- Rule of 9’s: Head 9%, Each arm 9%, Chest 9%, Abdomen 9%, Each anterior leg 9%, Each posterior leg 9%, Upper back 9%, Lower back 9%, Genitals 1%
- Palmar method: Patient’s palm equates to 1%
Degree involvement:
- 1st degree (sunburn): Erythema of involved tissue, skin blanches with pressure, the skin may be tender
- 2nd degree (partial thickness): Skin is red and blistered. The skin is very tender
- 3rd degree (full thickness): Burned skin is tough and leathery. Skin is non-tender
- 4th degree: Into the bone and muscle
Treatment: Monitor ABCs, fluid replacement, and sulfadiazine. Children with > 10% total body surface area and adults with > 15% total body surface area burns need formal fluid resuscitation
Suture removal — The timing of suture removal varies with the anatomic site
- Eyelids – Three days
- Neck – Three to four days
- Face – Five days
- Scalp – 7 to 14 days
- Trunk and upper extremities – Seven days
- Lower extremities – 8 to 10 days
Follow-up visits — Most clean wounds do not need to be seen prior to removal unless signs of infection develop. Highly contaminated wounds should be seen for follow-up in 48 to 72 hours. It is imperative that clear discharge instructions are given to every patient regarding signs of wound infection.
| Suture material | Knot security | Wound tensile strength | Tissue reactivity | Workability | Anatomic site |
| Nylon (Ethilon) | Good | Good | Minimal | Good | Skin closure anywhere |
| Polybutester (Novafil) | Good | Good | Minimal | Good | Skin closure anywhere |
| Polypropylene (Prolene) | Least | Best | Least | Fair | Skin closure anywhere. Blue dyed suture useful in dark-skinned individuals. |
| Silk | Best | Least | Most | Best | Rarely used |
| Suture material | Knot security | Wound tensile strength | Security (days)* | Tissue reactivity | Anatomic site |
| Fast-absorbing gut | Poor | Least | 4 to 6 | Most | Face |
| Vicryl Rapide | Good | Fair | 5 to 7 | Minimal | Face, scalp, undercast/splint |
| Surgical gut | Poor | Fair | 5 to 7 | Most | Face (rarely used) |
| Poliglecaprone 25 (Monocryl) | Good | Fair | 7 to 10 | Minimal | Face, consider in contaminated wounds needing deep closure |
| Chromic gut | Fair | Fair | 10 to 14 | Most | Mouth, tongue, nailbed |
| Polyglactin (Vicryl) | Good | Good | 30 | Minimal | Deep closure, nailbed, mouth |
| Polyglycolic acid (Dexon) | Best | Good | 30 | Minimal | Deep closure |
| Polydioxanone (PDS) | Fair | Best | 45 to 60 | Least | Deep closure |
| Polyglyconate (Maxon) | Fair | Best | 45 to 60 | Least | Deep closure |
Most wounds should be covered with an antibiotic ointment and a nonadhesive dressing immediately after laceration repair
- The dressing should be left in place for 24 hours, after which time most wounds can be opened to air.
Prophylactic antibiotics may decrease the risk of infection in some animal and human bites, intraoral lacerations, open fractures, and wounds that extend into cartilage, joints, or tendons
- Allow animal bites, especially in non-cosmetic areas such as the hand and foot are to heal by secondary intention
The sacrum and hip are most often affected. Reposition every 2 hours
- Stage 1: erythema of localized area, usually non-blanching over the bony surface
- Stage 2: partial loss of dermal layer, resulting in pink ulceration
- Stage 3: full dermal loss, often exposing subcutaneous tissue and fat
- Stage 4: full-thickness ulceration exposing bone, tendon, or muscle. Osteomyelitis may be present
Wound management by stage of the ulcer
- Stage I: aggressive preventive measures, thin-film dressings for protection
- Stage II: occlusive dressing to maintain healing, transparent films, hydrocolloids
- Stages III-IV: Débridement of necrotic tissue. Exudative ulcers will benefit from absorptive dressings such as calcium alginates, foams, and hydrofibers. Dry ulcers require occlusive dressing to maintain moisture, including hydrocolloids, and hydrogels.
Risk factors: age >65, impaired circulation, immobilization, undernutrition, incontinence
DX: based on observation and staged according to classification
TX: debridement ⇒ depends on the extent of necrosis; surgical closure may be necessary; vacuum-assisted closure uses negative pressure to reduce wound edema and remove debris/reduce bacterial load
Image: YOLO-Based Deep Learning Model for Pressure Ulcer Detection and Classification - Scientific Figure on ResearchGate by CC 4.0
Stasis dermatitis is caused by fluid buildup due to varicose veins, poor circulation, or heart disease
- Skin discoloration of the ankles or shins, itching, thickened skin, and open sores (ulcers) are symptoms
Treatments may include compression stockings and corticosteroid creams, as well as treating the underlying condition
- Systemic antibiotics for patients with more extensive infection and signs of cellulitis


