AC Joint Separation
|
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now. |
AC Joint SeparationPatient will present as → a 25-year-old male, a recreational soccer player, presents with acute pain in his right shoulder following a fall onto his outstretched hand during a soccer match two days ago. He reports immediate pain and swelling in the shoulder, with difficulty lifting his arm due to pain. He has not experienced any numbness or tingling in the arm. On physical examination, there is noticeable swelling and tenderness over the acromioclavicular (AC) joint. There is a visible step-off at the AC joint, suggestive of a possible separation. Pain is exacerbated with cross-body adduction and during the O’Brien’s test. Range of motion is limited, especially with abduction and forward elevation due to pain. Neurovascular examination of the upper extremity is normal. Radiographic imaging of the shoulder reveals widening of the AC joint space. The patient is diagnosed with a Grade II AC joint separation. Management includes a brief period of immobilization with a sling to allow for pain control and healing, followed by early range-of-motion exercises as tolerated. The patient is advised to avoid heavy lifting and overhead activities. Anti-inflammatory medications are prescribed for pain management. The patient is referred to physical therapy for shoulder stabilization and strengthening exercises. He is counseled about the importance of adhering to the rehabilitation protocol to ensure proper healing and prevent chronic instability or dysfunction. A follow-up appointment is scheduled in two weeks to evaluate his progress and to adjust the treatment plan if necessary. |
An AC joint separation involves damage to the ligaments supporting the AC joint, either sprains or tears, commonly caused by a fall on the shoulder or outstretched hand. This can result in pain, shoulder deformity, and loss of forelimb mobility.
DX: X-rays - Anteroposterior X-rays of both sides of the clavicle are taken
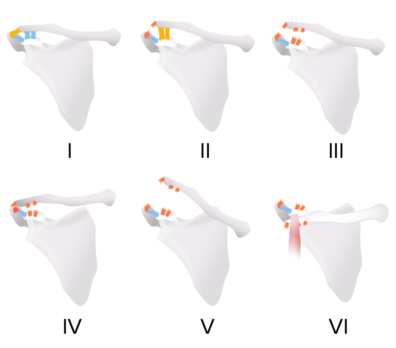
Acromioclavicular joint sprains are classified based on x-ray findings:
TX: Conservative management is possible for mild to moderate injuries because they can be managed with a sling and analgesia
References: Merck Manual · UpToDate |
Biceps Tendonitis
|
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now. |
Biceps TendonitisPatient will present as → a 33-year-old man who complains of left anterior shoulder pain for 4 weeks. The pain is made worse with overhead activities. On examination, you note maximal pain in the shoulder with palpation between the greater and lesser tubercle. Pain in the shoulder is exacerbated when the arm is held at the side, elbow flexed to 90 degrees, and the patient is asked to supinate and flex the forearm against your resistance. |
Biceps tendinitis is an inflammation or irritation of the upper biceps tendon. Also called the long head of the biceps tendon, this strong, cord-like structure connects the biceps muscle to the bone in the shoulder socket
Provocative factors:
DX: X-ray to rule out a fracture
TX: Treat with Rest (immobilize in sling), NSAIDs, PT strengthening, and steroid injections
Special tests: Speed test: Pain elicited in the bicipital groove when the patient attempts to forward elevate shoulder against examiner resistance while the elbow is extended and forearm supinated. Positive if the pain is reproduced. It may also be positive in patients with SLAP lesions. Yergason’s test: Elbow flexed 90 degrees, wrist supination against resistance. Positive if the pain is reproduced. Yergason’s Test Video Speed's Test VideoReferences: Merck Manual · UpToDate |
Rotator cuff tendinopathy/tear
|
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now. |
|||||||||
Rotator cuff tendinopathy and tearPatient will present as → a 69-year-old male with right shoulder pain for the past several months. He reports that he cannot reach above his head without severe pain. As a retired carpenter, he reports that this has significantly impacted his quality of life. Additionally, he is unable to lie on his left side at night due to shoulder pain. On physical exam, there is focal tenderness over the left anterolateral shoulder. Radiography reveals reduced space between the acromion and humeral head. |
|||||||||
A patient will present with → shoulder pain with overhead activity or at night when lying on the arm or weakness and immobility after acute injury
DX: Radiography for all patients as initial imaging - loss of subacromial space due to upward migration of humeral head
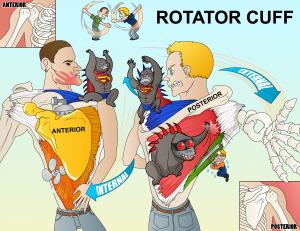
TX: Treat with physical therapy (for all patients), NSAIDs, steroid injections, and surgical repair for patients with complete tears or for those who fail 3-6 months of conservative management There are 4 muscles in the rotator cuff (SITS)
Supraspinatus tear or inflammation:
Subscapularis tear or inflammation:
Teres minor/infraspinatus tear or inflammation:
References: Merck Manual · UpToDate
Which of the following rotator cuff tendons is most likely to sustain injury because of its repeated impingement (impingement syndrome) between the humeral head and the undersurface of the anterior third of the acromion and coracoacromial ligament?
Question 1 Explanation: A critical zone exists for the supraspinatus tendon due to its superior insertion site. It is susceptible for injury because it has a reduction in its blood supply that occurs with abduction of the arm. Impingement of the shoulder is most commonly seen with the supraspinatus tendon, the long head of the biceps tendon and/or the subacromial bursa.
There is 1 question to complete.
|
 Osmosis Osmosis |
|
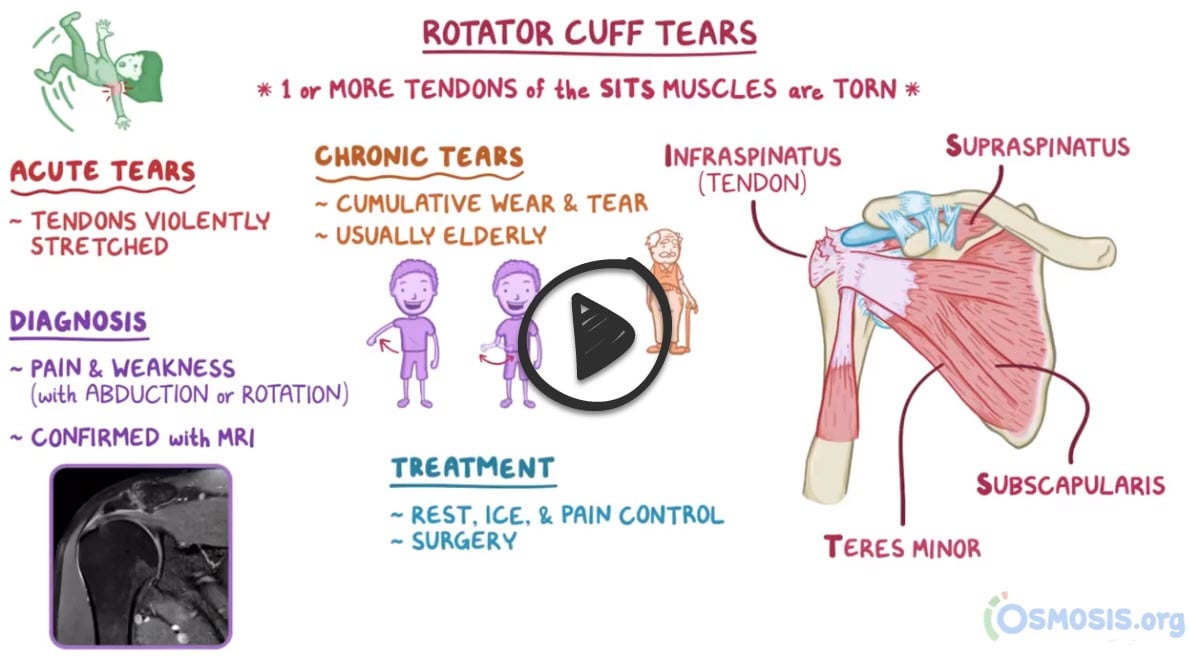 |
The rotator cuff is a group of muscles and tendons which act to stabilize the shoulder. It is comprised of four muscles, the supraspinatus, infraspinatus, teres minor and subscapularis. External rotation is done with the teres minor and infraspinatus, while internal rotation is controlled by the subscapularis. Abduction of the arm occurs through flexion of the supraspinatus.
Play Video + QuizAdhesive Capsulitis - AKA frozen shoulder
|
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now. |
Adhesive Capsulitis (frozen shoulder)Patient will present as → a 52-year-old female presents with a six-month history of progressive shoulder pain and stiffness. She reports that the pain is constant, worsens at night, and is aggravated by movements, especially when reaching overhead or behind her back. She also notes a significant reduction in her shoulder’s range of motion. The patient mentions a history of type 2 diabetes and a sedentary lifestyle. On examination, there is noticeable restriction in both active and passive range of motion of her left shoulder, particularly in external rotation and abduction. There is no apparent joint instability or muscle weakness, and the neurovascular examination is normal. No history of trauma or prior shoulder pathology is reported. Based on these findings, a diagnosis of adhesive capsulitis, also known as frozen shoulder, is considered. The patient is advised to begin a regimen of physical therapy focusing on shoulder mobilization exercises and stretching. She is also prescribed nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management. The importance of diabetes control and regular follow-up is emphasized to monitor her progress and modify the treatment plan as necessary. |
Frozen shoulder, also called adhesive capsulitis, is a painful condition in which the movement of the shoulder becomes limited. A frozen shoulder occurs when the strong connective tissue surrounding the shoulder joint (called the shoulder joint capsule) becomes thick, stiff, and inflamed
DX: Frozen shoulder is a clinical diagnosis made on the basis of medical history and physical examination
TX: NSAIDs, physical therapy, and intra-articular steroid injections
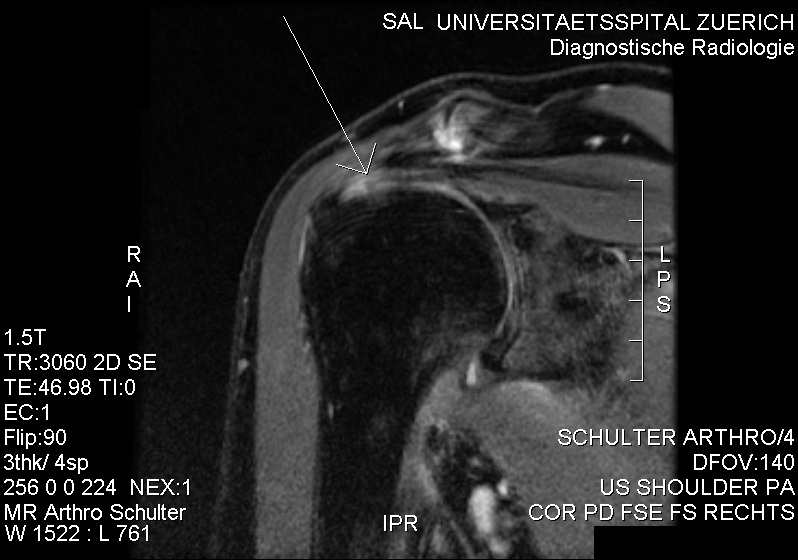 MRI with suspicion of frozen shoulder due to minor intraarticularly injectable contrast agent. No contrast agent at the bursa subacromialis and subdeltoidea. References: UpToDate |
Impingement
Shoulder impingement syndromePatient will present as → a 70-year-old male with an insidious onset of left shoulder pain that is exacerbated by overhead activities and while lifting objects away from his body. He is a retired mechanic of 35 years. The patient reports that over the last several months, he has been having difficulty sleeping because of the pain. On physical examination, there is notable tenderness over the left anterolateral shoulder, and passive forward flexion >90° causes severe pain. An x-ray reveals proximal migration of the humeral head and calcification of the coracoacromial ligament. Based on these findings, a diagnosis of shoulder impingement syndrome is considered. Conservative management is initiated with NSAIDs for pain relief, rest, and modification of activities to avoid overhead motions. The patient is referred to physical therapy for rotator cuff and scapular stabilizer strengthening exercises, and postural correction. Instructions are given on the importance of gradual return to sports and the potential need for further intervention, such as a subacromial injection or, rarely, surgical decompression, if symptoms do not improve with conservative management. A follow-up appointment is scheduled to assess progress and response to treatment. |
Subacromial impingement syndrome (SAIS) refers to the inflammation and irritation of the rotator cuff tendons as they pass through the subacromial space
DX: X-ray may show tendonc calcification or a subacromial spur
TX: Treatment involves rest, ice, activity modification, NSAIDs, and corticosteroid injections
References: UpToDate |
Shoulder Bursitis
Subacromial BursitisPatient will present as → a 45-year-old male, an avid tennis player, presents with a three-month history of right shoulder pain. He describes the pain as a constant, dull ache, worsening with overhead activities and at night, especially when lying on the affected side. He denies any history of trauma but mentions that his pain began after intensifying his tennis training. On physical examination, there is tenderness to palpation over the lateral aspect of the right shoulder, and pain is exacerbated by abduction and internal rotation of the arm. The Neer and Hawkins tests elicit pain, while the rotator cuff strength remains intact. There is no evidence of joint instability or neurological deficits. Based on the clinical presentation, a diagnosis of subacromial bursitis is suspected. The patient is advised to modify his activities, especially reducing overhead movements. He is prescribed a course of nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation, and referred for physical therapy focusing on shoulder strengthening and range of motion exercises. A follow-up appointment is scheduled to reassess his condition and consider further interventions, such as corticosteroid injections, if there is no improvement with conservative management. |
Subacromial bursitis is a common etiology of shoulder pain. It results from inflammation of the bursa, a sac of tissue present under the acromion process of the shoulder
DX: Diagnosis is by history and physical examination, including provocative maneuvers
TX: Includes prevention of the precipitating factors, rest, and NSAIDs. Cortisone injections can be helpful 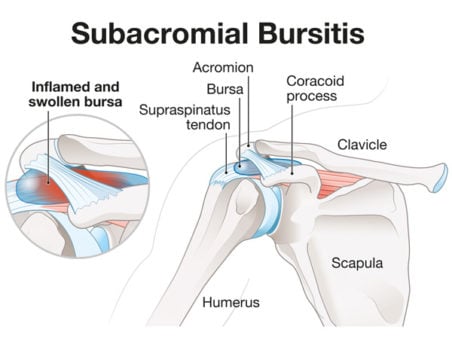 The subacromial bursa sits in a tight space under the acromion process of the shoulder, making it susceptible to overuse injury.
References: Merck Manual · UpToDate |
Glenohumeral Joint Osteoarthritis
Glenohumeral Joint OsteoarthritisPatient will present as → a 67-year-old female with a history of type 2 diabetes and hypertension presents complaining of progressive right shoulder pain over the past year. She describes the pain as a deep, aching sensation, worsening with movement and at night, leading to disturbed sleep. She notes decreased range of motion and difficulty in performing daily activities, such as reaching overhead and behind her back. She denies any history of injury to the shoulder. On examination, there is noticeable crepitus with passive movement of the right shoulder, tenderness to palpation over the glenohumeral joint, and a limited range of motion, particularly in external rotation and abduction. There are no signs of acute inflammation or systemic illness. Radiographic imaging of the shoulder reveals joint space narrowing, osteophyte formation, and subchondral sclerosis, consistent with osteoarthritis. Based on these findings, a diagnosis of primary glenohumeral joint osteoarthritis is made. The patient is advised on activity modification, provided with a prescription for NSAIDs for pain management, and referred to physical therapy for strengthening and range of motion exercises. Intra-articular corticosteroid injections are discussed as a potential option for pain relief. The patient is also educated about the possibility of future surgical interventions, such as shoulder arthroplasty, should conservative measures fail to provide adequate relief. Regular follow-up is scheduled to monitor her symptoms and functional status. |
Degenerative shoulder (glenohumeral) osteoarthritis is characterized by degeneration of articular cartilage and subchondral bone with narrowing of the glenohumeral joint
DX: Radiographs demonstrate joint space narrowing, subchondral sclerosis, and osteophytes at the inferior aspect of the humeral head
TX: NSAIDs, physical therapy, corticosteroid injections
References: Merck Manual · UpToDate |
Question 1 |
rotator cuff tendonitis | |
myocardial infarction | |
anterior shoulder dislocation | |
rotator cuff tear | |
bicipital tendonitis |
Question 2 |
infraspinatus tendon | |
supraspinatus tendon | |
teres minor tendon | |
subscapularis tendon | |
bicipital tendon |
|
List |