8-year-old with a non-healing wound on the leg
Patient will present as → a 12-year-old girl brought to the clinic by her parents concerning a persistent, dull pain in her left leg that worsens with movement. She also has had a fever for the past three days. Her parents note that she had a puncture wound on the same leg about two weeks ago while playing near a construction site. On examination, the child is irritable, the left leg is swollen, and there is tenderness over the tibia. The overlying skin is warm and erythematous. Laboratory results reveal an elevated white blood cell count, and ESR and CRP levels are also high. An MRI of the leg demonstrates demineralization, periosteal thickening, and bone destruction. Blood cultures are taken, and empirical intravenous antibiotic therapy is initiated.[
Osteomyelitis is an acute or chronic infection and inflammation of bone and bone marrow – it can occur as a result of hematogenous seeding, the contiguous spread of infection, or direct inoculation into intact bone (trauma/surgery)
- Fever, restriction of movement of the involved extremity or refusal to bear weight, pain or tenderness in the infected area, and signs of localized inflammation
- In patients with diabetes, classic signs and symptoms of infection may be masked due to vascular disease and neuropathy
- Staphylococcus aureus - most common cause overall
- Pasteurella multocida - seen in cases caused by cat and dog bites
- Salmonella spp. in patients with sickle cell
- Mycobacterium tuberculosis - can also be seen in cases of vertebral involvement (Pott disease)
Routine radiography is standard 1st-line imaging
- Classic X-ray triad of demineralization, periosteal reaction, and bone destruction
- Radiographic evidence of osteomyelitis lags behind symptoms and pathologic changes by 7 to 10 days
- Magnetic resonance imaging (MRI) shows the changes before plain-film radiography or bone scan
Labs: CRP is usually elevated but nonspecific. WBC and ESR are high in most cases
- A persistently elevated CRP (4–6 weeks) can be associated with persistent osteomyelitis
- Definitive diagnosis is made by blood cultures or by needle aspiration/bone biopsy
Empiric therapy should be directed toward the most probable organism and tailored once cultural results are available. All hardware (if post-op) needs to be removed
- Duration of therapy: 4–6 weeks for acute osteomyelitis and generally >8 weeks for chronic osteomyelitis or MRSA infection
- If a diabetic foot ulcer is larger than 2 x 2 cm or the bone is palpable, osteomyelitis is likely
 Osmosis Osmosis |
|
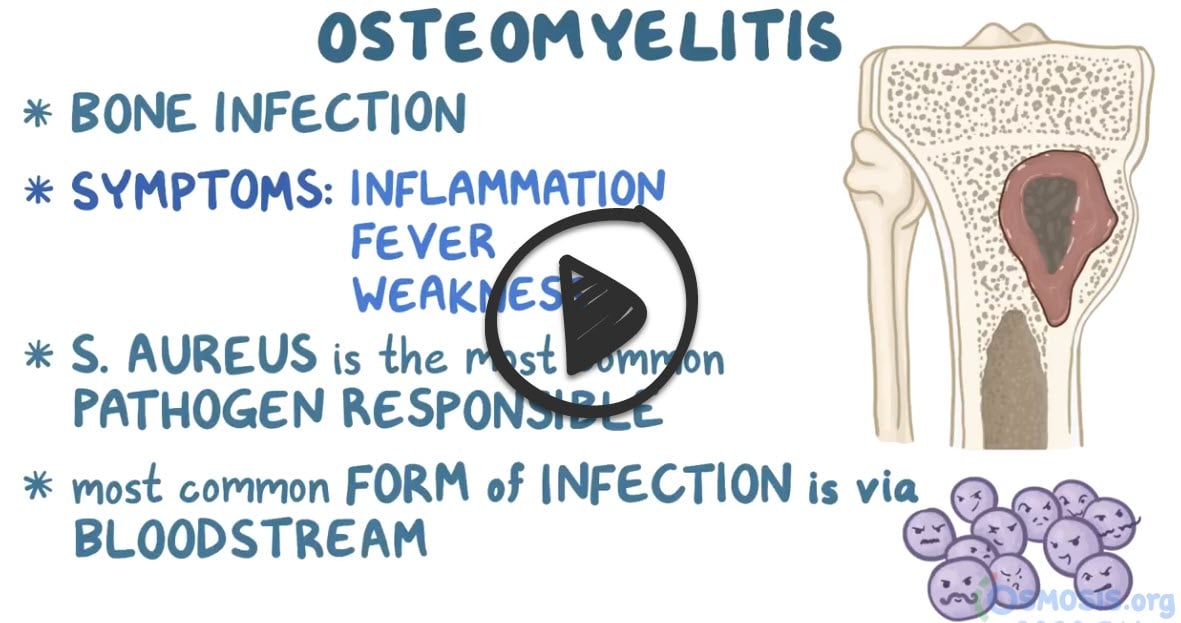 |
 Osteomyelitis is an infection of the bone that also affects the bone marrow and surrounding soft tissue. Staphylococcus aureus is the most common offending organism, although other organisms may cause osteomyelitis as well. Osteomyelitis persisting longer than one month is considered chronic. Patients with this condition experience constant bone pain that is unrelieved by rest and is worsened with activity. Other symptoms of osteomyelitis include local warmth and edema at the site of infection, fever, chills, nausea, night sweats, and restlessness. Treatment of osteomyelitis includes antibiotic therapy and surgical removal of poorly vascularized tissue and/or necrotic bone. Hyperbaric oxygen may also be used in patients with chronic osteomyelitis that is refractory to treatment.
Osteomyelitis is an infection of the bone that also affects the bone marrow and surrounding soft tissue. Staphylococcus aureus is the most common offending organism, although other organisms may cause osteomyelitis as well. Osteomyelitis persisting longer than one month is considered chronic. Patients with this condition experience constant bone pain that is unrelieved by rest and is worsened with activity. Other symptoms of osteomyelitis include local warmth and edema at the site of infection, fever, chills, nausea, night sweats, and restlessness. Treatment of osteomyelitis includes antibiotic therapy and surgical removal of poorly vascularized tissue and/or necrotic bone. Hyperbaric oxygen may also be used in patients with chronic osteomyelitis that is refractory to treatment.
| Osteomyelitis | Play Video + Quiz |
| Staphylococcus aureus | Play Video + Quiz |
| Salmonella | Play Video + Quiz |
Question 1 |
Start empiric antibiotics immediately Hint: Starting antibiotics without a confirmed diagnosis can make it difficult to later establish the diagnosis of osteomyelitis through culture. | |
Obtain blood cultures and start empiric antibiotics Hint: Blood cultures are generally not useful in cases of nonhematogenous osteomyelitis, which is more likely in this patient given his diabetic foot ulcer. | |
Proceed to magnetic resonance imaging (MRI) of the foot | |
Perform bone biopsy for culture and histology Hint: While bone biopsy is the gold standard for diagnosing osteomyelitis, it is generally performed after imaging studies have suggested the presence of osteomyelitis. | |
Refer the patient for surgical debridement Hint: Surgical debridement is a therapeutic option but should be based on confirmatory diagnostic tests like MRI and bone biopsy. |
Question 2 |
Start a prolonged course of intravenous vancomycin for six weeks Hint: A prolonged course is generally reserved for patients with residual infected bone or those with orthopedic hardware. | |
Start a short course of oral antibiotics for two weeks Hint: Intravenous antibiotics are preferred initially for better bioavailability and efficacy. | |
Start a short course of intravenous antibiotics for two weeks | |
Start intravenous vancomycin and add rifampin Hint: Rifampin is generally added for patients with retained hardware and methicillin-sensitive or methicillin-resistant S. aureus osteomyelitis. | |
Long-term antibiotic suppression with an oral agent Hint: This approach is generally reserved for patients with retained hardware and/or necrotic bone not amenable to debridement. |
|
List |
References: Merck Manual · UpToDate





