85 y/o with Rib pain (4/10) that is worse with deep breathing
Patient will present as → a 29-year-old man presents to the ED with a stab wound to the left chest lateral just below the nipple. The paramedics report that he had been writhing in pain in the ambulance. His blood pressure is 78/50 mmHg, pulse is 125/min, and respirations are 23/min. Tube thoracostomy is performed in the left chest at the fifth intercostal space. About 1,600 ml of blood is evacuated immediately, but the patient continues to lose blood.
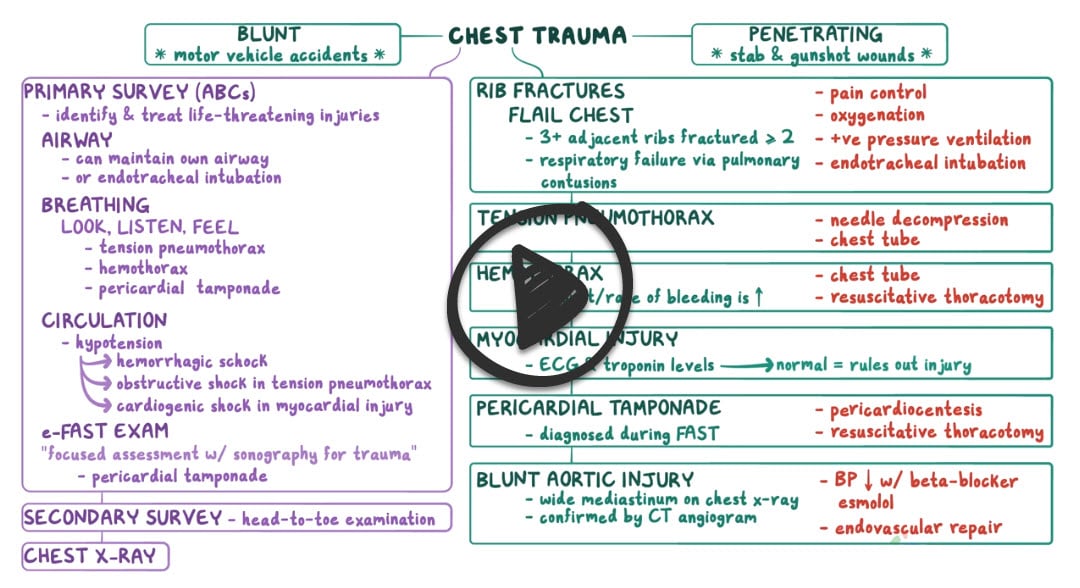
Thoracic trauma can be distinguished by the mechanism of injury
Blunt trauma refers to mechanisms causing increased intrathoracic pressure, such as car collisions (the most common cause of thoracic trauma) and falls
- Rib fractures are the most common blunt thoracic injuries. Ribs 4-10 are most frequently involved. Patients usually report inspiratory chest pain and discomfort over the fractured rib or ribs. Physical findings include local tenderness and crepitus over the site of the fracture.
- Flail chest involves three or more consecutive rib fractures in two or more places, which produce a free-floating, unstable segment of the chest wall
- Sternal fractures cause pain, tenderness, bruising, and swelling over the fracture site. CPR has also been known to cause thoracic injury
- Pulmonary contusion resulting from blunt trauma to the chest causing interstitial edema that impairs compliance and gas exchange
- Ruptured diaphragm - should be considered in patients who sustain a blow to the abdomen and present with dyspnea or respiratory distress
- Blunt myocardial injury - dysrhythmias, ST changes
- Pneumothoraces in blunt thoracic trauma are most frequently caused when a fractured rib penetrates the lung parenchyma
Penetrating trauma largely refers to gunshot and stab wounds, occasionally impalement
- Hemothorax - blood in the chest cavity
- Pneumothorax- air in the chest cavity
- Hemopneumothorax - two conditions: pneumothorax (air in the chest cavity) and hemothorax (blood in the chest cavity)
- Ruptured diaphragm - CXR: abnormal peridiaphragmatic anatomy. CT scan and endoscopy if further workup needed
- Pulmonary contusion - CXR: opacification of the lung within 6 hours
- Rib fracture
- Subcutaneous emphysema - air trapped in subcutaneous tissue as a result of penetrating trauma
- Pneumomediastinum - abnormal presence of air in the mediastinum escaping from the lungs into the chest cavity
- Thoracic wall lacerations
- Sternal fracture
Symptoms:
- Pain in the chest that gets worse when laughing, coughing, or sneezing, deep inspiration, and overhead activities
- Difficulty breathing
- Tenderness, bruising, and swelling
Chest radiography remains the basis for initiating other investigations
- CT, aortography, bronchoscopy/endoscopy
- Hemoglobin or hematocrit values and arterial blood gas determinations offer the most useful information for treating these patients
- ECG
- Bone scan may be indicated when x-rays are negative and clinical suspicion remains
Treatment involves immediate airway management: intubate early if airway compromise suspected
- Rib fractures - the majority heal uneventfully with rest, analgesia, cessation of inciting activity for ~4-6 weeks
- Needle thoracostomy - Use a large bore needle at 2nd intercostal space in the midclavicular line - the best initial step in the management of tension pneumothorax
- Tube thoracostomy - chest tube at 5th intercostal space in anterior axillary line - next step in management after needle placement in tension pneumothorax
- Oxygenation - positive pressure ventilation for flail chest
- Thoracotomy indications - > 1500 ml total blood loss or > 200 ml/hour continued drainage of blood for > 3 hours
- Surgical repair as needed
 Osmosis Osmosis |
|

|
Tension pneumothorax is characterized by intrapleural pressure that is greater than the atmospheric pressure. It presents with sudden deterioration, hypotension, jugular venous distention, and no breath sounds. It is most commonly due to positive pressure mechanical ventilation.
Play Video + QuizSpontaneous pneumothorax
Spontaneous pneumothorax occurs due to the rupture of a subpleural emphysematous bleb that leads to the accumulation of air in the pleural space. It is more common in tall and thin young males.
Question 1 |
Cardiac tamponade Hint: See B for explanation | |
Flail chest | |
Pulmonary contusion Hint: See B for explanation | |
Tension pneumothorax Hint: See B for explanation |
Question 2 |
Acute respiratory distress syndrome Hint: Acute respiratory distress syndrome would present with sudden and severe shortness of breath secondary to trauma, sepsis, overdose, transfusion, pancreatitis, or aspiration. Patients are typically critically ill with multisystem organ failure and radiography will demonstrate diffuse bilateral involvement with ground glass changes and frank alveolar infiltrates. In the setting of blunt chest trauma in a young patient with the radiography provided, a pulmonary contusion is a more likely diagnosis; however, acute respiratory distress syndrome should certainly be considered.
| |
Cardiac contusion Hint: Cardiac contusion would present after blunt chest trauma and could present with chest pain, shortness of breath, ECG changes, and an elevated troponin. While this patient’s initial trauma may have led to this presentation, her absence of ECG findings, normal troponins, and pulmonary infiltrates on radiology suggest an alternative diagnosis.
| |
Hemothorax
Hint: Hemothorax would present with pulmonary decompensation after trauma with a unilateral accumulation of radiopaque fluid in the lung rather than diffuse, patchy, and irregular alveolar infiltrates. A chest tube should promptly be placed to drain the hemothorax, and surgery may be needed for persistent or severe bleeding.
| |
Pneumonia
Hint: Pneumonia presents with a cough, fever, pulmonary crackles, and a lobar consolidation on chest radiography and would not be associated with trauma. Aspiration pneumonia could be seen after trauma; however, it would not manifest hours later with diffuse and bilateral infiltrates. | |
Pulmonary contusion |
|
List |
References: Merck Manual · UpToDate