19-year-old with a history of pneumothorax and chest pain
Patient will present as → a 19-year-old male transported to the ED following a car crash. Upon arrival, he is alert and anxious and appears to be in respiratory distress. A quick assessment reveals that she sustained trauma to his face, neck, and chest. His left hemithorax appears to be expanding more than the right. He is receiving oxygen via a nonrebreathing mask. His vital signs are: respiratory rate 36 and labored. SpO2 is 85%. On physical exam, you notice decreased tactile fremitus, deviated trachea, hyperresonance, and diminished breath sounds.
Listen to his left lung field
Listen to his right lung field
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
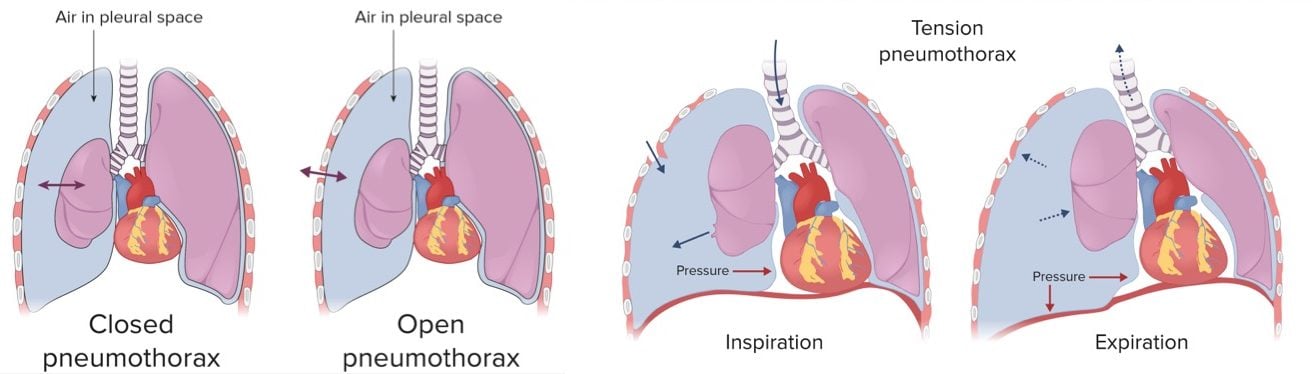
Pneumothorax is the accumulation of air in the pleural space
- Common symptoms include acute onset of ipsilateral chest pain and dyspnea with decreased tactile fremitus, deviated trachea, hyperresonance, and diminished breath sounds
Pneumothorax can be either spontaneous or traumatic
- Spontaneous (primary pneumothorax)
- Primary: occurs in the absence of underlying disease - tall, thin males between 10 and 30 years of age are at greatest risk of primary pneumothorax
- Secondary: occurs in the presence of underlying disease - asthma, COPD, cystic fibrosis, interstitial lung disease
"Spontaneous pneumothorax recurs in 30% of patients usually within 2 years. Treatment in recurrent episodes is either administration of a noxious agent into the pleural space to obliterate the pleural space or partial pleurectomy with oversewing of apical blebs or abrasion of the pleural space"
Traumatic occurs after penetrating or blunt trauma
- Tension from penetrating trauma, CPR, mechanical ventilation - pneumothorax is secondary to a sucking chest wound that allows air to enter the chest with inspiration but does not allow air to leave on expiration.
Pneumothorax is characterized by the acute onset of ipsilateral chest pain and dyspnea
- Physical findings depend on the size of the pneumothorax and may include unilateral chest expansion, decreased tactile fremitus, hyperresonance, and diminished breath sounds
- Tension pneumothorax is associated with a mediastinal shift to the contralateral side and impaired ventilation, leading to cardiovascular compromise
- Tension pneumothorax → penetrating injury → air in pleural space increasing and unable to escape
- Tension pneumothorax is associated with a mediastinal shift to the contralateral side and impaired ventilation, leading to cardiovascular compromise
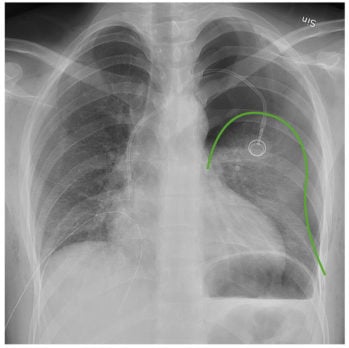
The diagnosis of pneumothorax is a radiologic one:
- Those who are unstable should have rapid bedside imaging with pleural ultrasonography (highly sensitive and specific)
- Those with a stable presentation can wait for confirmation by chest radiography - expiratory chest film reveals pleural air
- CT for those with uncertain dx, suspected to have a loculated pneumothorax, or stable trauma patients who require CT to assess the extent of other injuries
- ABG analysis, if done, reveals hypoxemia
Management:
- Small pneumothoraces <15% of the diameter of the hemithorax will resolve spontaneously without the need for chest tube placement
- For large, > 15% of the diameter of hemithorax, and symptomatic pneumothoraces, chest tube placement is performed
- Patients should be followed with serial CXR every 24 hours until resolved
"If a pneumothorax is small but the patient is mildly symptomatic or unlikely to cooperate with follow up (i.e. homeless alcoholic) admit the patient and administer high-flow oxygen. The resulting nitrogen gradient will speed resorption."
Tension pneumothorax is a medical emergency
- If it is suspected, a large bore needle should be inserted through the chest wall to allow air to move out of the chest
- Placement of a chest tube follows the decompression
 Osmosis Osmosis |
|
 |
Tension pneumothorax is characterized by intrapleural pressure that is greater than the atmospheric pressure. It presents with sudden deterioration, hypotension, jugular venous distention, and no breath sounds. It is most commonly due to positive pressure mechanical ventilation.
Play Video + QuizSpontaneous pneumothorax
Spontaneous pneumothorax occurs due to the rupture of a subpleural emphysematous bleb that leads to the accumulation of air in the pleural space. It is more common in tall and thin young males.
Question 1 |
order a V/Q scan Hint: A V/Q scan is indicated in suspected cases of pulmonary embolism. | |
order a chest x-ray Hint: Patients in respiratory distress and evidence of a tension pneumothorax, such as tracheal deviation, should have treatment initiated without waiting on a chest x-ray to be taken. | |
administer a sclerosing agent Hint: Pleurodesis by administration of a sclerosing agent is indicated in treatment of recurrent, not traumatic, pneumothorax. | |
insert large bore needle into left 2nd ICS stat |
Question 2 |
Penetrating or blunt trauma forces Hint: Penetrating or blunt trauma force is responsible for a traumatic pneumothorax. | |
Underlying lung cancer Hint: A pneumothorax that results from an underlying lung disease is classified as a secondary pneumothorax. | |
Pressure of air in the pleural space exceeds room air pressure Hint: When pressure of air in the pleural space exceeds room air pressure, it leads to a tension pneumothorax. | |
Rupture of subpleural apical blebs due to high negative intrapleural pressures |
Question 3 |
Surgical fixation of the fractured ribs Hint: Surgical fixation of flail chest is less reliable than positive-pressure ventilation and is performed only rarely in the United States.
| |
Application of elastic binders and adhesive tape Hint: While application of elastic binders and adhesive tape was historically utilized to stabile the chest, this intervention has been found to decrease chest expansion and worsen lung atelectasis. | |
Endotracheal intubation and mechanical ventilation | |
Chest physiotherapy that encourages frequent coughing Hint: Conservative treatment for mild to moderate flail chest includes analgesic relief of pain, chest physiotherapy that encourages frequent coughing and restriction of fluids to prevent fluid overload, however this patient needs early ventilatory support. |
Question 4 |
Hemothorax Hint: A hemothorax usually results from trauma. While breath sounds would be absent over the involved area, the percussion note would be dull, not hyperresonant. | |
Pneumothorax | |
Pulmonary embolus Hint: While a pulmonary embolism most commonly presents with dyspnea and pain on inspiration, the physical examination is often unremarkable and would not reveal the findings of absent breath sounds and hyperresonance to percussion. | |
Foreign body aspiration Hint: Foreign body aspiration is most common in children and the elderly. Aspiration of a food bolus is the most common cause in adults which leads to a history of a choking episode followed by dysphagia, wheezing and coughing. Physical examination findings are dependent on the location of the obstruction. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture