The NCCPA™ PANCE and PANRE Genitourinary Content Blueprint requires lists two types of fluid and electrolyte disorders
| Hyponatremia / Hypervolemia
Disorders of water excess = increased free water = decreased serum sodium = hyponatremia |
Definition: serum sodium of < 135 mmol/L
Peripheral and presacral edema, pulmonary edema, JVD, hypertension, decreased hematocrit, decreased serum protein, decreased BUN/CR Causes:
Presentation:
Treatment:
Serum Na should be corrected slowly—by ≤ 10 mEq/L over 24 h to avoid osmotic demyelination syndrome |
||||||||
|
|||||||||
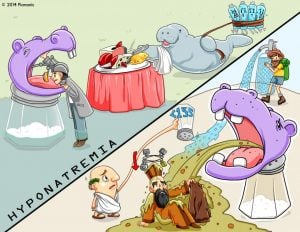 |
Hyponatremia is a low serum sodium level less than 135 mEq/L. This causes a shift of fluid volume from the extracellular fluid to the intracellular fluid resulting in cellular swelling and reduced excitable depolarization of cells. Many things cause may precipitate hyponatremia including actual sodium deficits or relative sodium deficits. Some relative causes include water intoxication (water excess) which results in a hypoosmolar imbalance. An additional assessment is done to determine if the patient has hyponatremia related to fluid overload or a fluid deficit, as these conditions manifest slightly differently.
Play Video + Quiz
|
Disorders of water deficiency = decreased free water = increased serum sodium = hypernatremia
Etiology: Diarrhea, burns, diuretics, hyperglycemia, diabetes insipidus, a deficit of thirst
Poor skin turgor, dry mucous membranes, flat neck veins, hypotension, increased BUN/CR ratio > 20:1
- Decrease circulating volume = decrease of flow to kidneys means more bound urea in the blood, which means ↑ BUN
Treatment: intravenous (IV) 5% dextrose in water (D5W)
- Rapid overcorrection causes cerebral edema and pontine herniation
Diabetes insipidus - Low urine sodium (but high serum sodium) and polyuria usually indicate diabetes insipidus
- Neurogenic (central) is caused by deficient secretion of vasopressin (ADH - anti-piss-hormone) from the posterior pituitary
- Nephrogenic DI is caused by kidneys that are unresponsive to normal vasopressin levels - usually inherited X-linked or from lithium or renal disease
- Urine osmolality of less than 250, despite hypernatremia, indicated Diabetes Insipidus
 Picmonic
Picmonic
 |
Hypernatremia is characterized by a serum sodium level above the normal range of 145 mEq/L. Hypernatremia is an increase in osmolarity of the extracellular fluid volume (ECF). This may be attributed to an actual sodium excess in the ECF like hyperaldosteronism or a relative sodium excess which is caused by a decrease of free water in the ECF like dehydration. High serum sodium levels causes a fluid shift from the intracellular fluid volume (ICF) to the ECF. This causes cellular shrinking. Hypernatremia should be assessed along with fluid balance as it often is associated with a fluid excess or deficit. |
Causes:
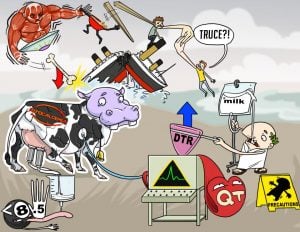
- Seen in the late stages of kidney failure, stage 5
- Can be seen in spironolactone and ACEI use and acute renal failure
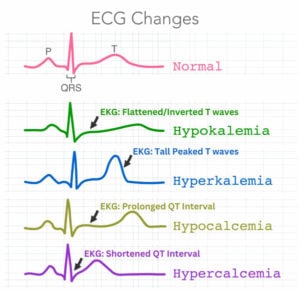
Presentation: Peaked T waves prolonged QRS, muscle fatigue
Treatment: Insulin, sodium bicarbonate, and glucose. (drive potassium back into the cell). Calcium gluconate
(antagonize the effect of potassium on the heart)
Pearls: hyperkalemia with EKG changes must be treated immediately. The next progression is sine waves, V-tach, and V-Fib
 Picmonic
Picmonic
 |
Hyperkalemia is a condition in which a person's serum potassium level is higher than normal. It can result from a number of causes, such as severe tissue trauma, untreated Addison's disease, acute acidosis, misuse of potassium-sparing diuretics, or overdose with IV potassium. |
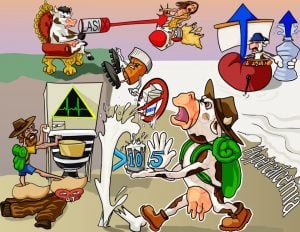
Causes:
- Overuse of diuretics
- Cushing’s syndrome
Presentation: Muscle cramps, constipation, flattened/inverted T waves, U waves
Treatment
- Potassium repletion
- remember to NOT use dextrose-containing fluids as this will stimulate insulin release and shift potassium within the cell, which worsens the hypokalemia
- Replace magnesium in magnesium deficiency
 Picmonic
Picmonic
 |
Hypokalemia is defined as low serum potassium levels with the most common cause being from loop or thiazide diuretic use. Other causes include insufficient potassium intake, alkalosis, excessive insulin, increased renal excretion of potassium, and potassium loss from vomiting, diarrhea, and abuse of laxatives. |
- Serum total calcium < 8.4 mg/dL
- Ionized fraction of calcium < 4.4 mg/dL
Causes
- The most common cause is hypoparathyroidism
- Other causes
- Thyroid surgery (injuring the parathyroid gland)
- Renal disease
Presentation: QT prolongation, Trousseau’s sign, Chvostek’s sign
- Labs: ↓ Ca+ ↓ PTH ↑ phosphate
- EKG = Prolonged QT
Treatment: IV calcium gluconate or calcium chloride
Pearls:
- If suspicious of phosphorus or calcium imbalance, always order a PTH level
- Always remember it is the effect on the EKG that counts the most, not the serum levels
 Picmonic
Picmonic
 Hypocalcemia is defined as serum calcium < 8.5 mg/dL. Parathyroid hormone (PTH), albumin, vitamin D, magnesium, and phosphate are all involved in calcium homeostasis, and derangements in their levels can cause changes in total and active calcium levels. Acid-base changes due to medications or critical illness alter calcium-binding. Critical illness such as sepsis or severe burns also causes hypocalcemia through actions on calcium homeostasis and end-organ effects. Many medications, including calcium chelators, bisphosphonates, and chemotherapeutic agents can cause hypocalcemia through effects on calcium binding and homeostasis. Acute treatment begins with IV calcium gluconate, which is cardioprotective. Chronic hypocalcemia treatment includes calcium carbonate, calcium citrate, and oral vitamin D supplements. Finally, patients who are hypomagnesemia should have this electrolyte addressed. This is because hypomagnesemia can lead to decreased PTH secretion, leading to decreased availability of calcium. Hypocalcemia is defined as serum calcium < 8.5 mg/dL. Parathyroid hormone (PTH), albumin, vitamin D, magnesium, and phosphate are all involved in calcium homeostasis, and derangements in their levels can cause changes in total and active calcium levels. Acid-base changes due to medications or critical illness alter calcium-binding. Critical illness such as sepsis or severe burns also causes hypocalcemia through actions on calcium homeostasis and end-organ effects. Many medications, including calcium chelators, bisphosphonates, and chemotherapeutic agents can cause hypocalcemia through effects on calcium binding and homeostasis. Acute treatment begins with IV calcium gluconate, which is cardioprotective. Chronic hypocalcemia treatment includes calcium carbonate, calcium citrate, and oral vitamin D supplements. Finally, patients who are hypomagnesemia should have this electrolyte addressed. This is because hypomagnesemia can lead to decreased PTH secretion, leading to decreased availability of calcium. |
|
| Hypocalcemia Picmonic | Play Video + Quiz |
| Hypocalcemia Causes Picmonic | Play Video + Quiz |
| Hypocalcemia Treatments Picmonic | Play Video + Quiz |
- Serum total calcium > 10.5 mg/dL
- Ionized fraction of calcium > 5.6 mg/dL
Causes
The most common cause is hyperparathyroidism
- Sarcoidosis
- Tuberculosis
- Paget disease
- Metastatic cancers to bone (prostate, breast, ovarian, renal)
- Multiple myeloma
Presentation: “Stones, bones, abdominal groans, psychiatric moans,” EKG: shortened QT interval
- Blood: ↑ PTH, ↑ Calcium, ↓ phosphorus
- ionized calcium level (serum calcium can give you false information)
- Associated with malignancy and hyperparathyroidism
Treatment: IV normal saline and furosemide
Pearls: hypercalcemia in the elderly is cancer until proven otherwise
 Picmonic
Picmonic
Dysfunction of several pathways can lead to high levels of calcium circulating in the blood. Calcium homeostasis is regulated by calcium absorption in the intestines, bone turnover, and reabsorption and excretion of calcium in the kidneys. Bone resorption is stimulated by increased levels of vitamin D and parathyroid hormone (PTH). Calcium absorption in the intestines is stimulated by vitamin D and high calcium intake. Renal excretion of calcium is mediated by PTH and vitamin D, and can be affected by many disease states. Malignancy is another important cause of hypercalcemia due to direct osteolytic effects on bone as well as hormonal changes in calcium homeostasis. The treatment of hypercalcemia depends on the cause, severity, and comorbid conditions of the patient. It should be aimed at lowering the calcium level as well as correcting the underlying cause where possible. The level of plasma calcium and the rate of rise are both important in determining the severity of hypercalcemia and the need for treatment. Patients with asymptomatic mild hypercalcemia (<12 mg/dL) do not need immediate treatment. Adequate oral hydration is often sufficient for control and can be tried initially. A calcium level of 12-14 mg/dL warrants intervention if the elevation was acute or the patient is symptomatic. Patients with severe hypercalcemia of >14 mg/dL need emergent intervention to lower their plasma calcium. The initial treatment for severe hypercalcemia is a combination of volume expansion with normal saline, calcitonin, and a bisphosphonate. Definitive treatment often involves treating the underlying cause |
|
| Hypercalcemia Picmonic | Play Video + Quiz |
| Hypercalcemia Causes Picmonic | Play Video + Quiz |
| Hypercalcemia Treatments Picmonic | Play Video + Quiz |
Presentation: Muscle weakness, hyperreflexia, prolonged QT, PR and wide QRS, ventricular tachycardia, torsades de pointes
Treatment: IV magnesium sulfate (acute) or oral magnesium oxide (chronic)
 Picmonic
Picmonic
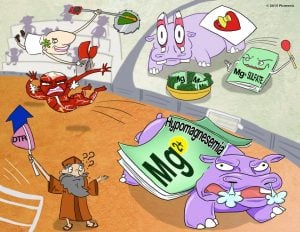 |
Hypomagnesemia occurs when serum magnesium levels are below 1.5 mEq/L. Causes of hypomagnesaemia include diarrhea, vomiting, chronic alcoholism, and malabsorption syndrome. Other causes include NG suction, poorly controlled diabetes mellitus, and hyperaldosterone. Magnesium is an intracellular cation used to activate enzymatic reactions and maintain normal calcium and potassium balance. Clinical manifestations of hypomagnesemia include confusion, increased deep tendon reflexes, insomnia, and tachycardia. The patient may exhibit neuromuscular irritability characterized by seizures, muscle cramps, and tremors. Treatment for hypomagnesemia includes administering IV magnesium sulfate and increasing dietary intake of foods high in magnesium. Play Video + Quiz |
Presentation: Muscle weakness, prolonged QT, PR and wide QRS
Treatment: IV isotonic saline, loop diuretics can be considered
 Picmonic
Picmonic
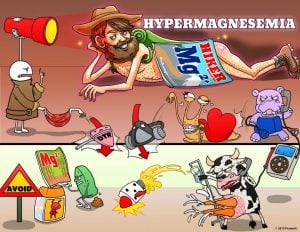 |
Hypermagnesemia occurs when the serum level of magnesium exceeds 2.5 mEq/L. This is caused by excess magnesium intake and renal insufficiency. Pregnant women receiving magnesium sulfate to manage symptoms of eclampsia are also at risk. Magnesium is an intracellular cation used to activate enzymatic reactions and maintain normal calcium and potassium balance. Symptoms of hypermagnesemia include flushing, lethargy, muscle weakness, and decreased deep tendon reflexes. The patient may also present with decreased respirations, bradycardia, and hypotension. Interventions to address hypermagnesemia include administering IV calcium gluconate and diuretics. Patients who are renally impaired may require dialysis. Medications containing magnesium, such as certain antacids and laxatives, should be avoided. Play Video + Quiz |
Etiology: Chronic kidney disease
Presentation: typically asymptomatic
Treatment: calcium carbonate, restrict potassium
Presentation: weakness, muscle and bone pain, osteomalacia, rickets
Treatment: IV phosphate replacement