Patient will present as → a 62-year-old female complaining of joint pain, polyuria, polydipsia, and generalized fatigue. The patient reports a history of recurrent kidney stones and depression. Radiographs show osteopenia and subperiosteal resorption on the phalanges (bones, stones, abdominal groans, and psychic moans).
Hyperparathyroidism is a condition in which one or more of the parathyroid glands become overactive and secrete too much parathyroid hormone (PTH). This causes the levels of calcium in the blood to rise
- Most patients with calcium levels < 12 are asymptomatic
- Symptoms usually begin as the calcium level rises above 12, and the symptoms will worsen as the calcium level continues to rise
- Initially, patients may complain of nausea and vomiting with a loss of appetite. They may feel muscle weakness and fatigue, and constipation may be present
- As the calcium level rises, they may become confused and lethargic. Polyuria can occur with renal failure. Cardiac arrhythmias can occur and even coma.
Hyperparathyroidism always = ↑ PTH
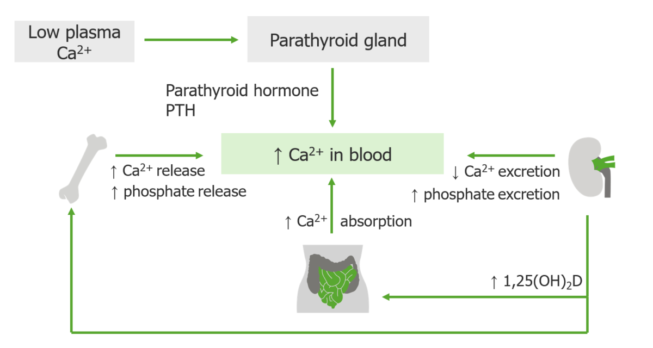
Parathyroid hormone has only one function: to correct hypocalcemia and maintain the serum level of calcium within narrow limits. If the serum calcium is low, the four parathyroid glands secrete PTH, which is made and stored in the glands. When released, PTH works with and through vitamin D to restore the calcium level to normal.
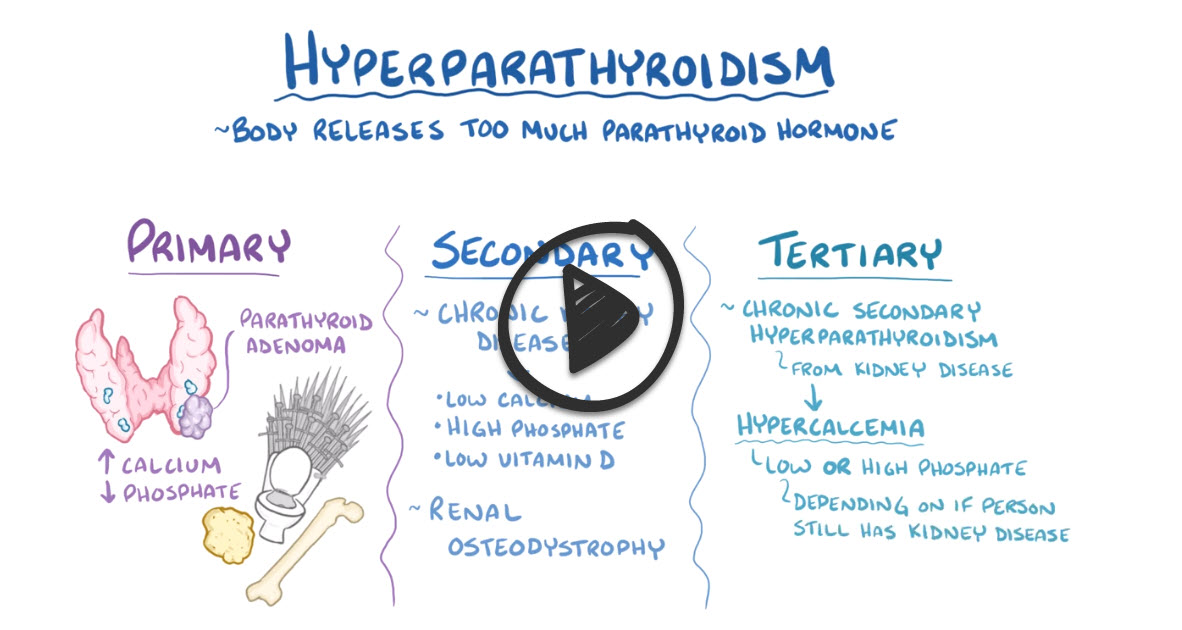
There are three types of hyperparathyroidism - primary, secondary, and tertiary
- Primary = ↑ PTH usually caused by a PTH secreting parathyroid ADENOMA
- Secondary =↑ PTH by a physiologic response to hypocalcemia or vitamin D deficiency. Chronic kidney disease is the most common cause of secondary hyperparathyroidism
- Tertiary hyperparathyroidism is a situation where individuals who have had secondary hyperparathyroidism for many years develop primary hyperparathyroidism. In tertiary hyperparathyroidism parts of the parathyroid gland start making parathyroid hormone independently of blood calcium levels - resulting in hypercalcemia.
The symptoms of primary hyperparathyroidism can be remembered as stones, thrones, bones, groans, and psychiatric overtones - Osteoporosis, renal calculi, bone pain, GI symptoms, depression, psychosis, fatigue
- Stones = for calcium-based kidney stones or gallstones that can form
- Thrones refers to the toilet to remind you of the polyuria or frequent urination that results from impaired sodium and water reabsorption
- Bones is for bone pain that results after chronic hormone-driven demineralization in order to release calcium
- Groans is for constipation and muscle weakness, both of which are partly due to decreased muscle contractions
- Psychiatric overtones refers to symptoms like a depressed mood and confusion
The symptoms of secondary hyperparathyroidism are the same four - ‘stones, thrones, bones, groans, and psychiatric overtones’ + bone resorption (osteodystrophy) + calcification in blood vessels and soft tissues, because the high levels of phosphate cause it to find and stick to any available calcium, which forms bone-like crystals in places that they shouldn’t be
Tertiary hyperparathyroidism causes all of the same symptoms, but can also have elevated phosphate levels and as a result deposits of calcium-phosphate can settle in blood vessels and soft tissues
| Serum Ca | Serum Phos | Serum PTH | |
| Primary | ↑ | ↓ | ↑ |
| Secondary | normal or ↓ | ↑ | ↑ |
| Tertiary | ↑ | ↑ | ↑ |
↑ Calcium is the most common metabolic abnormality associated with hyperparathyroidism
↑ PTH secretion from the parathyroid raises the blood calcium level by:
- Breaking down the bone (where most of the body's calcium is stored) and causing calcium release
- Increasing the body's ability to absorb calcium from food from the GI tract
- Increasing the kidney's ability to hold on to calcium that would otherwise be lost in the urine
This results in increased serum and urinary calcium, osteoporosis, and renal calculi.
Labs
- ↑ Calcium is the most common metabolic abnormality
- Blood: ↑ PTH, ↑ Calcium, ↓ phosphorus
- Urine: hyperphosphaturia, hypercalciuria this makes sense because all that calcium and phosphorus must go somewhere, so they go out through the kidneys and into the urine
- PTH inhibits the reabsorption of phosphate by the kidney. Therefore, with too much PTH there is less reabsorption of the phosphate leading to a low phosphate level in the blood
Remove the PARATHYROID adenoma, subtotal parathyroidectomy (3 1/2 of gland removed), or total parathyroidectomy
- If it is secondary, then once you replace the cause (Vitamin D and Calcium supplementation) you will have fixed the problem.
- If the calcium is very high - treat with IV fluids, furosemide, or calcitonin
- May need to treat osteoporosis with Bisphosphonates.
 Osmosis Osmosis |
|
 |
Primary Hyperparathyroidism is characterized by an increase in parathyroid hormone (PTH) secretion, which regulates serum calcium and phosphorus levels by stimulating bone resorption of calcium, renal tubular reabsorption of calcium, and the activation of Vitamin D.
Play Video + QuizParathyroid Gland Overview
The parathyroid gland is a series of four small glands located in the neck on the rear surface of the thyroid gland. It serves primarily in calcium homeostasis and has a blood calcium sensor that detects when blood calcium levels are abnormally low. It responds by releasing parathyroid hormone (PTH) which stimulates osteoclasts into action. Osteoclasts resorb bone and release a large amount of calcium. This calcium enters the blood and results in increased blood calcium levels. PTH can also activate vitamin D by promoting the activity of an enzyme that converts inactive vitamin D to active vitamin D
Question 1 |
Elevated serum calcium and low parathyroid hormone (PTH) Hint: This pattern suggests a non-PTH mediated cause of hypercalcemia, such as malignancy or vitamin D intoxication. | |
Low serum calcium and elevated parathyroid hormone (PTH) Hint: This is indicative of secondary hyperparathyroidism, often seen in chronic kidney disease. | |
Elevated serum calcium and elevated parathyroid hormone (PTH) | |
Low serum calcium and low parathyroid hormone (PTH) Hint: This suggests hypoparathyroidism or other causes of hypocalcemia unrelated to PTH. | |
Normal serum calcium and elevated parathyroid hormone (PTH) Hint: While PTH may be elevated, primary hyperparathyroidism typically presents with hypercalcemia. |
Question 2 |
Elevated serum calcium and low parathyroid hormone (PTH) Hint: This pattern is more indicative of primary hyperparathyroidism or conditions causing hypercalcemia independent of PTH. | |
Low serum calcium and elevated parathyroid hormone (PTH) | |
Elevated serum calcium and elevated parathyroid hormone (PTH) Hint: This combination suggests primary hyperparathyroidism, where the parathyroid glands produce excessive PTH, leading to hypercalcemia. | |
Low serum calcium and low parathyroid hormone (PTH) Hint: This pattern suggests hypoparathyroidism or other conditions causing hypocalcemia without appropriate PTH response. | |
Normal serum calcium and elevated parathyroid hormone (PTH) Hint: While PTH may be elevated, the hallmark of secondary hyperparathyroidism is the combination of low serum calcium with elevated PTH. |
Question 3 |
24-hour urine calcium excretion test Hint: Useful in the evaluation but does not localize the source of hyperparathyroidism. | |
Thyroid function tests Hint: Important in overall endocrine evaluation but not specific for parathyroid gland pathology. | |
Sestamibi scan of the parathyroid glands | |
Bone density scan Hint: Can assess for bone loss due to hyperparathyroidism but does not confirm the diagnosis. | |
Serum phosphate level Hint: Typically low in hyperparathyroidism but does not localize the parathyroid pathology. |
Question 4 |
Oral calcium supplements Hint: Not indicated in hypercalcemia due to hyperparathyroidism. | |
Parathyroidectomy | |
Thiazide diuretics Hint: Can increase serum calcium levels and are not recommended in hypercalcemia. | |
Calcitonin injections Hint: Used to lower calcium levels temporarily but not a definitive treatment for hyperparathyroidism. | |
Bisphosphonates Hint: Used in osteoporosis but do not treat the underlying hyperparathyroidism. |
|
List |
References: Merck Manual · UpToDate