85 y/o with back pain and constipation x 7 days
Patient will present as → a 68-year-old man presetns to the clinic for a regular check-up. His PSA levels have been gradually increasing over the last few years and are now 11 ng/mL. A digital rectal examination reveals an asymmetrically enlarged prostate with an irregular, nodular consistency on the left side. A transrectal ultrasound-guided biopsy is performed, which confirms the diagnosis of prostate adenocarcinoma with a Gleason score of 7. The patient has no symptoms of urinary obstruction or bone pain.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
May present with urinary retention, decrease in urine stream strength, or back pain (metastatic disease)
- Urinary retention is more likely a sign of BPH
- Digital rectal exam: hard, nodular, enlarged and asymmetrical prostate
- PSA > 4 warrants further workup
- PSA > 10 suggestive of cancer
Risk factor:
- Risk factors include old age (most men > 80 have a focus of prostate cancer) and family history
PSA > 4 get an ultrasound with needle biopsy
PSA > 10 get a bone scan to r/o METS
USPSTF recommendations for prostate cancer screening:
-
- All men aged 55 to 69 years – the decision to undergo periodic prostate-specific antigen (PSA)-based screening for prostate cancer should be an individual one.
- Men 70 years and older – The USPSTF recommends against PSA-based screening for prostate cancer in men 70 years and older.
The NCCN issued revised guidelines on prostate cancer screening:
-
- The NCCN recommends performing a baseline history (including family history, medications, and any history of prostate screening and disease) and physical examination
- The clinician should then discuss the risks and benefits of a baseline PSA test with the patient, and consider a baseline DRE to identify high-risk cancers associated with a seemingly normal PSA.
- In patients with a normal DRE result, the NCCN recommends baseline PSA testing at age 45-49 years, with retesting at age 50 years in patients with a level below 0.7 ng/mL and annual or biannual retesting in those with a level of 1.0 ng/mL or higher.
- For patients aged 50-70 years with a normal DRE and a PSA below 3 ng/mL, the NCCN recommends retesting every 1-2 years.
- NCCN panel members were divided on the question of PSA thresholds that would prompt prostate biopsy: 2.5 ng/mL has been used, whereas 3 ng/mL is evidence-based and reduces the risk for overdetection; however, some panel members recommended considering the PSA level in the context of other risk factors rather than using a specific PSA cutoff.
- In selected cases, risk calculators could be used to stratify risk.
Radical Prostatectomy - The complication is erectile dysfunction!
- Patients with metastases will need androgen deprivation therapy (leuprolide) if there are no meds, then castration
- Monitor PSA should be less < 0.1
 Osmosis Osmosis |
|
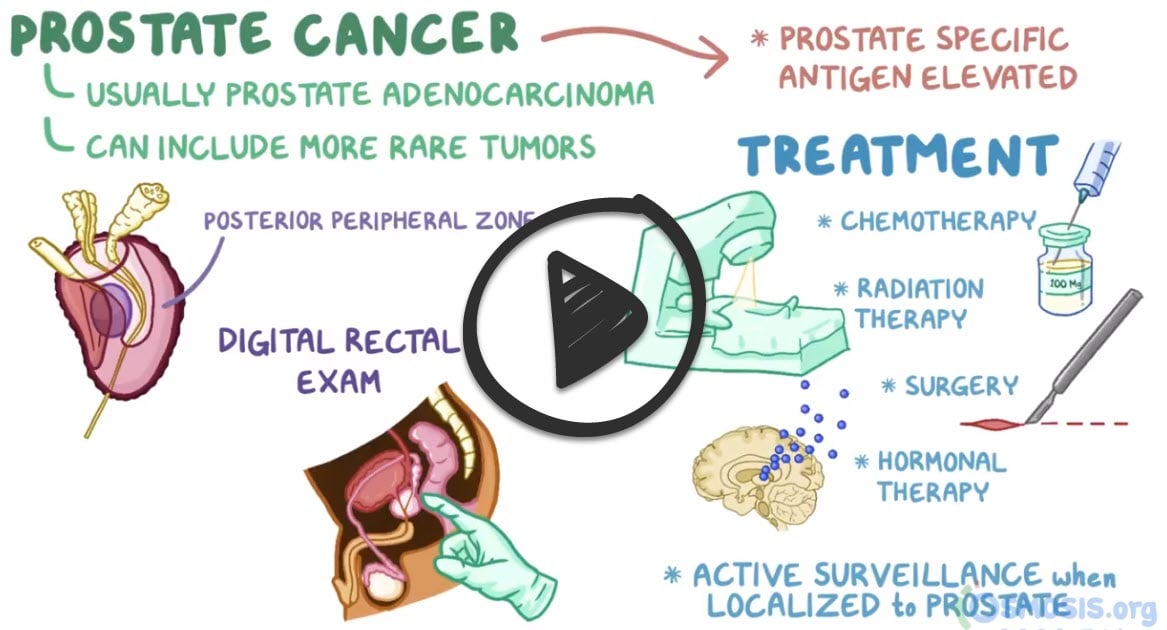 |

Prostate cancer is the most common cancer among men, and typically occurs in men over the age of 65. It can initially present with symptoms similar to those seen in BPH, like dysuria, dribbling, urgency, hesitancy, and hematuria. Prostate cancer can metastasize, and often does so to bone, and a common site is the lumbosacral vertebrae. Patients can display fatigue and lower back pain. There are diagnostic tests if there is a clinical suspicion of malignancy, such as PSA, PAP, and digital rectal exam. The only definitive diagnostic test is via ultrasound-guided needle biopsy.
| Prostate cancer assessment | Play Video + Quiz |
| Leuprolide | Play Video + Quiz |
Question 1 |
Periodic rectal exams Hint: Many prostate carcinomas are contained within the gland, making it difficult to assess progression with a digital examination alone. | |
Transrectal ultrasonography Hint: Ultrasonography is used largely for staging disease, not monitoring disease progression. | |
Measurements of serum acid phosphatase Hint: Serum acid phosphatase is more predictive of metastatic disease than PSA measurement, but its use has largely been replaced by PSA. | |
Measurements of prostate-specific antigen |
Question 2 |
Squamous cell carcinoma found in the peripheral zone Hint: Squamous cell carcinomas constitute less than 1% of all prostate carcinomas | |
Squamous cell carcinoma found in the central zone Hint: 15%-20% arise in the central zone | |
Acinar adenocarcinoma found in the peripheral zone | |
Sarcoma found in the transitional zone Hint: 10%-15% arise in the transitional zone | |
Adenocarcinoma located in the transitional zone Hint: While adenocarcinomas are the most common type of prostate cancer, they are most commonly found in the peripheral zone, not the transitional zone, making this option less accurate than option C. |
Question 3 |
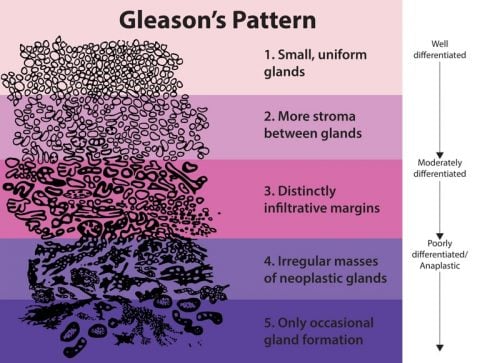
Grade 1 Hint: Small, uniform glands | |
Grade 2 Hint: More stroma between glands | |
Grade 3 | |
Grade 4 Hint: Irregular masses of neoplastic glands | |
Grade 5 Hint: Only occasional gland formation |
Question 4 |
Routine PSA screening for all men over age 50 Hint: This statement does not accurately reflect the USPSTF guidelines, which recommend against a one-size-fits-all approach and instead advocate for individualized decision-making for men aged 55 to 69 years. | |
PSA screening for men aged 55 to 69 years should be an individual decision | |
Annual PSA screening for men starting at age 40 Hint: The USPSTF does not recommend routine annual PSA screening starting at age 40 for all men. Screening decisions should be individualized, particularly for those in the 55 to 69-year age group. | |
PSA screening is not recommended at any age Hint: This statement is too broad and does not accurately represent the nuanced approach of the USPSTF, which suggests individualized decision-making for men aged 55 to 69 years and recommends against PSA-based screening for prostate cancer in men 70 years and older. | |
PSA screening for men aged 70 and older should be performed annually Hint: The USPSTF recommends against PSA-based screening for prostate cancer in men aged 70 years and older due to the potential harms outweighing the benefits in this age group. |
Question 5 |
MRI and CT Hint: While MRI is excellent for imaging the prostate and identifying suspicious areas, CT does not provide the same level of detail for prostate tissue and is generally not used for guiding prostate biopsies.
| |
Ultrasonography and CT Hint: Ultrasonography is commonly used in guiding needle biopsies of the prostate, but CT does not offer significant advantages in imaging the prostate or targeting biopsies and is not typically combined with ultrasonography for this purpose. | |
MRI and ultrasonography | |
PET and ultrasonography Hint: PET scans are used in certain contexts for imaging prostate cancer, particularly for detecting metastatic disease rather than for guiding biopsies of the prostate itself. Ultrasonography is used for biopsy guidance but does not benefit significantly from combination with PET for targeting biopsies in the prostate. | |
CT and PET Hint: Both CT and PET scans are more relevant for staging advanced prostate cancer and assessing for metastasis rather than for guiding initial biopsies of the prostate based on imaging of the gland itself. |
Question 6 |
External-beam radiation therapy Hint: This is a common treatment for localized prostate cancer, including medium-risk cases, and can be an effective option for controlling the disease. | |
Robotic prostatectomy Hint: Surgical removal of the prostate using robotic assistance is another viable treatment for localized prostate cancer, offering precise removal of cancerous tissue. | |
Total androgen deprivation | |
Watchful waiting Hint: For some men, especially those with medium-risk, localized prostate cancer, watchful waiting or active surveillance may be recommended to monitor the cancer closely without immediate treatment. | |
Cryotherapy Hint: While not as commonly recommended as radiation therapy or prostatectomy for medium-risk, localized prostate cancer, cryotherapy is a treatment option that involves freezing cancer cells. It's less commonly chosen but still considered a viable option for some patients. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture