Patient will present as → a 39-year-old woman after total thyroidectomy for papillary carcinoma of the thyroid is noted to have carpal spasms when her blood pressure is taken and facial muscle contractions with tapping over the facial nerve. You also note increased deep tendon reflexes along with perioral paresthesia. Lab work reveals decreased serum calcium, decreased parathyroid hormone, and elevated serum phosphate. On EKG, there is a prolongation of the QT interval.
Hypoparathyroidism will present with a decreased parathyroid hormone (↓ PTH). This causes calcium levels in the blood to decrease
- Hypoparathyroidism is rare, and you are much more likely to be tested on hyperparathyroidism
- The two most common etiologies are postsurgical (damage from neck or thyroid surgery) or autoimmune
- Accidental damage/removal of parathyroid during neck/thyroid surgery
- Autoimmune destruction of the thyroid gland
Patients will show signs of neuromuscular irritability with carpopedal spasm, laryngeal spasm, tingling, tetany, and facial grimacing.
- Muscular changes with hypoparathyroidism will be the opposite of those with hyperparathyroidism.
- Chvostek's sign (watch video): Tap of facial nerve elicits cheek twitch
- Trousseau's sign (watch video): BP cuff inflation elicits carpal spasm
Diagnosis is made by the triad: ↓ Ca+, ↓ PTH, and ↑ phosphate
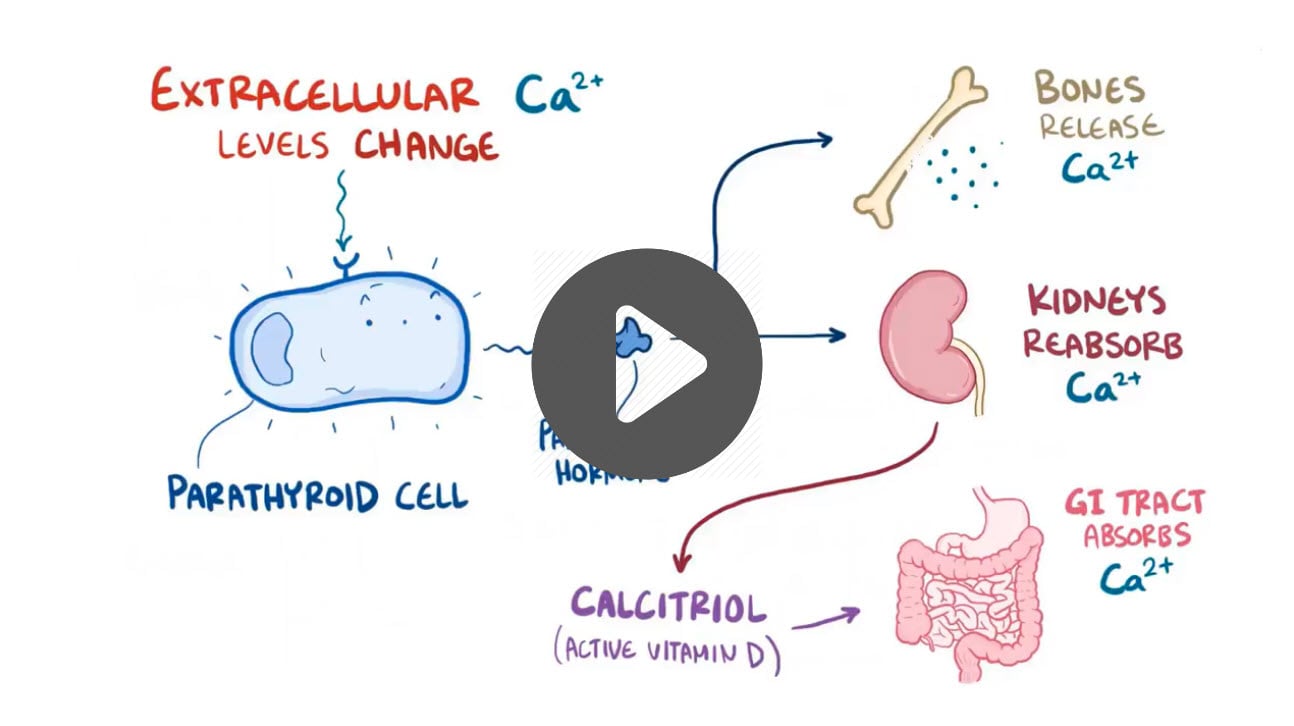
- Why the low serum calcium? Calcium is low because the gland cannot secrete PTH (hence a low PTH), and PTH is responsible for the reabsorption of calcium from the bones, kidneys, and GI tract. Because you can't reabsorb calcium, your calcium will be low.
- Why the elevated phosphate? PTH normally inhibits the reabsorption of phosphate by the kidney. Therefore, without enough PTH there is more reabsorption of the phosphate, leading to a high phosphate level in the blood.
- EKG = Prolonged QT
The following are signs of hypocalcemia:
- Chvostek's sign (watch video) is the twitching of the facial muscles in response to tapping over the area of the facial nerve
- Trousseau's sign (watch video) is carpopedal spasm caused by inflating the blood-pressure cuff to a level above systolic pressure for 3 minutes
- ↑ DTRs and carpopedal spasms
Immediate: vitamin D and calcium to bring calcium levels back to normal
- Tetany - secure airway, IV calcium gluconate
- Long-term: recombinant human parathyroid hormone to make up for the body's underproduction
 Osmosis Osmosis |
|
 |
Hypoparathyroidism is an uncommon condition characterized by a low level of parathyroid hormone (PTH). Often caused by “accidental” removal of the parathyroid glands during thyroid surgery. Other causes of parathyroid deficiency include tumors and heavy metal poisoning. Treatment consists of taking supplements to normalize calcium and phosphorus levels.
Play Video + QuizParathyroid Gland Overview
The parathyroid gland is a series of four small glands located in the neck on the rear surface of the thyroid gland. It serves primarily in calcium homeostasis and has a blood calcium sensor that detects when blood calcium levels are abnormally low. It responds by releasing parathyroid hormone (PTH) which stimulates osteoclasts into action. Osteoclasts resorb bone and release a large amount of calcium. This calcium enters the blood and results in increased blood calcium levels. PTH can also activate vitamin D by promoting the activity of an enzyme that converts inactive vitamin D to active vitamin D
Question 1 |
Hypothyroidism Hint: While hypothyroidism can present with muscle cramps and depression, it does not typically cause carpal-pedal spasms, which are more indicative of electrolyte imbalances like hypocalcemia. | |
Hyperventilation with panic attacks Hint: Hyperventilation syndrome can lead to transient decreases in ionized calcium, causing symptoms like carpal-pedal spasms. However, the patient's history of phenytoin use and the absence of reported hyperventilation or panic attacks make hypocalcemia a more likely diagnosis. | |
Hyperkalemia Hint: Hyperkalemia can cause muscle weakness and cardiac disturbances but does not cause carpal-pedal spasms, which are characteristic of hypocalcemia. | |
Hypocalcemia | |
Hyponatremia Hint: While hyponatremia can present with neuropsychiatric symptoms, it does not typically cause muscle cramps or carpal-pedal spasms, which are specific signs of calcium imbalance. |
Question 2 |
Autoimmune destruction of the parathyroid glands Hint: While it can cause hypoparathyroidism, it is less common than surgical causes. | |
Surgical removal of the parathyroid glands | |
Radiation therapy to the neck Hint: Can lead to hypoparathyroidism but is less common compared to surgical removal. | |
Magnesium deficiency Hint: Can affect PTH secretion but is not a primary cause of hypoparathyroidism. | |
Genetic disorders Hint: Certain genetic conditions can lead to hypoparathyroidism but are less common than surgical causes. |
Question 3 |
Elevated serum phosphate | |
Low serum magnesium Hint: While magnesium deficiency can affect PTH secretion, it is not a direct result of hypoparathyroidism. | |
Elevated serum potassium Hint: Not directly related to hypoparathyroidism. | |
Low serum glucose Hint: Not a typical finding associated with hypoparathyroidism. | |
Elevated serum sodium Hint: Changes in sodium levels are not characteristic of hypoparathyroidism.
|
Question 4 |
Oral calcium supplements Hint: Used for long-term management but not sufficient for acute symptomatic hypocalcemia. | |
Intravenous calcium gluconate | |
Vitamin D analogs Hint: Important for long-term management to enhance intestinal calcium absorption but not for immediate symptom relief. | |
Magnesium supplementation Hint: Indicated if hypomagnesemia is present but not as initial treatment for acute hypocalcemia. | |
Parathyroid hormone (PTH) therapy Hint: May be considered for chronic management but is not the first line for acute symptomatic hypocalcemia. |
Question 5 |
Oral calcium supplements Hint: Used for long-term management but not sufficient for acute symptomatic hypocalcemia. | |
Intravenous calcium gluconate | |
Vitamin D analogs Hint: Important for long-term management to enhance intestinal calcium absorption but not for immediate symptom relief. | |
Magnesium supplementation Hint: Indicated if hypomagnesemia is present but not as initial treatment for acute hypocalcemia. | |
Parathyroid hormone (PTH) therapy Hint: May be considered for chronic management but is not the first line for acute symptomatic hypocalcemia. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture