You have completed emergency medicine EOR topics: |
| Bullous pemphigoid |
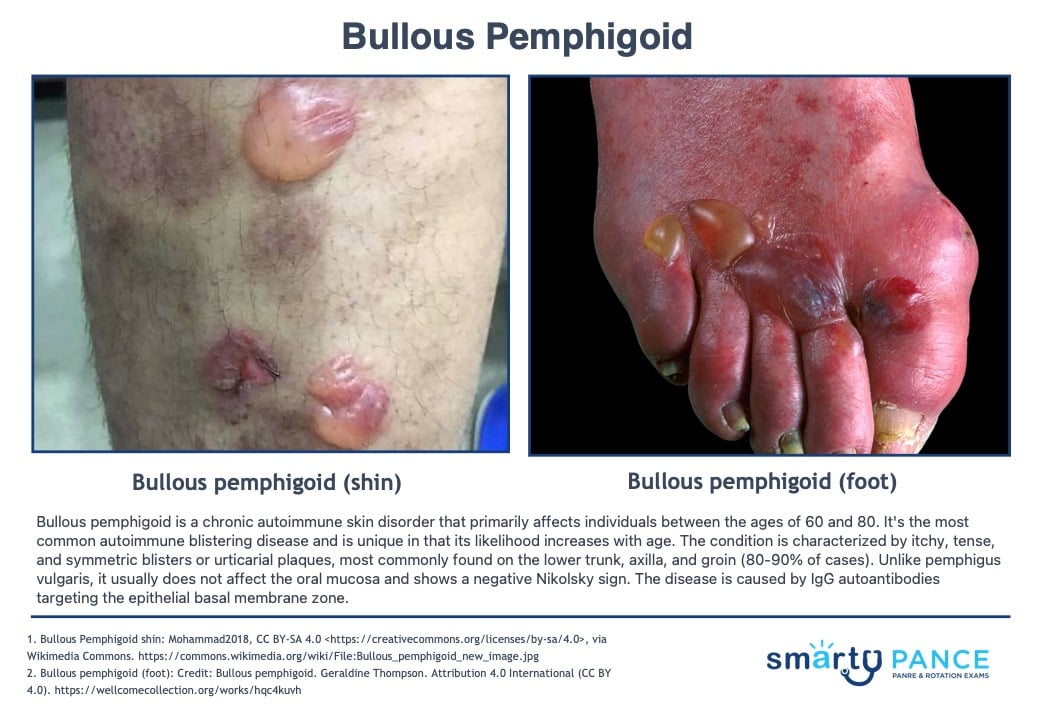
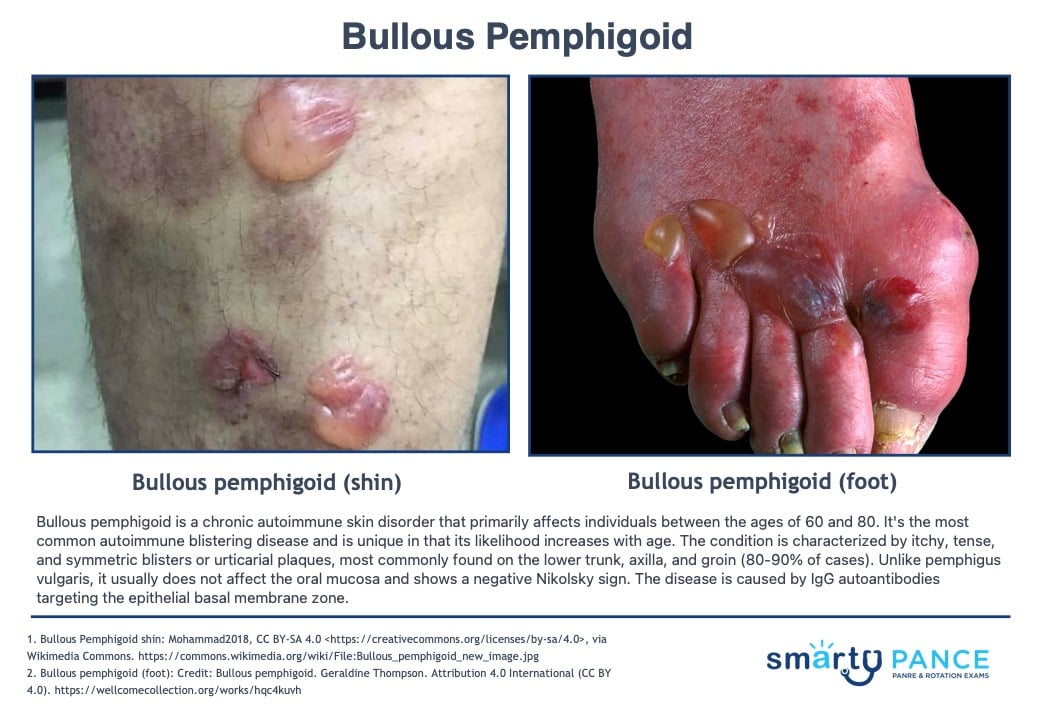
Patient will present as → a 75-year-old female who presents to the clinic with a large number of pruritic, tense, subepidermal bullae across her upper thighs. There was no mucosal involvement, a negative Nikolsky sign, and a skin biopsy showed subepidermal bullae filled with eosinophils and neutrophils. Bullous pemphigoid is a rare, chronic acquired autoimmune subepidermal blistering skin disorder caused by linear deposition of autoantibodies (IgG) against hemidesmosomes in the epidermal-dermal junction
- Bullous pemphigoid is less severe than pemphigus vulgaris, does not affect mucous membranes, and has a negative Nikolsky sign
- Large bullae and crusts located on axillae, thighs, groin, and abdomen. More tense, less fragile, and deeper than pemphigus vulgaris
- Diagnosis is made by skin biopsy with direct immunofluorescence exam shows deposition of IgG and C3 basement membrane
Treat with systemic corticosteroids
|
| Lice |
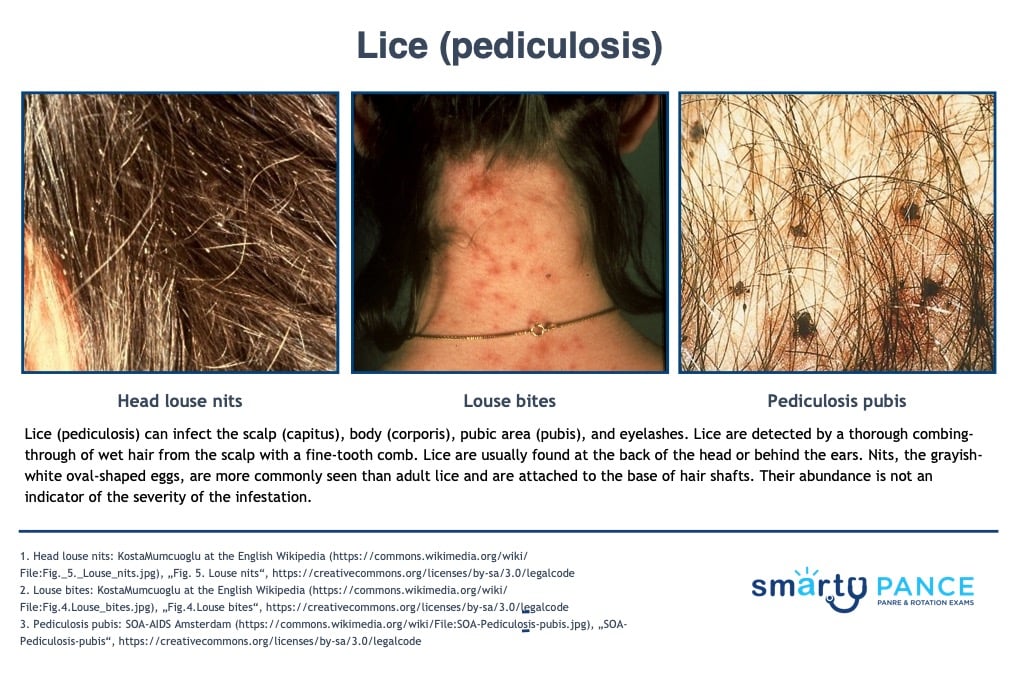
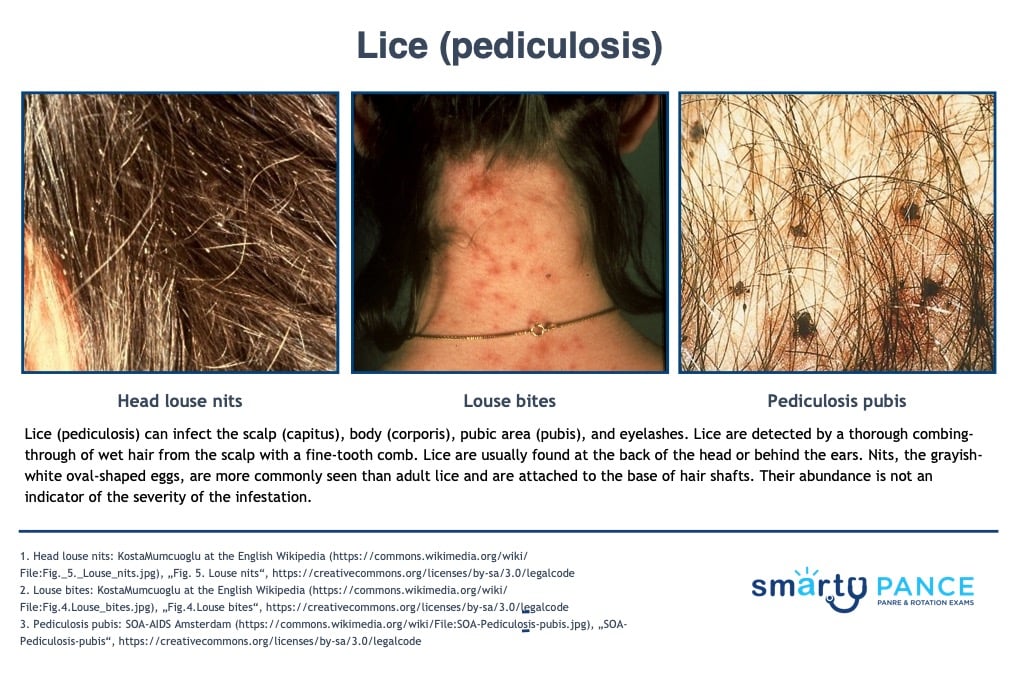
Patient will present as → a 9-year-old girl who is brought in by her mom, who noticed the child scratching her head at school pickup. She reports that this itchiness has gone on for around 1 week now. Her mom reports angrily that the school just notified them that several children had lice. Physical exam reveals several ovoid, grayish-white eggs < 1 cm away from the base of the hair shaft at the back of the head and behind the ears. She is given topical permethrin and counseled that she can still go to school. Pruritic scalp, body, or groin. Nits are observed as small white specs on the hair shaft
- Body (corporis); Pubic (pubis)
DX: Observation of lice and nits; nits = ovoid, grayish-white eggs
TX: launder potential fomites such as sheets in hot water (> 131 F or 55 C)
- Permethrin topical is the drug of choice used in combination with wet combing
- Capitis: shampoo to towel-dried hair and wash after 10 minutes, then repeat in 9 days
- Pubis/body lice: permethrin cream is applied to the entire clean body from the neck down, then washed off after 8-12 hours
- Screen for other STIs in patients with pubic lice - abstain from sexual contact until the infestation clears
- For eyelash infestation, apply ophthalmic-grade petroleum jelly BID x 10 days
- Lindane = older topical treatment that can’t be used on infants, children, and elderly due to neurotoxicity
- Children OK to return to school after the first application of treatment
- For resistant cases, consider oral ivermectin
- Treat all family members
View more images of pediculosis
|
| Burns |
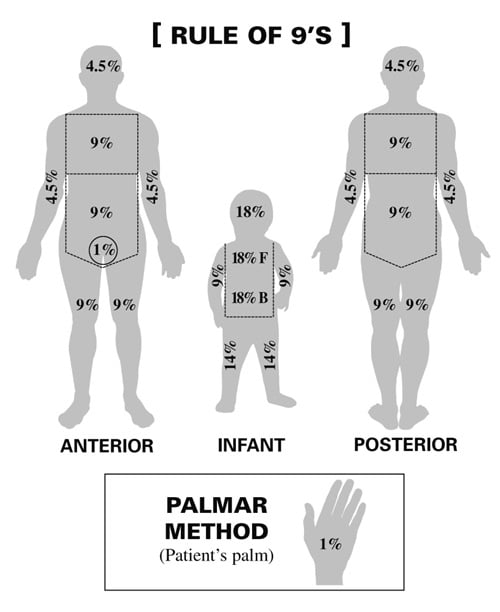
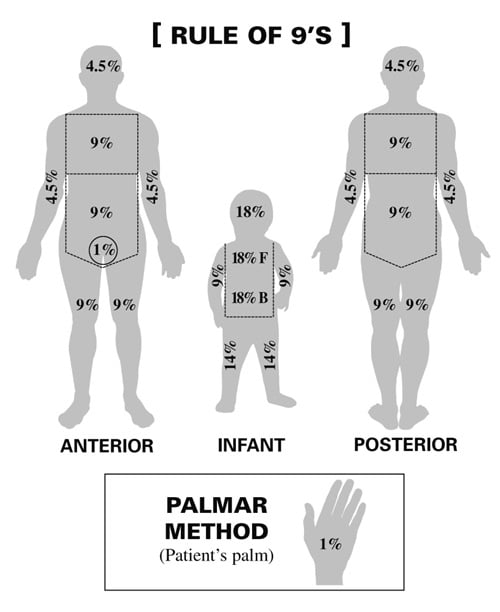
Patient will present as → a 35-year-old male who was throwing some paint thinner on fire to get it going a little better when it splashed on him and caught his R arm and his R hip area on fire. He did not have pain right away and was not going to go to the hospital. He washed off the burnt areas because he had grease and oil on his hands and lower arm. The pain then started to get bad enough for him to have his wife take him to the ER. Body percentage:
- Rule of 9’s: Head 9%, Each arm 9%, Chest 9%, Abdomen 9%, Each anterior leg 9%, Each posterior leg 9%, Upper back 9%, Lower back 9%, Genitals 1%
- Palmar method: Patient’s palm equates to 1%
Degree involvement:
Treatment: Monitor ABCs, fluid replacement, and sulfadiazine. Children with > 10% total body surface area and adults with > 15% total body surface area burns need formal fluid resuscitation
|
| Pilonidal disease |
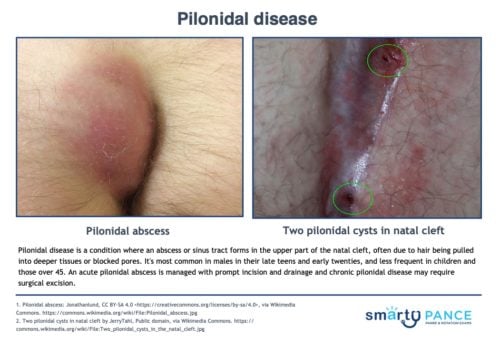
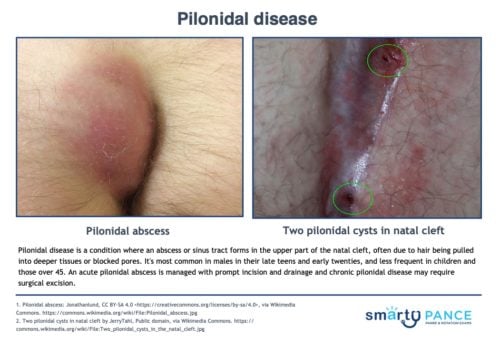
Patient will present as → a 15-year-old male with pain, discomfort, and swelling above the anus and near his tailbone that comes and goes. He reports that the pain worsens when he sits or bends forward. Medical history is significant for metabolic syndrome. He is a high school student who spends hours playing on his Xbox. On physical exam, there is a tender and fluctuant mass that is erythematous. There is also purulent discharge from a sinus tract. An abnormal skin growth located at the tailbone that contains hair and skin
- Results from an abscess, sinus tract, at the upper part of the natal (gluteal) cleft
- Will usually present as a teenager with pain, discomfort, and swelling above the anus or near the tailbone that comes and goes
- Often includes drainage of pus or blood
DX: The diagnosis is clinical
TX: drainage and surgical removal of the cyst - look for sinus tract – remove hair, curette granulation tissue
- Cefazolin + metronidazole or augmentin used empirically with cellulitis
View more images of pilonidal disease
|
| Cellulitis |
Cellulitis
 You are called to see a 20 y/o with wound ulceration and bleeding You are called to see a 20 y/o with wound ulceration and bleeding
Patient
- Gender: Male
- Age: 20 years
Signs and Symptoms
- 5 days splinter in leg; wound ulceration and bleeding
Click here to work through this patient case simulation.
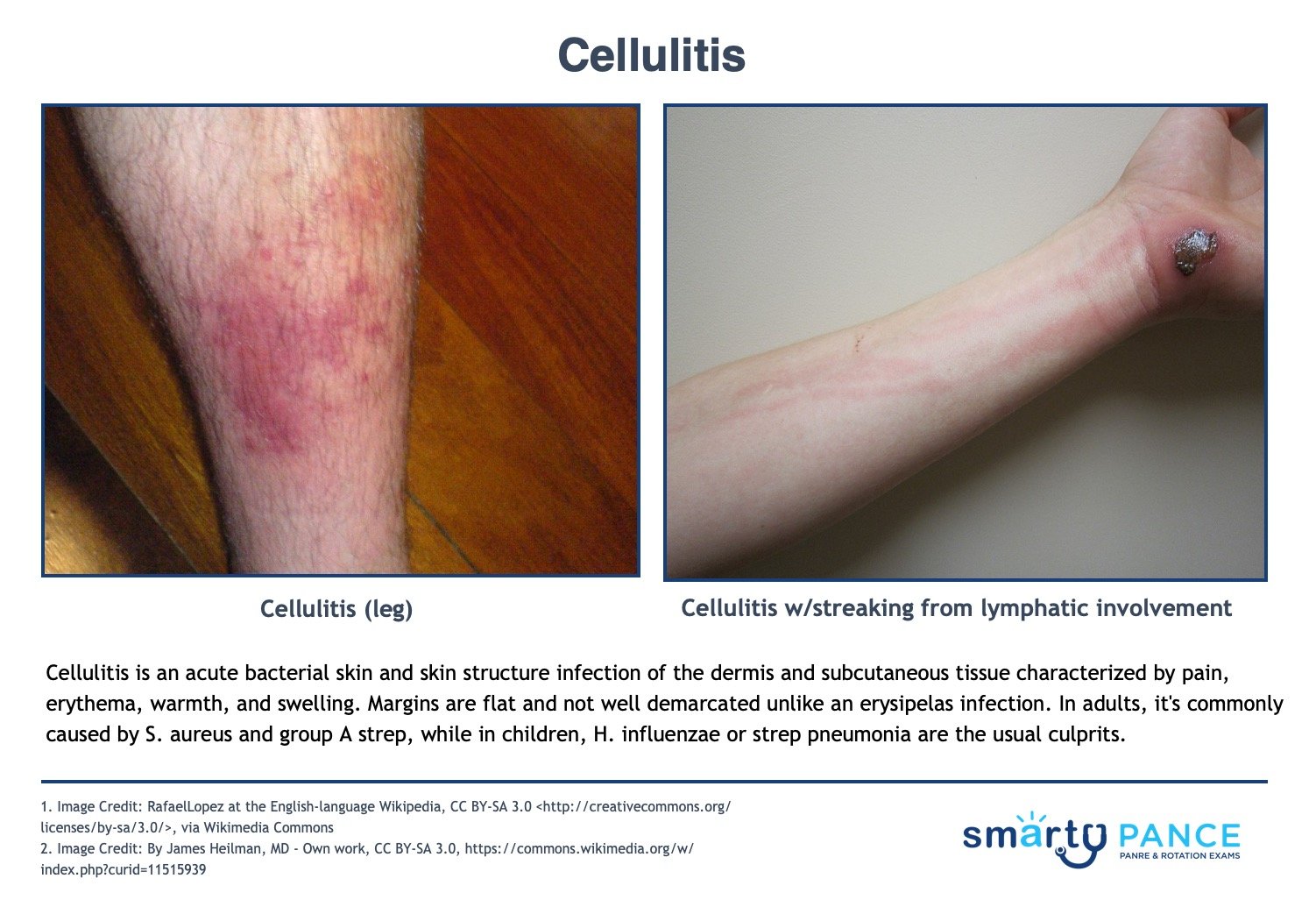
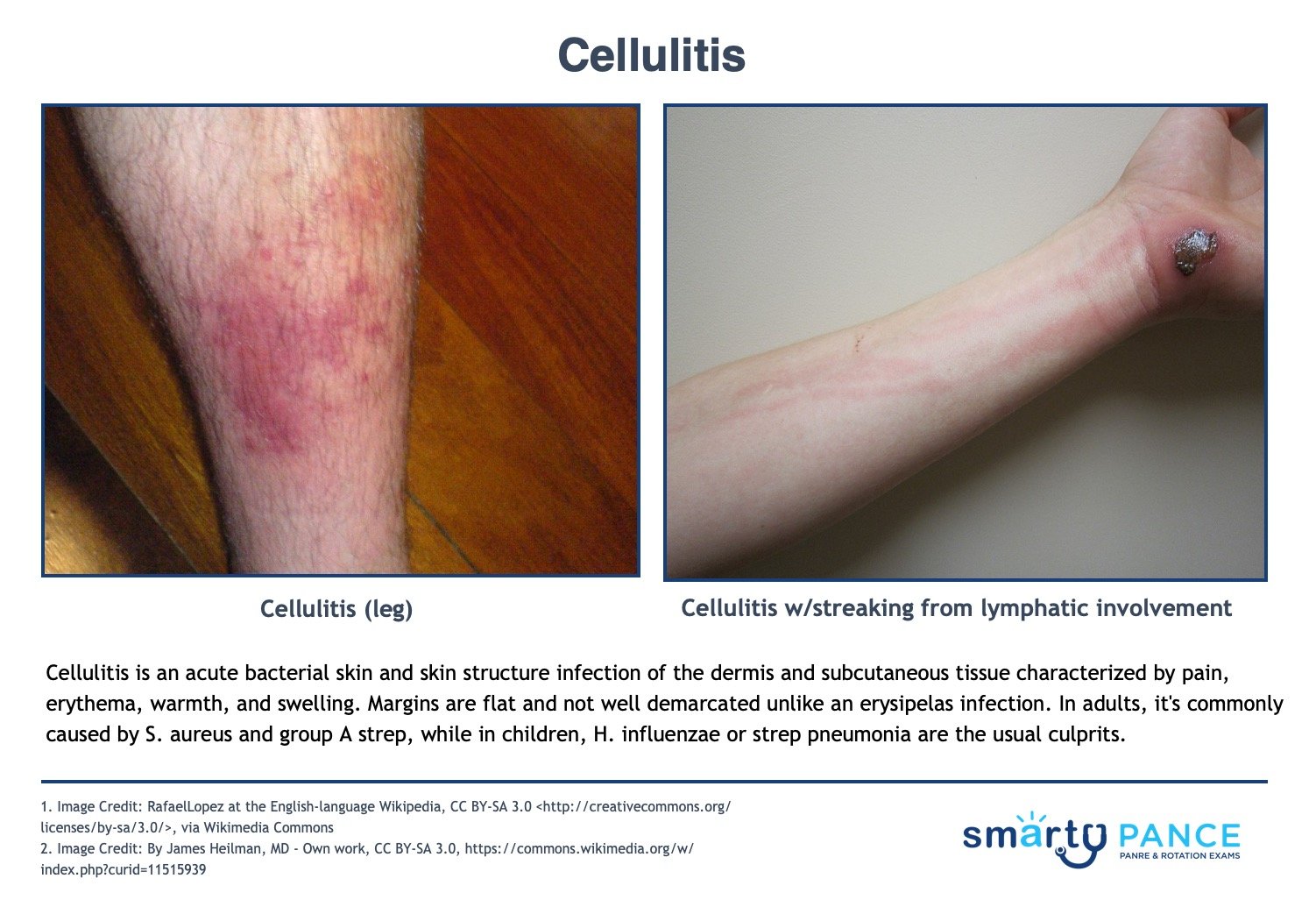
Patient will present as → a 64-year-old female with a 4 cm × 7 cm edematous, red, hot tender area on the left thigh. The lesion has gotten larger over the past 6 hours. She tells you she has also had a low-grade fever and some chills. On physical exam, there is a poorly demarcated 12cm red and tender plaque on her right calf. Some parts resemble an orange peel. There is a superficial cut in the middle of the plaque. An acute bacterial skin and skin structure infection of the dermis and subcutaneous tissue; characterized by pain, erythema, warmth, and swelling. Margins are flat and not well demarcated.
- Caused by Staphylococcus and Streptococcus in adults
- H. influenzae or strep pneumonia in children
- Cellulitis does not have sharp, well-defined borders, unlike an erysipelas infection
DX: Culture should be taken of all purulent wounds and followed up in 48 hours
Treat mild cellulitis (MSSA)
-
- Cephalexin 500 mg QID x 5-7 days
- Cefuroxime 500 mg BID x 5-7 days
- If PCN allergy - Clindamycin 450 mg TID x 5-7 days
Cat bites with augmentin or doxycycline if PCN allergic
-
- Puncture wound with Cipro (cover pseudomonas)
Treat purulent or methicillin-resistant Staphylococcus aureus infection (MRSA) with
- Trimethoprim-sulfamethoxazole (TMP-SMZ) 1 DS tab PO BID x 7 days
- Clindamycin 450 mg PO TID x 7 days
- Doxycycline 100 mg PO BID x 8 days
- Intravenous Vancomycin or Linezolid
View more images of cellulitis
|
| Pressure sores |
Patient will present as → an 80-year-old bed-bound woman with a temperature of 104°F who you are called to see in the nursing home. The patient is disoriented and confused. On physical examination, the patient’s blood pressure is 110/ 80 mm Hg, and her pulse is 72 beats/ minute and regular. There is an 8 × 5 cm pressure ulcer over her sacrum. Also, there is a purulent, foul-smelling discharge coming from the ulcer. The sacrum and hip are most often affected. Reposition every 2 hours
- Stage 1: erythema of localized area, usually non-blanching over the bony surface
- Stage 2: partial loss of dermal layer, resulting in pink ulceration
- Stage 3: full dermal loss, often exposing subcutaneous tissue and fat
- Stage 4: full-thickness ulceration exposing bone, tendon, or muscle. Osteomyelitis may be present
Wound management by stage of the ulcer
- Stage I: aggressive preventive measures, thin-film dressings for protection
- Stage II: occlusive dressing to maintain healing, transparent films, hydrocolloids
- Stages III-IV: Débridement of necrotic tissue. Exudative ulcers will benefit from absorptive dressings such as calcium alginates, foams, and hydrofibers. Dry ulcers require occlusive dressing to maintain moisture, including hydrocolloids, and hydrogels.
Risk factors: age >65, impaired circulation, immobilization, undernutrition, incontinence
DX: based on observation and staged according to classification
TX: debridement ⇒ depends on the extent of necrosis; surgical closure may be necessary; vacuum-assisted closure uses negative pressure to reduce wound edema and remove debris/reduce bacterial load
 Pressure ulcer staging. Stage I, erythema; Stage II, breakdown of the dermis; Stage III, full-thickness skin breakdown; Stage IV, bone, muscle, and supporting tissue involved. |
| Dermatitis (eczema, contact) |
Patient will present as → a 22-year-old female complaining of a rash around her mouth. She describes a feeling of mild burning or tension but denies pruritus. Examination reveals papulopustules on erythematous bases; the vermillion border is spared. A culture is negative 1. Contact dermatitis: well-demarcated erythema, erosions, vesicles
- Allergic: Nickel, poison ivy, etc. Type 4 hypersensitivity
- Irritant (diaper rash): Cleaners, solvents, detergents, urine, feces
- Treatment: Avoid the offending agent. Burow's solution (aluminum acetate), topical steroids, zinc oxide (diaper rash)

2. Atopic dermatitis: Pruritic, eczematous lesions, xerosis (dry skin), and lichenification (thickening of the skin and an increase in skin markings). Most common on flexor creases (e.g., antecubital and popliteal folds)
- IgE, type 1 hypersensitivity
- Infant- face and scalp
- Adolescent- flexural surfaces
- Treatment: Topical corticosteroids and emollients, topical calcineurin inhibitor (i.e., tacrolimus or pimecrolimus)

3. Nummular eczema: Coin-shaped/disc-shaped
- Treatment: High or ultra-high potency topical corticosteroids are first-line therapy for nummular eczema

4. Seborrheic dermatitis (cradle cap): Erythematous, yellowish greasy scales, crusted lesions.
- Infants - scalp (cradle cap)
- Adults/adolescents - face, chest, scalp
- Treatment: Ketoconazole shampoo


5. Perioral dermatitis: Young women. Papulopustular, plaques, and scales around the mouth.
- Treatment: Topical metronidazole, avoid steroids

View more images of dermatitis
|
| Rash |
Causes
- Skin rashes can be due to underlying disease
- Skin rashes can be due to the environment
- Examples include hot and humid weather, excess sun exposure
- Other causes include irritating substances and allergies
Presentation:
- Area of irritated or swollen skin
- Itchy, red, painful, and irritated
- It can also lead to blisters or patches of raw skin
- Rashes can be a symptom of many different medical problems
- Rashes may basically be divided into two types: infectious or noninfectious
Noninfectious rashes include eczema, contact dermatitis, psoriasis, seborrheic dermatitis, drug eruptions, rosacea, hives (urticaria), dry skin (xerosis), and allergic dermatitis.
Infectious rashes can present with fever
- For example, the rash in measles is an erythematous, morbilliform, maculopapular rash that begins a few days after the fever starts. It classically starts at the head and spreads downwards.
- Systemic disease rashes
- You see with jaundice, CRF, SLE, other autoimmune diseases
Treatment
- Differs according to which rash a patient’s diagnose
- Common rashes can be treated using steroid topical creams such as hydrocortisone or non-steroidal treatments
Pearls
Rashes are a clue as to what the patient may be exposed to or what infection or systemic disease they may have it is a piece of information that can help to the diagnosis of the patient
|
| Discharge |
Breast/nipple discharge
- Mastitis/Breast abscess: nipple discharge, redness, warm skin
- Breast Cancer: nipple discharge, breast discomfort, breast mass
- Gynecomastia: nipple discharge, breast enlargement, overweight
- Inflammatory breast cancer: nipple discharge, breast enlargement, redness
- Hypogonadism: nipple discharge, sexual dysfunction, reduced sex drive
GU
- Infections of the vagina, such as a yeast infection, bacterial vaginosis, trichomoniasis, human papillomavirus (HPV), or herpes
- Infection of the cervix (cervicitis)
- An object in the vagina, such as a forgotten tampon
- Sexually transmitted infections (STIs), such as chlamydia or gonorrhea
- Various sex practices, such as oral-to-vaginal and anal-to-vaginal contact
- Vaginal medicines or douching
- Menopause: vaginal discharge, an absence of menstruation, anxiety
Other skin conditions
- Abscess: pain, redness, with or without discharge
|
| Scabies |
Scabies  You are called to see a 4 y/o with itchy spots on arms, chest, and back
Patient
- Gender: Male
- Age: 4 years
- Weight: 29.3 lb/13.3 kg
- Height: 37.3 in/94.8 cm
Vitals
- Temperature: 96.9 F/36.1 C
- Blood Pressure: 98/46
- Heart Rate: 107
Signs and Symptoms
- Itchy spots on arms, chest, and back
Click here to work through this patient case simulation
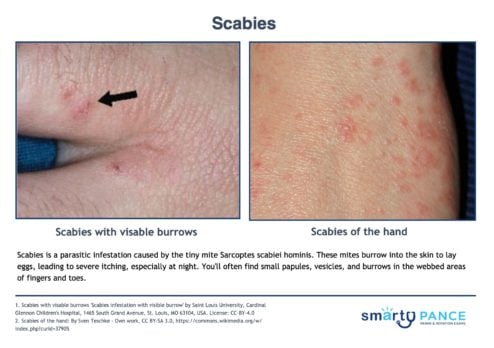
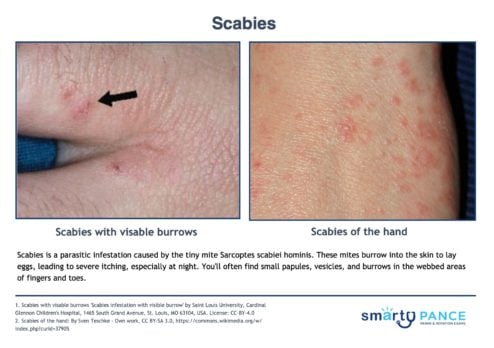
Patient will present as → an 11-year-old male complaining of intensely itchy, painful, red streaks between his fingers and in the groin area. The patient reports that the itchiness seems to be worse at night. His best friend whom he had a sleepover this past weekend, is also having similar symptoms. Pruritic papules - S-shaped or linear burrows on the skin. Often located in web spaces of hands, wrists, and waist with severe itching (worse at night)
DX: Microscopic observation of mites, eggs, or feces after a skin scrape
TX: Treat with topical permethrin 5% - apply to the entire body and wash after 8-14 hours ⇒ repeat in one week (> 2 months old)
- Sulfur 5%-10% ointment (< 2 months old)
- All clothing, bedding, and towels are washed and dried using heat and have no contact with body for at least 72 hours
- Oral ivermectin if extensive involvement or immunocompromised individual
- Approved for adults and children weighing at least 33 pounds who can swallow pills (OK for nursing women, but avoid in pregnancy)
- Prescribe two doses of about 200 mcg/kg, with the second dose given in 7-14 days. Most adults will need 4-6 tabs per dose
- The typical dose for an adult is 3 mg tabs. Take 4 tabs now and repeat again in 7-14 days
Pruritus may persist for 2-4 weeks after treatment
View more images of scabies
|
| Drug eruptions |
Patient will present as → a 17-year-old female with severe widespread red rash involving mainly the trunk and extremities one day after she took oral cephalexin suspension for a sore throat. An adverse cutaneous reaction in response to the administration of a drug, usually within the past 6 weeks
- Skin reactions are the most common adverse drug reactions
- Severity can range from mild eruptions that resolve after the removal of the inciting agent to severe skin damage with multiorgan involvement
DX: clinical – consider bacterial, viral, underlying skin disease like cutaneous lymphoma
TX: monitor for signs of impending cardiovascular collapse (anaphylaxis, DRESS (Drug Rash with Eosinophilia and Systemic Symptoms), SJS/TEN, extensive bullous reactions, generalized erythroderma)
- Withdraw offending agent
- Don’t rechallenge with drugs causing urticaria, bullae, angioedema, DRESS, or anaphylaxis
- Anaphylaxis or widespread urticaria ⇒ epinephrine 0.2-0.5mg – prednisone to prevent a recurrence
- Antihistamines

View more images of drug eruptions
|
| Spider bites |
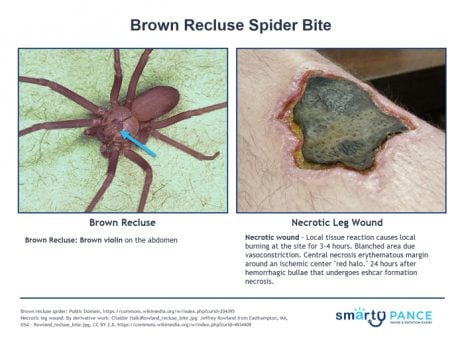
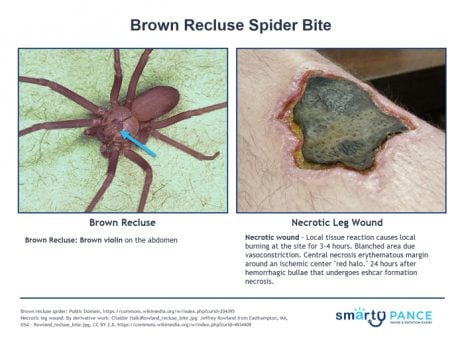
Brown Recluse:
- Brown violin on the abdomen
- Necrotic wound - local tissue reaction causes local burning at the site for 3-4 hours → blanched area (due to vasoconstriction) → central necrosis erythematous margin around an ischemic center “red halo” → 24-72 hours after hemorrhagic bullae that undergoes Eschar formation → necrosis
- TX: wound care, local symptomatic measures, delayed excision
Black Widow:
- Red hourglass on the abdomen
- Neurologic manifestations - may not see much at bite site: toxic reaction: nausea, vomiting, HA, fever, syncope, and convulsions
- TX: wound care, local symptomatic measures, sometimes opioids, benzos; treat with anti-venom in elderly and kids

|
| Erysipelas |
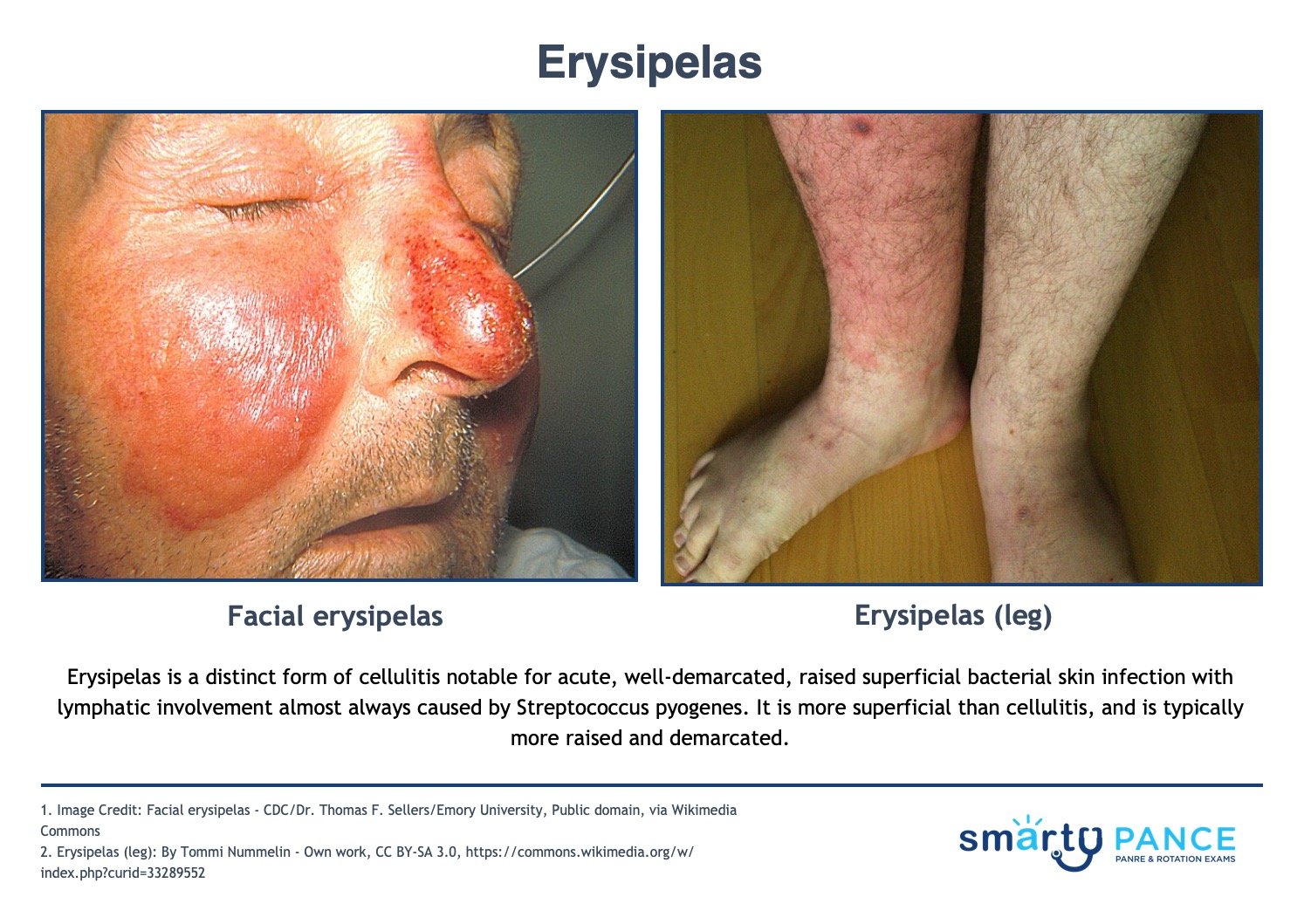
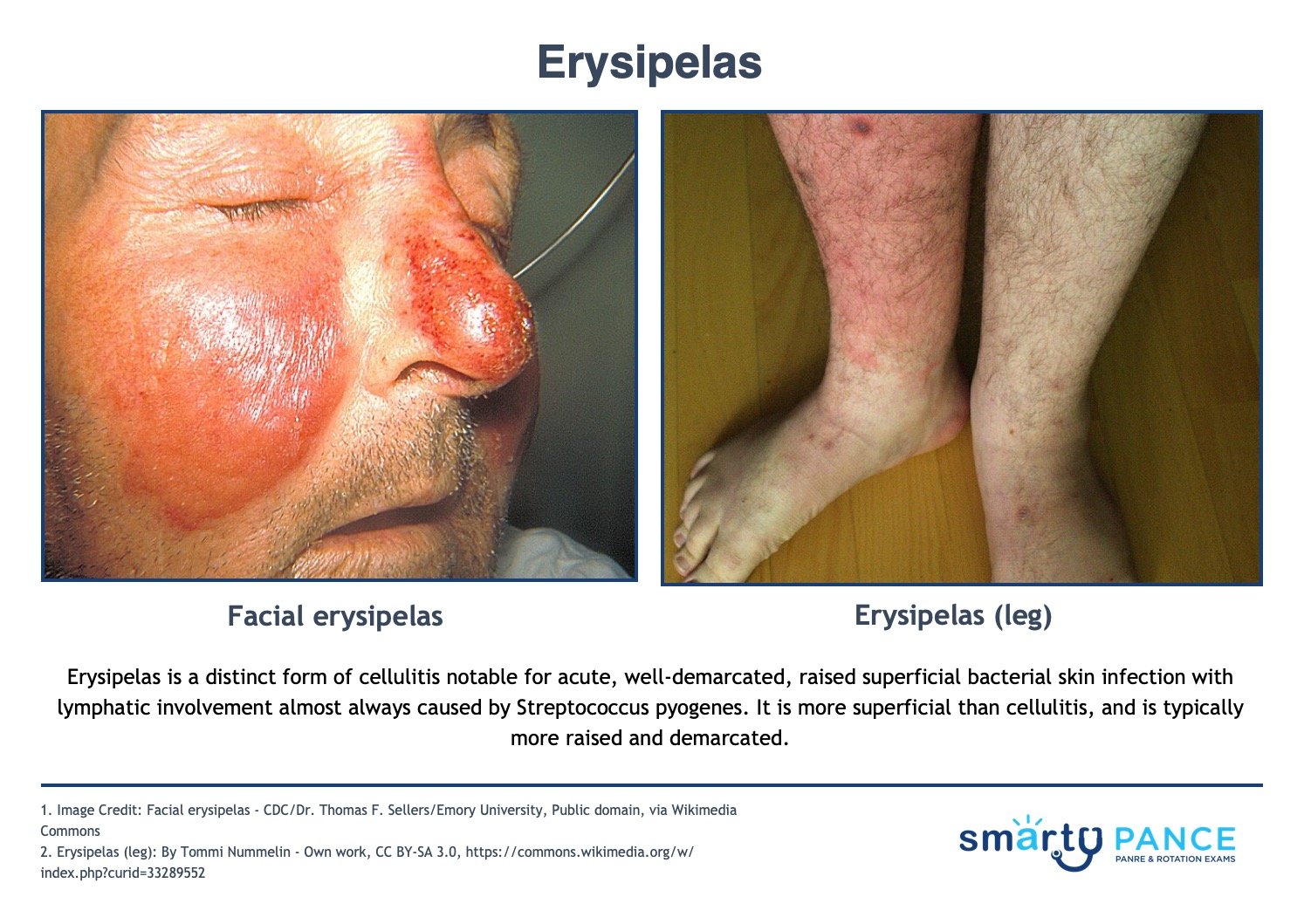
Patient will present as → a 19-year-old female with a painful rash on her left leg. She had a small bug bite in the same area about three weeks ago. Since then, the area has become red, painful, and hot. On physical exam, you note shiny, raised, indurated, and tender plaque-like lesions on the left leg. The redness is well-demarcated and hot to the touch. You send her home on penicillin. A distinct form of cellulitis notable for acute, well-demarcated, raised superficial bacterial skin infection with lymphatic involvement almost always caused by Streptococcus pyogenes
- Symptoms may include redness and pain at the affected site, fevers, and chills
- It looks like cellulitis, but it is well-demarcated and caused by group A strep (strep pyogenes)
DX: Wound culture and sensitivity
- CBC, ↑ CRP, ↑ ESR, ↑ WBCs; antistreptolysin titer O shows streptococcal involvement
- Blood cultures
TX: Treat with antibiotics: regimen depends on location and severity
- Mild can be treated with Penicillin G
- Patients with an allergy to penicillin can be treated with erythromycin or clindamycin
- Moderate: Trimethoprim-sulfamethoxazole (TMP-SMX)-DS: 1–2 tablets PO BID and penicillin VK 500 mg PO QID or cephalexin 500 mg PO QID
- Severe: IMP or MER or ERTA IV and linezolid 600 mg IV/PO BID or vancomycin IV or daptomycin 4 mg/kg IV q24h
View more images of erysipelas
|
| Stevens-Johnson syndrome |
Patient will present as → a 60-year-old woman with a severe drug-induced reaction on both lower limbs with few lesions elsewhere in addition to mucosal involvement of the mouth of two days duration. The insulting drug was sulfonamide, and the onset of the rash was within 48 hours of taking the drug. The rash comprised bilateral symmetrical bullae on a background of erythematous macules and patches in addition to erosions and peeling. Stevens-Johnson syndrome is a rare, serious hypersensitivity complex that affects the skin and the mucous membranes. It's usually a reaction to a medication or an infection commonly caused by anticonvulsants and sulfa drugs!
- SJS is 3-10% of the body
- It begins with a prodrome of flu-like symptoms, followed by a painful red or purplish rash that spreads and blisters. Layers of skin peel away in sheets (+) Nikolsky's sign (pushing blister causes further separation from the dermis)
- Stevens-Johnson syndrome (SJS) is a milder form of toxic epidermal necrolysis (TEN) with LESS THAN 10% of body surface area detachment
DX: Skin biopsy shows necrotic epithelium
DDX: erythema multiforme, viral exanthems, drug rash
TX: Stop all offending medications, early admission to burn unit, manage fluid/electrolytes/nutrition, airway stability, eye care
- Intravenous immunoglobulin (IVIG)
- Steroids, which used to be the treatment of choice, are now thought to be an increased risk for sepsis
 Image by Balasundaram S, Ranganathan K, Umadevi K, Gunaseelan R, Kumaraswamy N, Solomon S, Devaleenol B, Ambrose P – Journal of oral and maxillofacial pathology. CC BY 2.0
 Image: by lasundaram S, Ranganathan K, Umadevi K, Gunaseelan R, Kumaraswamy N, Solomon S, Devaleenol B, Ambrose P – Journal of oral and maxillofacial pathology: JOMFP (2011). CC BY 2.0 View more images of SJS-TEN
|
| Herpes zoster |
Shingles
 You are called to see a 5 y/o with leg pain and rash You are called to see a 5 y/o with leg pain and rash
Patient
- Gender: Male
- Age: 5 years
Signs and Symptoms
Click here to work through this patient case simulation.
Herpes zoster (shingles): varicella reactivation causing a maculopapular rash along one dermatome
Patient with herpes zoster (shingles) will present as → a 67-year-old male who presents to your clinic with a two-day history of a painful rash on his left flank radiating to his back. This was preceded by burning pain in the same region several days prior. The patient does not recall any history of childhood exanthems and is not up to date on his immunizations. Vital signs are stable. Physical exam reveals a maculopapular rash in a dermatomal distribution on the left flank and extending into the back.
- If testing is deemed necessary - PCR or direct immunofluorescence (DFA) are the tests of choice
-
- Hutchinson’s sign - lesion on the nose -> is an early indicator of ophthalmic (eye) shingles
- Zoster ophthalmicus: shingles involving CCN V, dendritic lesions on slit lamp exam if keratoconjunctivitis is present
- Zoster Oticus (Ramsay-Hunt Syndrome): facial nerve (CN VII) otalgia, lesions on the ear, auditory canal, and TM, facial palsy, auditory symptoms
- Treat shingles with acyclovir, valacyclovir, and famciclovir - given within 72 hours to prevent post-herpetic neuralgia
- Postherpetic Neuralgia: pain > 3 months, paresthesias, or decreased sensation. Treat with gabapentin or TCA, topical lidocaine gel, and capsaicin
Recombinant zoster vaccine (RZV, Shingrix) is recommended to prevent shingles in adults 50 years and older
-
- Two dose series 2-6 months apart
- Should be given to patients who previously received Zostavax (ZVL) ⇒ administered at least two months after ZVL
|
| Toxic epidermal necrolysis |
Patient will present as → a 60-year-old woman with a severe drug-induced reaction with extensive skin involvement covering > 30% of her body surface area. The insulting drug was anticonvulsant medication, and the onset of the rash was within 10 days of taking the drug. The rash comprised bilateral symmetrical bullae on a background of erythematous macules and patches in addition to erosion and peeling. On examination, her skin peels away in sheets when pressure is applied and rubbed. A rare, life-threatening skin condition that is usually caused by a reaction to drugs
- TEN is > 30% of the body
- Very similar to Steven-Johnson syndrome – The difference is the age of the individuals (in toxic epidermal necrolysis older patients vs. SJS younger patients) and percentage of the body affected (in TEN > 30% of body surface area affected vs. SJS < 10% of body surface area affected)
DX: Confirm the diagnosis by biopsy (showing necrotic epithelium)
TX: Early treatment decreases the often high mortality rate
- Except for mild cases, treat SJS/TEN in a burn unit and with intensive supportive care
- Consult ophthalmology if the eyes are affected
- Cyclosporine and possibly plasma exchange for severe cases
|
| Impetigo |
Impetigo
 You are called to see a 2 y/o with rhinorrhea and facial rash You are called to see a 2 y/o with rhinorrhea and facial rash
Patient
- Gender: Female
- Age: 2 years
- Weight: 32 lb/14.5 kg
Vitals
- Temperature: 98.1 F/36.7 C
- Heart Rate: 90
- Respiratory Rate: 16
Signs and Symptoms
- Nasal congestion; rhinorrhea; pruritic facial rash
Click here to work through this patient case simulation.
Patient will present as → a 5-year-old girl with crusting facial lesions present for 3 days. The mother reports that prior to the development of the facial lesions, her daughter was scratching at insect bites. Examination reveals a red facial rash with a golden “honey-colored crust” and pruritus. Child < 6 y/o complaining of non-painful, pruritic lesions on the face
- The main symptom is red sores that form around the nose and mouth. The sores rupture, ooze for a few days, then form a yellow-brown crust
- “honey-colored” and weeping
- Most commonly caused by S. aureus
Nonbullous impetigo: the most common form of impetigo caused by staphylococcus aureus or streptococcus pyogenes characterized by honey-colored crusts on the face and extremities
Bullous impetigo: staphylococcus aureus impetigo that progresses rapidly from small to large flaccid bullae (newborns/young children) caused by epidermolytic toxin release. There is less lymphadenopathy and the trunk is more often affected; < 30% of patients
- When the bullae rupture, yellow crusts with oozing result
DX: The diagnosis is usually made clinically, but rarely a culture may be useful
TX: topical mupirocin, dicloxacillin, cephalexin for more severe illness
- Complications: poststreptococcal glomerulonephritis
 View more images of impetigo View more images of impetigo
|
| Urticaria |
Patient will present as → a well-appearing 9-month-old male with a rash that comes and goes. According to the mother, citrus was recently added to the patient’s diet. On physical exam, you observe a widespread rash composed of blanchable, edematous, pink, papules, and wheels on the face, trunk, and lower extremities. The patient is started on PRN oral antihistamines for pruritis and the mother is encouraged to eliminate citrus from his diet. The rash resolves within 72 hours. Urticaria (hives) is a skin rash triggered by a reaction to certain foods, medications, stress, or other irritants
- Symptoms include blanchable, pruritic, raised, red, or skin-colored papules, wheels or plaques on the skin's surface; usually, disappear within 24 hours
- (+) Darier's sign: localized urticaria appearing where the skin is rubbed (histamine release)
- Angioedema: a painless, deeper form of urticaria affecting the lips, tongue, eyelids hand, and genitals
DX: extensive lab testing not indicated; skin or IgE testing limited to the specific history of provoking allergen
TX: Hives usually go away without treatment, but antihistamine medications are often helpful in improving symptoms
- Second-generation antihistamine blockers (H1) are first-line treatment (Allegra, Claritin, Clarinex, Zyrtec)
- First-generation antihistamine for sleep disturbances: hydroxyzine/diphenhydramine
- H2 antihistamines as adjuvants: cimetidine, ranitidine
- Steroids for exacerbations, avoid chronic use
If anaphylaxis, give epinephrine: 0.3–0.5 mg. Use 1:1,000 dilution for IM route and 1:10,000 for IV route
- Peds: epinephrine 0.01 mg/kg SC/IV
 View more images of urticaria View more images of urticaria
|
| Itching |
Presentation:
An uncomfortable, irritating sensation that creates an urge to scratch that can involve any part of the body.
Common causes of this symptom:
- Itching can have causes that aren't due to underlying disease. Examples include hair regrowth, sunburns, insect bites, dry skin, or healing wounds
- Itching can result from
- Skin disorders (most common cause)
- Disorders of other organs (systemic disorders)
- Drugs and chemicals
Skin disorders
- Dry skin ( xeroderma and ichthyosis)
- Atopic dermatitis (eczema)
- Contact dermatitis
- Hives
- Insect bites scabies
Systemic disorders
- Allergic reaction ( food, drugs, bites, or stings)
- Disorders of the liver, such as jaundice
- Chronic kidney disease
- psychogenic itching
Treatment
- Skincare measures ( moisturizing the skin, and humidifying the air)
- Itching can usually be relieved by topical creams and steroids or systemic treatments such as Benadryl, steroids, Pepcid, etc.
Pearls:
- Itching usually results from dry skin, a skin disorder, or an allergic reaction
- Other causes may be a drug or a systemic disorder
|
| Viral exanthems |
Erythema infectiosum (fifth disease): Parvovirus B19 - "slapped cheek" rash on face - lacy reticular rash on extremities, spares palms and soles; resolves 2-3 weeks; supportive care/anti-inflammatories
Hand-foot-mouth disease: children < 10 years old caused by coxsackievirus type A virus-producing sores in the mouth and a rash on the hands, feet, mouth, and buttocks (watch video); usually clears 10 days; tx = supportive / anti-inflammatories
Measles (rubeola): The 4 C's - cough, coryza, conjunctivitis and cephalocaudal spread
- Morbilliform - maculopapular, brick red rash on face beginning at hairline then progressing to palms and soles last - rash lasts 7 days
- Koplik spots (small red spots in buccal mucosa with the blue-white pale center) precede the rash by 24-48 hours
- TX = supportive: anti-inflammatories, isolate 1 week after onset of rash
Rubella: 3-day rash; first appears on face, spreads caudally to trunk and extremities, and becomes generalized in 24 hours; cephalocaudal spread; teratogenic in 1st trimester (deafness, cataracts, TTP, mental retardation)
Roseola (sixth disease): Herpesvirus 6 or 7, only childhood exanthem that starts on the trunk and spreads to the face
- High fever for 3-5 days, then rose pink maculopapular blanchable rash on trunk/back and face
|