Patient will present as → a 25-year-old male who is being seen for an immigration physical. On physical examination, you note delayed secondary sexual characteristics - childlike voice, bilateral gynecomastia, minimal axillary hair, small testes 3 MLS, and a small penis ( < 1 cm). The patient is normotensive (BP 110/70), weight 74.8kg, height 160.7 cm, BMI 29. When questioned, he reports a lack of early morning erection. No history of tiredness or blurred vision. Laboratory investigation reveals a 9 am testosterone 2.8 nmol/L (8-30), LH 37 U/l, FSH 30.1 U/l, Prolactin - 96 mIU/L, 9 am cortisol - 374 nmol/L, T4 13.19 pmol/L, and TSH 1.3 mU/L. A chromosomal analysis reveals a 47 XXY, compatible with Klinefelter’s syndrome. MRI of the pituitary demonstrates a small pituitary, but no mass or lesion is seen.
A failure of the gonads (testes in men and ovaries in women) to function properly. Production of a man's testosterone and a woman's estrogen are inhibited
- If the onset is before puberty, growth, and sexual development may be affected
- After puberty, there may be sexual difficulties, reduced fertility, and absence of menstruation
Male hypogonadism
Decrease in effective testosterone levels as a result of
- Decreased free concentration - often a result of decreased production (Leydig and pituitary dysfunction), also result of increased synthesis of SHBG
- Decreased activity at receptor - often a result of androgen receptor deficiency
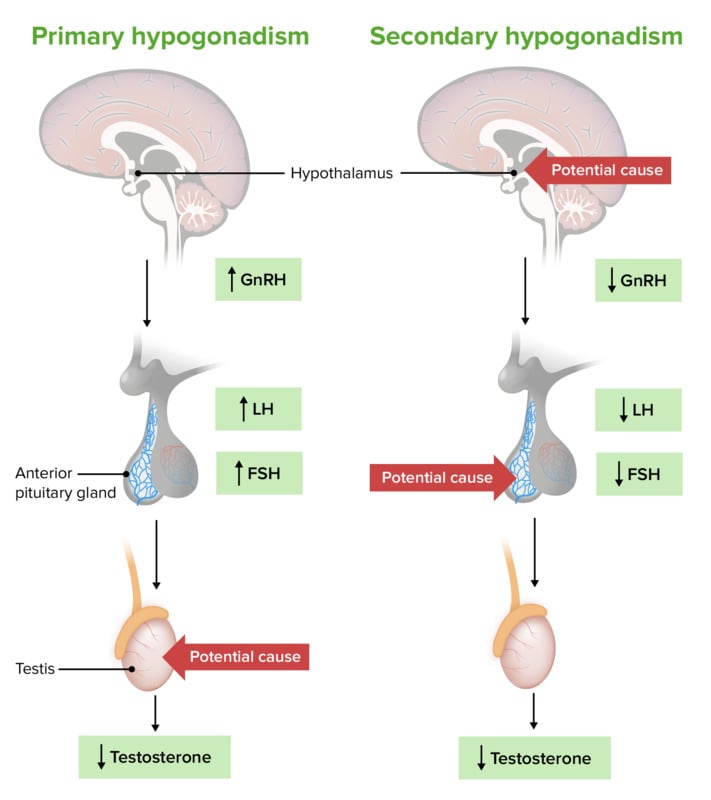
It may be primary, secondary, or age-related
Primary hypogonadism/hypergonadotropic hypogonadism - ↓ function of Leydig cells - results in ↓ testosterone synthesis
- Etiologies include alcoholic liver disease and damage to Leydig cells as a result of trauma, toxins, inflammation, and irradiation
- Klinefelter syndrome, orchitis, congenital or acquired anorchia, testicular maldescent, testicular tumors
Secondary hypogonadism/hypogonadotropic hypogonadism: ↓ function of hypothalamus/pituitary - results in ↓ LH and FSH synthesis and consequent ↓ testosterone synthesis
- Craniopharyngioma
- Pituitary adenoma
Hypothalamus pituitary testicular axis
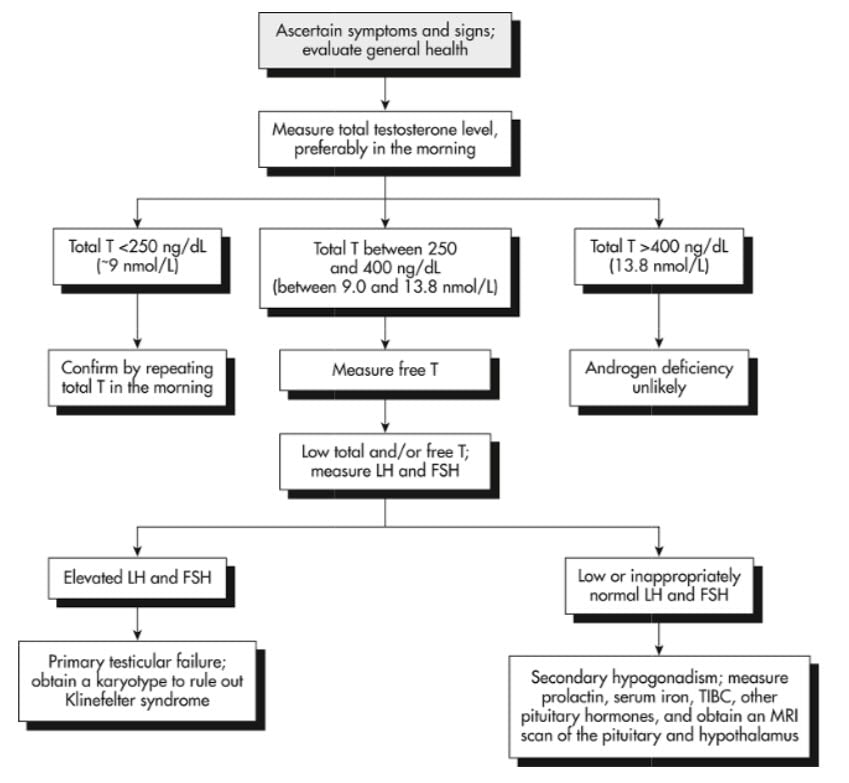
Testosterone replacement therapy is indicated when patients have symptoms and signs of hypogonadism and serum testosterone levels that are consistently subnormal with levels of <250 ng/dl.
- In patients with hypogonadotropic or secondary hypogonadism, chorionic gonadotropin and/or GnRH therapy can optimize spermatogenesis, whereas, generally in patients with primary hypogonadism, subnormal spermatogenesis and infertility are irreversible.
Nonpharmacologic therapy
- Weight reduction, especially when it appears to be a major factor underlying male hypogonadism
- Discontinuation of anabolic steroids, CNS-active medications, and narcotic abuse
- Surgery or radiation therapy for patients with a pituitary functioning or non-functioning tumor with visual field abnormality and headaches who are not candidates for further medical therapy or have been unsuccessfully treated with medication
- Surgery indicated for chronic gynecomastia and, occasionally, in cases with recent-onset gynecomastia that has not responded to testosterone replacement therapy
Chronic therapy testosterone formulations may include:
- Depo-testosterone 150 to 200 mg is injected intramuscularly every 2 weeks
- Testosterone adhesive patch (Androderm) delivers 2.5 or 5 mg of testosterone when applied nightly to the back, abdomen, upper arms, or thighs. Serum testosterone levels rise to within normal range in a few hours after application and, thereafter, are relatively stable. Daily doses of up to 10 mg may be necessary
- Testosterone gel - The gel is applied daily in the morning by hand over the shoulder, upper arms, or abdomen
- Testosterone pellets: 3 to 6 pellets of testosterone, each containing 75 mg of testosterone, are surgically inserted subcutaneously every 3 to 6 months and provide relatively stable serum testosterone levels
Monitoring should be done two to three months after the initiation of treatment and after changing a dose. When the dose appears to be stable, monitoring every 6 to 12 months should suffice
- Depo-testosterone: Serum testosterone should be measured midway between injections in men who are receiving testosterone enanthate or cypionate, and the value should be mid-normal, e.g., 500 to 600 ng/dL. The dose should be reduced if higher values are obtained
- Transdermal: The serum testosterone can be measured at any time in men who are using any of the transdermal preparations, with the recognition that the peak values occur six to eight hours after application of the patch
- Gel: two serum testosterone measurements before making dose adjustments. The therapeutic goal should be a testosterone value well within the normal range (400 to 700 ng/dL [13.9 to 24.3 nmol/L])
Question 1 |
Normal gonadotropins (LH/FSH) and normal testosterone Hint: This finding would be more indicative of a normal hypothalamic-pituitary-gonadal axis and does not align with the patient's clinical presentation. | |
Elevated gonadotropins and low testosterone Hint: This pattern is suggestive of primary hypogonadism, where the problem lies in the testes, leading to decreased testosterone production and a compensatory increase in gonadotropins. | |
Elevated gonadotropins and high testosterone Hint: This finding is not typical of either primary or secondary hypogonadism and would prompt evaluation for other conditions. | |
Reduced gonadotropins and low testosterone | |
Reduced gonadotropins and high testosterone Hint: This is an unusual pattern and does not fit with secondary hypogonadism. High testosterone levels would not typically be seen in the setting of reduced gonadotropin levels unless there is an exogenous source of testosterone. |
Question 2 |
Primary testicular failure Hint: Typically presents with high gonadotropin levels, which is not indicated in the scenario. | |
Hyperprolactinemia Hint: Can cause hypogonadism, but there's no indication of prolactin elevation or related symptoms. | |
Secondary hypogonadism due to obesity and diabetes | |
Exogenous testosterone use Hint: Leads to suppressed gonadotropin levels, but there's no history of testosterone use. | |
Klinefelter syndrome Hint: A genetic cause of primary hypogonadism, usually diagnosed earlier in life. |
Question 3 |
Kallmann syndrome Hint: A form of secondary hypogonadism with low gonadotropin levels. | |
Primary hypogonadism | |
Secondary hypogonadism Hint: Characterized by low gonadotropin levels. | |
Androgen insensitivity syndrome Hint: Presents with female or ambiguous genitalia despite a male karyotype. | |
Prolactinoma Hint: Would typically present with hyperprolactinemia and possibly low gonadotropin levels. |
Question 4 |
Testosterone gel | |
Oral testosterone undecanoate Hint: While this is a form of testosterone replacement, it is not typically the first choice due to concerns about liver toxicity and less stable testosterone levels compared to gels or injections. | |
High-dose intramuscular testosterone enanthate Hint: Parenteral testosterone can be used in hypogonadism treatment, but high doses are not usually the initial approach due to the risk of erythrocytosis and other side effects. Dosing should aim for mid-normal serum testosterone levels. | |
Clomiphene citrate Hint: This is used primarily for treating infertility due to hypogonadotropic hypogonadism and is not the standard treatment for typical hypogonadism with low testosterone levels. | |
Transdermal estrogen patch Hint: Estrogen therapy is not used in the treatment of male hypogonadism. Testosterone replacement is the appropriate therapy for hypogonadal men. |
|
List |
References: Merck Manual · UpToDate