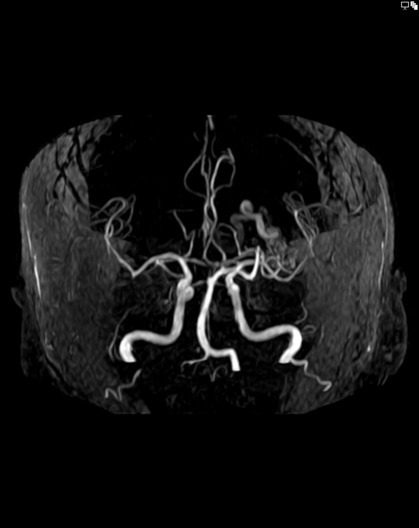
Patient will present as → a 63-year-old illiterate female with a history of right motor partial seizures and generalization since the age of 23 years arrives at the emergency room due to acute right hemiparesis. Neurological examination reveals a right hemiparesis, right tactile and pain hypoesthesia, poor fluency, temporal and spatial disorientation, and a Mini-Mental State Examination score of 5 points (one for immediate memory, two for naming, one for repetition, and one for commands). MRI is performed, demonstrating a massive AVM in the left hemisphere of the frontotemporoparietal region (9.2 × 6.0 cm) with parenchymal compression and microangiopathy.
Arteriovenous malformation is an abnormal connection between arteries and veins, bypassing the capillary system.
- Arteriovenous malformations (AVMs) are the most dangerous of the congenital vascular malformations, with the potential to cause intracranial hemorrhage and epilepsy in many cases
- Brain AVMs occur in about 0.1 percent of the population, one-tenth the incidence of intracranial aneurysms
- Supratentorial lesions account for 90 percent of brain AVMs
- Brain AVMs underlie 1 to 2 percent of all strokes, 3 percent of strokes in young adults, and 9 percent of subarachnoid hemorrhages
Brain AVMs are usually present between the ages of 10 and 40 years. In about half of all brain AVMs, intracranial hemorrhage is the first sign (41 to 79 percent)
In people without hemorrhage, signs and symptoms of a brain AVM may include:
- Seizure: 11-13 percent of patients with AVM present with seizure
- Headache: 0.2 percent of patients with headache and normal neurologic examinations were found to have an AVM
- Focal neurologic deficit
Risk factors include being male and having a family history of AVM
Angiography is the gold standard for the diagnosis, treatment planning, and follow-up after treatment of brain AVMs
- Brain AVMs are typically first identified on cross-sectional imaging (CT or MRI). MRI is more sensitive, particularly in the setting of an acute intracerebral hemorrhage
- A combination of MRI and angiography is often used to assess the likely success and risks of surgical, endovascular, or radiosurgical therapy
Surgical excision is the mainstay of treatment; radiosurgery is a useful option in lesions deemed at high risk for surgical therapy, and endovascular embolization can be a useful adjunct to these techniques
- Treatment for brain AVMs can be symptomatic, and patients should be followed by a neurologist for any seizures, headaches, or focal neurologic deficits
 Osmosis Osmosis |
|
 |
Subarachnoid hemorrhage (SAH) is a bleed in the subarachnoid space, which occurs most commonly due to rupture of a berry aneurysm. It can also occur from trauma and AVM. Patients often complain of the ‘worst headache of my life.
Play Video + QuizQuestion 1 |
Contrast-enhanced Computed Tomography (CT) Hint: While useful for initial assessment, CT with contrast does not offer the same level of vascular detail as DSA for diagnosing AVMs. | |
Magnetic Resonance Imaging (MRI) Hint: MRI is beneficial for visualizing AVMs and assessing their impact on surrounding brain tissue but lacks the vascular detail provided by DSA. | |
Digital Subtraction Angiography (DSA) | |
Carotid Doppler ultrasound Hint: This imaging modality is used for assessing blood flow in the carotid arteries, not for detailed visualization of AVMs. | |
Functional MRI (fMRI) Hint: fMRI is primarily used to map brain activity and is not a standard diagnostic tool for AVMs. It does not provide the detailed vascular imaging necessary for diagnosing AVMs. |
Question 2 |
Headache Hint: 0.2 percent of patients with a headache and normal neurologic examinations were found to have an AVM | |
Seizure Hint: 11-13 percent of patients with AVM | |
Intracranial hemorrhage | |
Focal neurologic deficit Hint: This presentation is fairly unusual for cerebral AVM. While a vascular steal syndrome has been hypothesized to cause this presentation, in most cases this is related to mass effect, hemorrhage, or seizure. | |
Visual disturbances Hint: Visual symptoms may occur depending on the AVM's location, especially if it affects the occipital lobe or optic pathways. However, they are less common as an initial symptom compared to headaches. |
Question 3 |
Conservative management with regular follow-up | |
Immediate surgical resection Hint: Indicated for symptomatic, accessible AVMs or those that have bled. | |
Stereotactic radiosurgery Hint: Considered for small, surgically inaccessible AVMs, more so if symptomatic. | |
Anticoagulation therapy Hint: Not a treatment for AVM and could increase the risk of hemorrhage. | |
High-dose corticosteroids Hint: Used to reduce edema in certain neurological conditions, not for managing AVMs. |
|
List |
References: Merck Manual · UpToDate