The NCCPA™ PANCE Cardiology System Content Blueprint covers 10 different conduction disorders
Conduction Disorders Quick Cram
| Normal sinus rhythm | Regular rhythm of the heart cycle stimulated by the SA node with an average heart rate of 60-100 bpm |
| Sinus tachycardia | Sinus rhythm but with a heart rate over 100 bpm |
| Sinus bradycardia | Sinus rhythm with a resting heart rate of < 60 bpm in adults or below the normal range for age in children |
| Atrial fibrillation/flutter | Irregularly irregular rhythm with disorganized and irregular atrial activations and an absence of P waves
Regular, sawtooth pattern and narrow QRS complex |
| Atrioventricular block | First Degree AV Block: PR interval is longer than 0.2 seconds or one block on EKG
Type I Second Degree (Wenckebach): progressive lengthening of the PR interval, then missed QRS complex Type II Second Degree (Mobitz): fixed PR interval with occasional dropped QRS complexes Third Degree AV Block: no association between the P wave and QRS complex |
| Bundle branch block | Left: R and R’ (upward bunny ears) in V4-V6
Right: R and R’ (upward bunny ears) in V1-V3 |
| Paroxysmal supraventricular tachycardia | Narrow complex tachycardia |
| Premature Beats | PVC: Early wide, bizarre QRS, no p wave seen
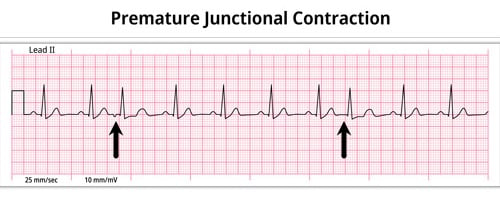
PAC: abnormally shaped P wave PJC: Narrow QRS complex, no p wave or inverted p wave |
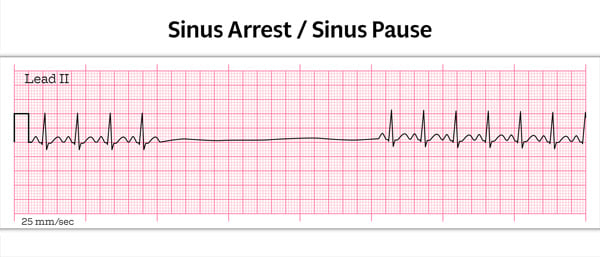
| Sick sinus syndrome | Brady-tachy: Arrhythmia in which bradycardia alternates with tachycardia
Sinus arrest: prolonged absence of sinus node activity (absent P waves) > 3 seconds |
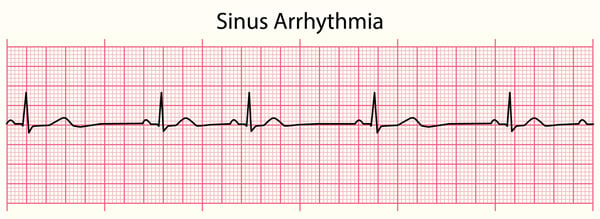
| Sinus arrhythmia | Normal, minimal variations in the SA Node's pacing rate in association with the phases of respiration. Heart rate frequently increases with inspiration and decreases with expiration |
| Torsades de pointes | Polymorphic ventricular tachycardia that appears to be twisting around a baseline |
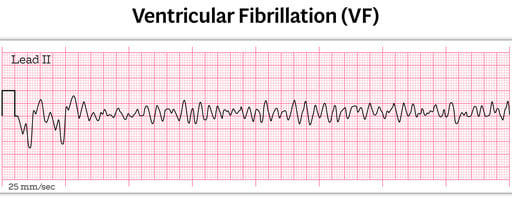
| Ventricular fibrillation | Erratic ventricular rhythm without identifiable P waves, QRS complexes, or T waves |
| Ventricular tachycardia | Wide complex tachycardia with three or more consecutive ventricular premature beats |
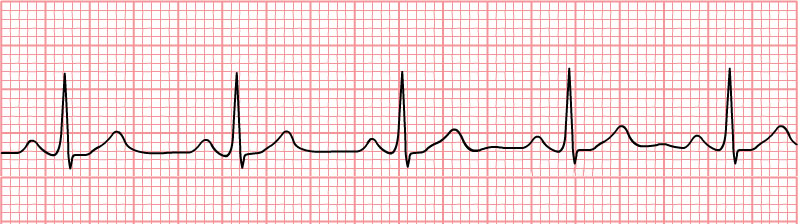
Normal Sinus Rhythm
Normal sinus rhythm refers to both a normal heart rate and rhythm.
- Normal heart rates are from 60 to 100 beats per minute.
- Electrical impulse originates in the sinoatrial node (SA).
- P waves are upright and appear before each QRS and have the same shape.
- Intervals between the P waves are regular although some variations can occur with respiration.
Sinus Tachycardia
Sinus tachycardia is a normal sinus rhythm but with a heart rate over 100 bpm.
- It is a normal response to exercise, excitement, and some illnesses
Sinus Bradycardia
Sinus bradycardia is a sinus rhythm with a rate of 40-60 bpm
Irritable sites in the atria fire very rapidly, between 400-600 bpm
- This very rapid pacemaking caused the atria to quiver
- The ventricles beat at a slower rate due to the AV node is blocking of some of the atrial impulses
Presentation:
- Elderly, excessive alcohol use
- Symptoms range from syncope, dyspnea, palpitations to no symptoms
- Irregularly irregular pulse
EKG: Low-amplitude fibrillatory waves without discrete P waves and an irregularly irregular pattern of QRS complexes
Treatment:
- Rate: Calcium channel blocker (diltiazem, verapamil) or beta-blocker (metoprolol)
- Rhythm:
- Duration <48 hours - cardioversion, amiodarone (obtain echo to determine if a clot is present prior
to cardioversion) - Duration >48 hours - anticoagulation for 21 days prior to cardioversion
- Duration <48 hours - cardioversion, amiodarone (obtain echo to determine if a clot is present prior
Anticoagulation is determined by CHA2DS2-VASc or CHADS2 scoring to assess the risk of stroke
- 0 points – no therapy or 81–325 mg/day of aspirin
- 1 point – either 81–325 mg/day of aspirin or anticoagulation
- 2 or more points – anticoagulation
There are two types of atrial flutter
- Type I (also called classical or typical) has a rate of 250-350 bpm
- Type II (also called non-typical) are faster, ranging from 350-450 bpm
EKG: Regular, sawtooth pattern (F-waves), narrow QRS complex
Occasionally occurs in COPD, congestive heart failure, atrial septal defect, coronary artery disease
Similar treatment as atrial fibrillation
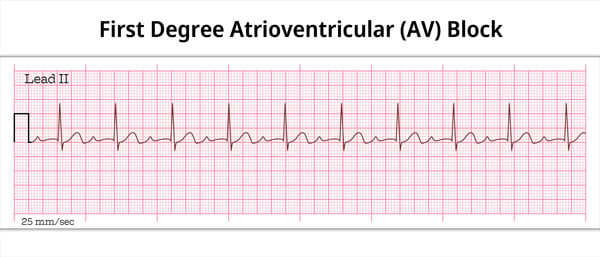
- 1st degree AV block: PR interval > .2 seconds
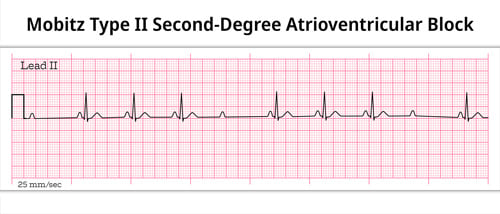
- 2nd degree AV block (Mobitz) two types:
- Mobitz type 1 (Wenckebach) – longer, longer, drop now you’ve got a Wenckebach
- Mobitz type 2 – some get dropped some get through now you’ve got Mobitz 2
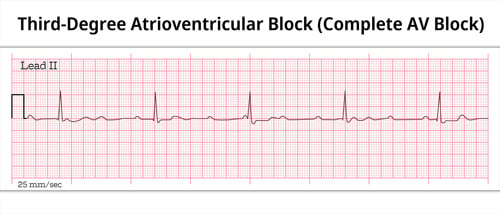
- 3rd degree (complete block): P’s and Q’s don’t agree now you’ve got 3rd degree
First degree AV block
PR interval > .2 seconds
First-degree heart block is actually a delay rather than a block. It is caused by a conduction delay at the AV node or bundle of His. This means that the PR Interval will be longer than normal (over 0.20 seconds) without disruption of atrial to ventricular conduction.
- (PR interval longer than 1 big box 0.20 seconds)
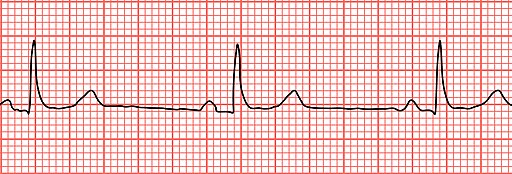
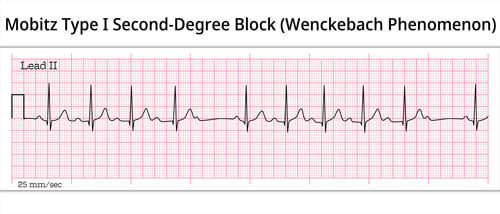
Second degree AV block Type 1 (Wenckebach) and Type 2 (Mobitz)
Type I: Wenckebach block
Wenckebach (longer, longer, longer drop now you've got a Wenckebach)
- With second-degree heart block, Type I (Wenckebach) some impulses are blocked but not all. More P waves can be observed vs QRS Complexes on a tracing
- Each successive impulse undergoes a longer delay. After 3 or 4 beats the next impulse is blocked
- On an EKG tracing, PR Intervals will lengthen progressively with each beat until a QRS Complex is missing. After this blocked beat, the cycle of lengthening PR Intervals resumes
- The Wenckebach pattern tends to repeat in P:QRS groups with ratios of 3:2, 4:3 or 5:4
Type II: Mobitz
MOBITZ 2 (some get dropped some get through now you've got mobitz 2)
With Mobitz Type II blocks, the impulse is blocked in the bundle of His. Every few beats there will be a missing beat but the PR Interval will not lengthen.
Third-degree AV block (complete heart block)
P’s and Q’s don’t agree now you've got 3rd degree
With this block, no atrial impulses are transmitted to the ventricles.
As a result, the ventricles generate an escape impulse, which is independent of the atrial beat. In most cases, the atria will beat at 60-100 bpm while the ventricles asynchronously beat at 30-45 bpm.
- There is no electrical communication between the atria and the ventricles, causing complete AV dissociation. P waves do not match the QRS one-for-one
With this conduction block, either the left or right bundle branch is blocked intermittently or fixed
The QRS complex is wider than normal (> 0.12 sec.)
Using a 12 lead EKG, blocks in either the left or right bundle branch may be diagnosed.
- QRS complex > .12 seconds
- May be due to MI
- Left: R and R’ (upward bunny ears) in V4-V6
- Right: R and R’ (upward bunny ears) in V1-V3
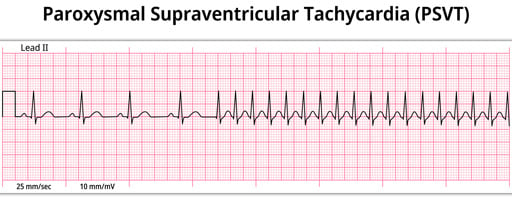
Paroxysmal supraventricular tachycardia
Summary of supraventricular tachycardia:
Heart rate: 150-250 BPM
Types:
- Paroxysmal supraventricular tachycardia (PSVT) – no structural abnormalities
- AV nodal reentrant tachycardia (AVNRT) – a small extra pathway exists in or near the AV node
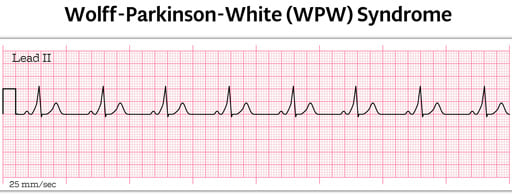
- Wolff Parkinson White (WPW) – presence of an abnormal accessory electrical conduction pathway between the atria and the ventricles – Bundle of Kent fibers and delta wave on EKG
- Atrial tachycardia (AT) is responsible for about 5 percent of PSVTs. It occurs when an electrical impulse fires rapidly from a site outside the sinus node and circles the atria, often due to a short circuit. In AT, the ECG shows identical P waves with a consistent rhythm.
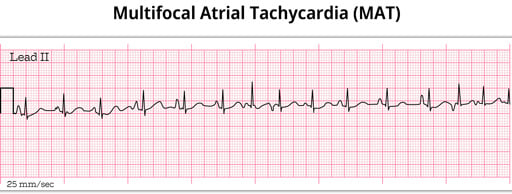
- Multifocal atrial tachycardia (MAT): Characterized by multiple ectopic foci within the atria firing electrical impulses erratically, resulting in a rapid and irregular atrial rhythm. The ECG shows different P wave shapes originating from different atrial locations.
Treatment:
- Valsalva for stable patients
- Adenosine for symptomatic patients
- Definitive treatment: Radiofrequency ablation
- WPW- do not administer adenosine or calcium channel blockers
Paroxysmal supraventricular tachycardia (PSVT)
A faster-than-normal heart rate beginning above the heart's two lower chambers in the atria, AV junction, or SA node associated with no structural abnormalities
Atrioventricular nodal reentrant tachycardia (AVNRT)
- A small extra pathway exists in or near the AV node
- If an electrical impulse enters this pathway, it may start traveling in a circular pattern that causes the heart to abruptly start beating fast and regular
Wolff-Parkinson-White Syndrome
This occurs when the impulse travels between the atria and ventricles via an abnormal path, called the bundle of Kent
- The impulse, not being delayed by the AV node, can cause the ventricles to contract prematurely
- EKG characteristics include a shorter PR Interval, longer QRS complex, and a delta wave (click here)
Multifocal Atrial Tachycardia
When multifocal atrial tachycardia occurs, multiple (non-SA) sites are firing impulses.
- EKG: Rapid, irregular rhythm > 100 bpm. At least 3 distinct P-wave morphologies
- The PR Interval varies
- Ventricular rhythm is irregular
Premature atrial contractions (PAC), Premature junctional complexes (PJC) and premature ventricular contractions(PVC)
- Typically benign. May cause palpitations.
- Increased frequency with stimulants (Ie. Caffeine)
EKG: Irregular beats (three types)
- PVC – widened QRS
- PAC – abnormally shaped P wave
- PJC – narrow QRS usually measured at 0.10 sec or less
Every 3rd beat – trigeminy. Every other beat- bigeminy
Treatment: None or beta-blockers if symptomatic
Premature atrial beats
This occurs when an ectopic site within the atria fires an impulse before the next impulse from the SA node
- EKG: An abnormal (non-sinus) P wave is followed by a QRS complex
- If the ectopic site is near the SA node, the P wave will likely have a shape similar to a sinus rhythm. But this P wave will occur earlier than expected.
Premature junctional beats
Premature junctional complex (PJC) occurs when an irritable site within the AV node fires an impulse before the SA node. This impulse interrupts the sinus rhythm
- EKG: Narrow QRS complex, either (1) without a preceding P wave or (2) preceded by an abnormal P wave with a PR interval of < 120 ms
- The QRS complex will be narrow, usually measured at 0.10 sec or less
Premature ventricular contractions
Premature ventricular complexes (PVCs) occur when a ventricular site generates an impulse. This happens before the next regular sinus beat.
- EKG: Broad QRS complex (≥ 120 ms) with abnormal morphology.
- Look for a wide QRS complex, equal or greater than 0.12 sec
- The QRS complex shape can be bizarre
- The P wave will be absent
Population: Elderly
Historically referred to as sick sinus syndrome (SSS), now commonly known as sinus node dysfunction (SND), is a collective term used to describe dysfunction in the sinus node's automaticity and impulse generation
- Sinus bradycardia: Sinus rhythm with a resting heart rate of < 60 bpm in adults, or below the normal range for age in children
- Sinus pause: pause < 3 seconds
- Sinus arrest: pause > 3 seconds
- Tachy-Brady Syndrome: Episodes of alternating sinus tachycardia and bradycardia
Treatment: Pacemaker
Sinus arrhythmia represents normal, minimal variations in the SA Node pacing rate in association with the phases of respiration.
- Heart rate frequently increases with inspiration and decreases with expiration
Torsade de Pointes is a special form of ventricular tachycardia
- EKG: Polymorphic ventricular tachycardia that appears to be twisting around a baseline
- Etiology: Hypokalemia or hypomagnesemia
- Treatment: IV Magnesium sulfate
Chaotic irregular deflections of varying amplitude and no useful contractions
- No identifiable P waves, QRS complexes, or T waves
- Rate 150 to 500 per minute
- Amplitude decreases with duration (coarse VF -> fine VF)
Treat with unsynchronized cardioversion
- Unsynchronized cardioversion - start CPR
- Give 3 sequential shocks (120, 150, 180); assess rhythm
- If VF persists --> do CPR and intubate
- Administer two doses amiodarone 2-4 min. Administer 1 mg IV bolus epi every 3-5 minutes (will ↑ myocardial blood flow and ↓ cerebral blood flow and ↓ defib threshold)
An implantable cardioverter-defibrillator may be necessary
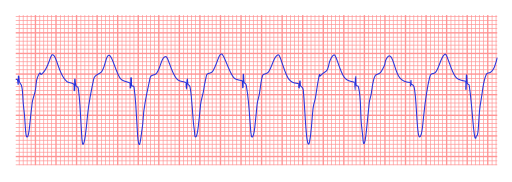
A sequence of three PVCs in a row is ventricular tachycardia.
- The rate will be 120-200 bpm.
- There are several different varieties of VT — the most being Monomorphic VT
Ventricular Tachycardia (Monomorphic)
Monomorphic ventricular tachycardia occurs when the electrical impulse originates in one of the ventricles. The QRS complex is wide. Rate is above 100 bpm.
EKG: Wide complex tachycardia
Treatment:
- Stable- amiodarone, lidocaine
- Unstable- CPR and defibrillation
Ventricular Tachycardia (Polymorphic)
Polymorphic ventricular tachycardia has QRS complexes that vary in shape and size. If a polymorphic ventricular tachycardia has a long QT Interval, it could be Torsade de Pointes.
Pacemaker Rhythm
Atrial and ventricular pacing can be seen on the ECG as a pacing stimulus (spike) followed by a P wave or QRS complex, respectively.
EKG: The appearance of the ECG in a paced patient is dependent on the pacing mode used, placement of pacing leads, device pacing thresholds, and the presence of native electrical activity
- EKG Pacing Spikes: Vertical spikes of short duration, usually 2 ms.
- It May be difficult to see in all leads