The NCCPA™ PANCE Cardiology System Content Blueprint covers five types of congenital heart disease. Congenital heart disease can be divided into two categories: cyanotic and noncyanotic
Congenital Heart Disease Quick Cram
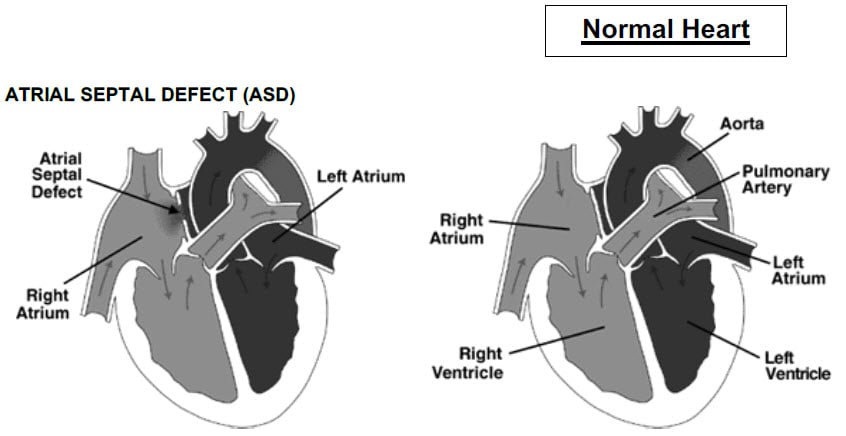
| Atrial septal defect | Systolic murmur heard best at the upper left sternal border with a wide, fixed, split s2 |
| Coarctation of the aorta | Grade II/VI murmur along the left sternal border that radiates into the left axilla and the left side of the back. Femoral pulses are decreased bilaterally. Rib notching on x-ray |
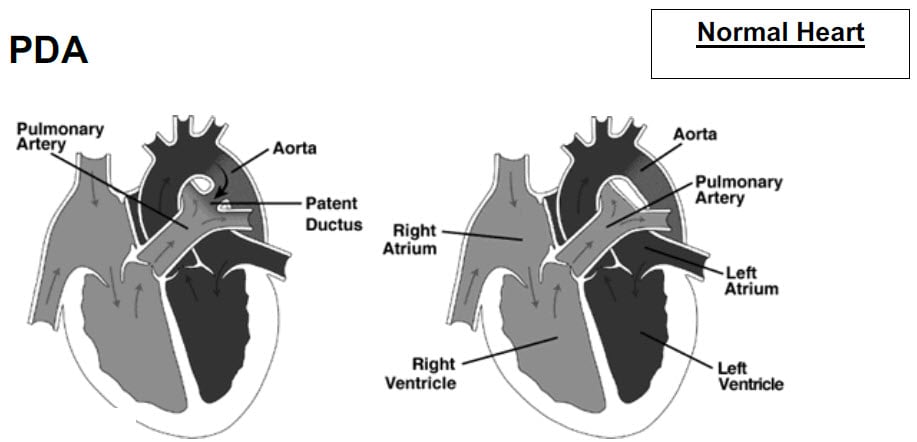
| Patent ductus arteriosus | A rough, continuous "machinery murmur" at the upper left sternal border (pulmonary area) |
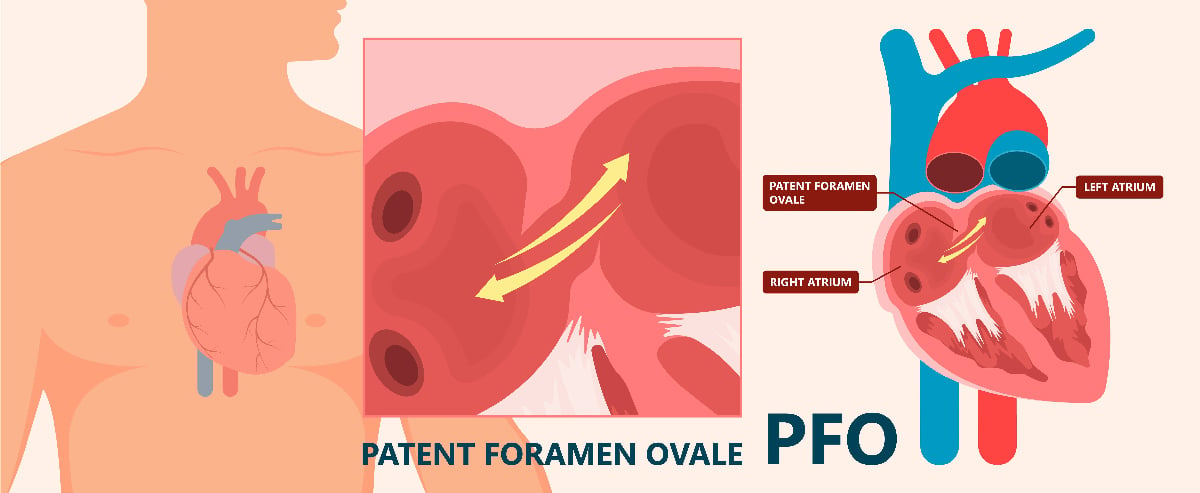
| Patent foramen ovale | Young patient with unexplained stroke or TIA |
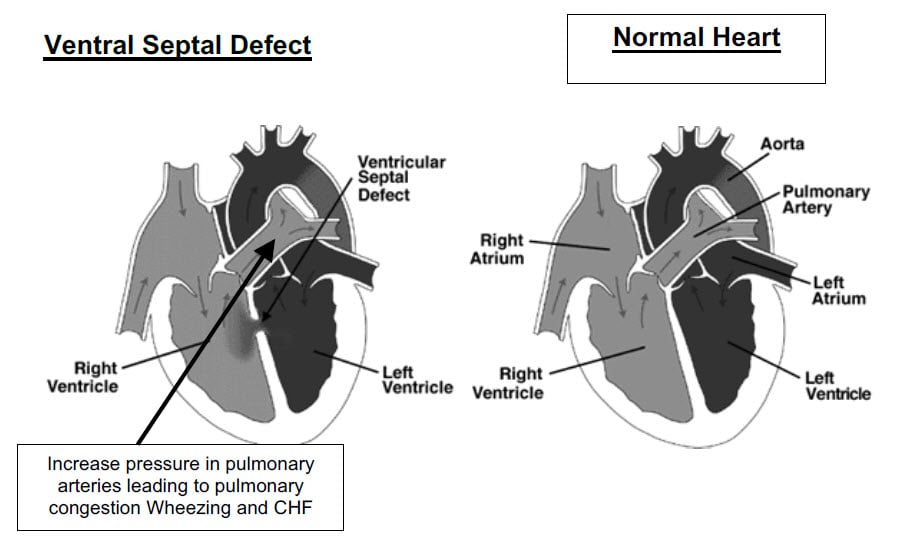
| Ventricular septal defect | Loud, harsh, pansystolic murmur at the lower left sternal border |
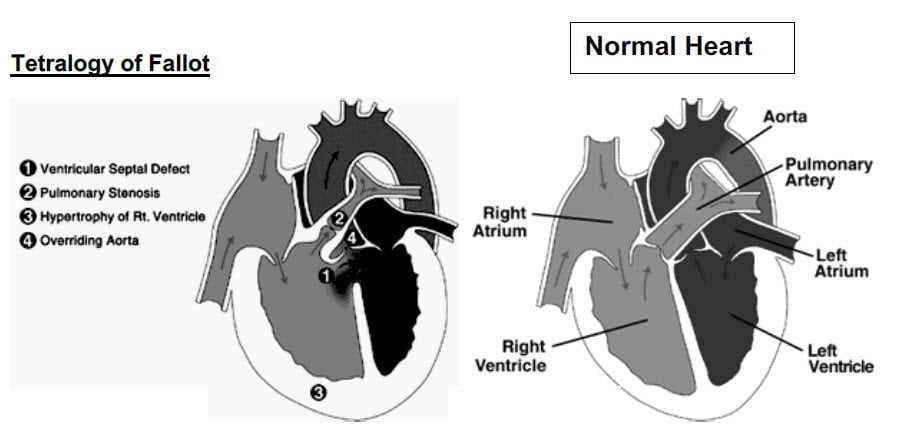
| Tetralogy of Fallot | Failure to thrive. "tet spells," baby with cyanosis and loss of consciousness with crying
Four features: PROVe
|
Non Cyanotic heart defects
| Atrial septal defect | Patient will present as → a 30-year-old woman with no significant past medical history presents to the clinic with complaints of increasing shortness of breath and palpitations, particularly during exercise. She also mentions a recent episode of fainting after climbing a flight of stairs. On examination, you note a grade III/VI systolic ejection murmur is present in the 2nd left intercostal space (pulmonic position) with an early to mid-systolic rumble and fixed splitting of the second heart sound (s2) during inspiration and expiration. She has no signs of heart failure. A chest X-ray reveals a prominent pulmonary artery, and an EKG shows a right bundle branch block. An echocardiogram is performed, which demonstrates a large secundum atrial septal defect (ASD) with a significant left-to-right shunt. Cardiac catheterization confirms the diagnosis, showing elevated pulmonary artery pressures. The patient is referred to a cardiologist for further management, including the possibility of surgical closure of the ASD to prevent long-term complications such as pulmonary hypertension and heart failure. Noncyanotic Foramen ovale fails to close. Ostium Secundum is most common Physical Exam: Wide, fixed, and split second heart sound (S2). Systolic ejection murmur at the second left intercostal space with an early to mid-systolic rumble. Failure to thrive. Diagnosis: Echocardiography - DEFINITIVE DIAGNOSIS will demonstrate a septal defect
Treatment:
|
| Coarctation of aorta | Patient will present as → a 15-year-old boy, previously healthy, presents to your clinic with complaints of leg fatigue and cramping after physical activities, especially when climbing stairs or playing soccer. He also reports frequent headaches. On examination, you find a significant discrepancy in blood pressure between his arms and legs, with higher readings in the arms. Additionally, there is a notable delay in the femoral pulse compared to the brachial pulse. Auscultation reveals a systolic murmur best heard in the left interscapular region. His medical history is unremarkable, and there are no known congenital heart defects in the family. However, he mentions that he has always been slightly shorter than his peers. CXR is performed, demonstrating a “figure of 3 sign” and an echocardiogram suggests a narrowing of the aorta distal to the left subclavian artery, consistent with coarctation of the aorta. A CT angiogram is ordered for further assessment, confirming the diagnosis and identifying the extent of the narrowing. The cardiology team is consulted for management, which may include surgical repair or balloon angioplasty, depending on the severity and anatomical characteristics of the coarctation. The patient is also started on antihypertensive medication to control his blood pressure until definitive treatment can be arranged. Noncyanotic - Typically found just after the vessels are given off to the left arm. This is a cause of high blood pressure, as the kidneys do not "see" as high of a blood pressure as they would like
Ejection murmur is heard at the aortic area and left sternal border that radiates into the left axilla and left back A bicuspid valve is seen in 50% of cases - also increases the incidence of cerebral berry aneurysm DX: Definitive Diagnosis is by echocardiography or by CT or MR angiography
TX: Treatment is balloon angioplasty with stent placement or surgical correction
|
| Patent ductus arteriosus | Patient will present as → a 6-month-old infant girl with a history of prematurity is brought to the PA for a routine check-up. Her mother mentions that the baby seems to tire more easily than expected during feeding and appears to breathe faster than her older child did at the same age. On examination, the PA notes a bounding pulse and a continuous machinery-like murmur best heard at the left upper sternal border at the second intercostal space (pulmonary area). The infant also shows mild tachypnea and tachycardia. Her growth is slightly below the expected percentile for her age. The PA orders an echocardiogram, which reveals a patent ductus arteriosus (PDA), a persistent connection between the aorta and the pulmonary artery. A consultation with a cardiologist is arranged, and they recommend starting the infant on a course of indomethacin, a medication that may help close the PDA. If medical management is unsuccessful, the possibility of surgical closure or catheter-based intervention is discussed to correct the defect, given the symptoms and impact on the infant’s growth and development. Noncyanotic - Ductus arteriosus is a normal fetal structure => If it remains open, it's called a patent ductus arteriosus
Rough “Machinery” murmur late in systole at the time of S2 making it loud
Diagnose: Echocardiogram Treatment: Indomethacin has been used to help close a PDA
|
| Patent foramen ovale | Patient will present as → a 38-year-old female presents to the clinic with a history of transient ischemic attack (TIA). She reports a sudden onset of speech difficulties and right-sided weakness that resolved completely within an hour. She has no prior history of strokes or TIAs, and her medical history is unremarkable. She does not smoke and has no family history of cardiac or thromboembolic diseases. On examination, she is neurologically intact. A thorough cardiovascular examination reveals no abnormalities, and her EKG is normal. Given her age and the unexplained nature of the TIA, a workup for cryptogenic stroke (stroke of undetermined etiology) is initiated. A transthoracic echocardiogram (TTE) with a bubble study is performed, showing bubbles passing from the right to the left atrium, indicating the presence of a patent foramen ovale. To further evaluate the PFO and rule out other structural heart diseases, a transesophageal echocardiogram (TEE) is conducted, confirming the diagnosis. The patient is counseled about the potential risks and benefits of PFO closure versus medical management. After discussing her options, she opts for medical management with antiplatelet therapy to reduce the risk of future thromboembolic events. A patent foramen ovale (PFO) is a persistent opening between the left and right atria of the heart, which normally closes shortly after birth. It is a common finding, present in up to 25% of the general population
DX: Transesophageal echocardiography (TEE) with bubble study is the definitive diagnostic tool, showing the passage of bubbles from the right atrium to the left atrium
TX: Treatment of PFO depends on the presence of symptoms and the risk of complications:
|
| Ventricular septal defect | Patient will present as → a 4-year-old boy who is brought to your office by his parents because he gets tired very easily and cannot keep up with the other children. On exam, you hear a loud, harsh, holosystolic murmur at the left lower sternal border without radiation to the axillae. An echocardiogram is performed and reveals a ventricular septal defect (VSD), with results seen here. Noncyanotic - VSD is the most common pathologic murmur in childhood
PE: Loud, harsh, holosystolic murmur, left to right - heard best at the lower left sternal border
DX: Echocardiogram Treatment: Most close by age 6, surgery if large |
Cyanotic defects
| Tetralogy of Fallot | Patient will present as → a 2-week-old newborn brought to the ER by his mom who reports a sudden loss of consciousness during feeding and with crying. She also has noticed that the infant’s lips have turned blue on three occasions during feeding. His blood pressure is 75/45 mmHg, his pulse is 170/min, and respirations are 44/min. A grade 3/6 harsh systolic ejection murmur is heard at the left upper sternal border. A CXR shows a small boot-shaped heart and decreased pulmonary vascular markings. Cyanotic Presentation: Difficult feeding, failure to thrive. "tet spells," a baby with cyanosis and loss of consciousness with crying Four features: PROVe
Physical exam: Crescendo-decrescendo, holosystolic murmur at LSB radiating to the back
DX: Echocardiography is the diagnostic modality of choice. This test can clearly define the four abnormalities as well as provide important information about aortic arch anatomy
Chest radiograph: Boot-shaped heart TX: Treatment is surgical. Most patients have surgery within the first year of life |