The NCCPA™ Cardiology PANCE and PANRE Content Blueprint covers 55 diseases
Cardiomyopathy |
|
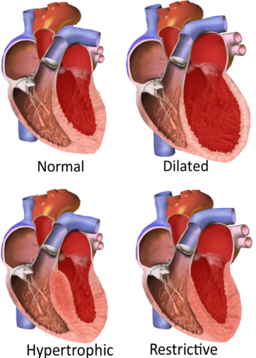
| Cardiomyopathy translates to “heart muscle disease,” so cardiomyopathy is a broad term used to describe a variety of issues that result from disease of the myocardium, or heart muscle | |
Types of cardiomyopathy
|
 |
| Impaired Systolic Function | |||||||||
| Dilated Cardiomyopathy | Patient will present as → a 68-year-old patient who comes to the office because of increased shortness of breath for four months. His symptoms are particularly bad at night. Medical history includes long-standing hypertension and alcoholism. Examination shows a displaced apex beat and normal breath sounds. Cardiac auscultation shows an S3 gallop and a pan-systolic murmur radiating to the axilla. The chest X-ray shows an enlarged left ventricular shadow. Dilated cardiomyopathy is the most common type (95%) of cardiomyopathy and is a condition in which an index event or process (such as an MI) damages the myocardium, weakening the heart muscle resulting in reduced strength of ventricular contraction, and dilation of the left ventricle
"An S3 gallop signifies the end of rapid ventricular filling in the setting of fluid overload and is often associated with dilated cardiomyopathy." DX: Echocardiography is the most definitive diagnosis - demonstrates left ventricular dilation and dysfunction and low cardiac output with poor EF (< 50%, but often less than 30%)
TX: βblocker + ACE + Loop Diuretic
|
||||||||
| Impaired Diastolic Function | |||||||||
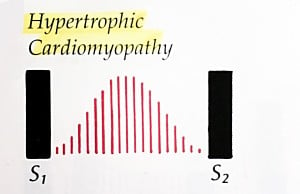
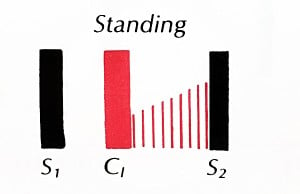
| Hypertrophic Cardiomyopathy | Patient will present as → a 25-year-old man is brought to the ED because he collapsed while playing tennis 20 minutes ago. Medical history includes unexplained chest pain and shortness of breath while exercising for three years. Family history includes an uncle who died of an unknown cardiac pathology at the age of 23. Cardiac auscultation shows a 2/6 systolic murmur is heard at the left of the sternum between the first two ribs. The murmur becomes louder when the patient performs a Valsalva maneuver and decreases with squatting. The hypertrophic portion of septum - LV outflow tract is narrowed - during systole and obstruction worsened with increased contractility Presentation: young athlete with a positive family history has sudden death or syncopal episode
Physical Exam:
"The murmur due to HCM will increase in intensity with any maneuver that decreases the volume of blood in the left ventricle (such as standing abruptly or the strain phase of a Valsalva maneuver ). " DX: Diagnosis is by echocardiography or MRI
TX: β-blockers (metoprolol) and/or rate-limiting Ca channel blockers (usually verapamil) to decrease myocardial contractility and slow the heart rate and thus prolong diastolic filling and decrease outflow obstruction
|
||||||||
| Restrictive Cardiomyopathy | Patient will present as → a 58-year-old man complaining of several months of worsening shortness of breath and ankle swelling. He denies palpitations, lightheadedness, syncope, or chest pain. He has a past medical history significant for hereditary hemochromatosis. On physical exam, his temperature is 37 C (98.6 F), pulse is 78, blood pressure is 130/72 mm Hg, and respiratory rate is 16. He has elevated jugular venous pressure, diminished breath sounds at the lung bases, tender hepatomegaly, and bilateral pitting ankle edema. There are no murmurs, rubs, or gallops. EKG shows low-voltage QRS complexes without any signs of ischemia. His chest x-ray shows a normal-sized heart and bilateral pleural effusions. Echocardiography shows symmetrical thickening of the left ventricle, normal left ventricular volume, and mildly reduced systolic function. Right heart failure with a history of an infiltrative process
DX: Echocardiography shows a normal left ventricular ejection fraction. Common findings include dilated atria and myocardial hypertrophy
TX: often unsatisfactory unless the cause can be addressed
|
||||||||
Conduction Disorders |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
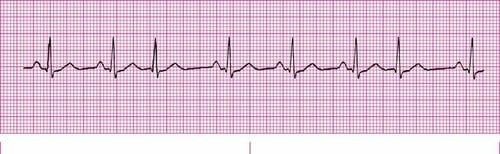
| Sinus Rhythm |
Normal Sinus Rhythm A normal sinus rhythm refers to both a normal heart rate and rhythm. Normal heart rates are from 60 to 100 beats per minute. The shape of the electrocardiogram (EKG) tracing will exhibit certain key attributes to be considered normal, as discussed below. With normal sinus rhythms, the heart beat's electrical impulse originates in the sinoatrial node (SA). The P waves are upright and appear before each QRS and have the same shape. The intervals between the P waves are regular although some variations can occur with respiration. Sinus Arrhythmia Sinus arrhythmia looks normal except for slight irregularities. A frequent cause of sinus arrhythmia can be rhythm variations caused by respiration. Sinus Tachycardia Sinus tachycardia is a normal sinus rhythm but with a heart rate over 100 bpm. It is a normal response to exercise, excitement and some illnesses. Sinus Bradycardia Sinus bradycardia is a sinus rhythm with a rate of 40-60 bpm. |
||||||||
| Atrial fibrillation/flutter (ReelDx) | Atrial Fibrillation
Low-amplitude fibrillatory waves without discrete P waves and an irregularly irregular pattern of QRS complexes Irritable sites in the atria fire very rapidly, between 400-600 bpm. This very rapid pacemaking caused the atria to quiver. The ventricles beat at a slower rate due to the AV node is blocking of some of the atrial impulses. Atrial Flutter There are two types of atrial flutter. Type I (also called classical or typical) has a rate of 250-350 bpm. Type II (also called non-typical) are faster, ranging from 350-450 bpm. EKG tracings will show tightly spaced waves or saw-tooth waveforms (F-waves). |
||||||||
| Atrioventricular block | First degree AV block
First-degree heart block is actually a delay rather than a block. It is caused by a conduction delay at the AV node or bundle of His. This means than the PR Interval will be longer than normal (over 0.20 sec.).
Second degree AV block Type 1 (Wenckebach) and Type 2 (Mobitz) Type I: Wenckebach block Wenckebach (longer, longer, longer drop now you've got a Wenckebach) With second-degree heart block, Type I, some impulses are blocked but not all. More P waves can be observed vs QRS Complexes on a tracing. Each successive impulse undergoes a longer delay. After 3 or 4 beats the next impulse is blocked. On an EKG tracing, PR Intervals will lengthen progressively with each beat until a QRS Complex is missing. After this blocked beat, the cycle of lengthening PR Intervals resumes. This heart block is also called a Wenckebach block. Type II: Mobitz MOBITZ 2 (some get dropped some get through now you've got mobitz 2) With Mobitz Type II blocks, the impulse is blocked in the bundle of His. Every few beats there will be a missing beat but the PR Interval will not lengthen. Third degree AV block With this block, no atrial impulses are transmitted to the ventricles. As a result, the ventricles generate an escape impulse, which is independent of the atrial beat. In most cases, the atria will beat at 60-100 bpm while the ventricles asynchronously beat at 30-45 bpm.
|
||||||||
| Bundle branch block | 
With this conduction block, either the left or right bundle branch is blocked intermittently or fixed. The QRS complex is wider than normal (> 0.12 sec.). Using a 12 lead EKG, blocks in either the left or right bundle branch may be diagnosed.
|
||||||||
| Paroxysmal supraventricular tachycardia | Supraventricular Tachycardia
A faster than normal heart rate beginning above the heart's two lower chambers in the atria, AV junction or SA node Wolff-Parkinson-White Syndrome This occurs when the impulse travels between the atria and ventricles via an abnormal path, called the bundle of Kent. The impulse, not being delayed by the AV node, can cause the ventricles to contract prematurely. EKG characteristics include a shorter PR Interval, longer QRS complex, and a delta wave. Multifocal Atrial Tachycardia When multifocal atrial tachycardia occurs, multiple (non-SA) sites are firing impulses. The P waves will vary in shape and at least three different shapes can be observed. The PR Interval varies. Ventricular rhythm is irregular. |
||||||||
| Premature beats | Premature atrial beats
This occurs when an ectopic sites within the atria fires an impulse before the next impulse from the SA node. If the ectopic site is near the SA node, the P wave will likely have a shape similar to a sinus rhythm. But this P wave will occur earlier than expected. Premature junctional beats Premature junctional complex (PJC) occurs when an irritable site within the AV node fires an impulse before the SA node. This impulse interrupts the sinus rhythm. The QRS complex will be narrow, usually measured at 0.10 sec or less. Premature ventricular contractions Premature ventricular complexes (PVCs) occur when a ventricular site generates an impulse. This happens before the next regular sinus beat. Look for a wide QRS complex, equal or greater than 0.12 sec. The QRS complex shape can be bizarre. The P wave will be absent. |
||||||||
| Sick sinus syndrome | 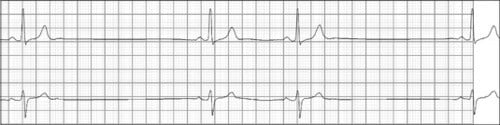
Episodes of alternating sinus tachycardia and bradycardia (tachy-brady syndrome), pacemaker placement |
||||||||
| Ventricular tachycardia | 
A sequence of three PVCs in a row is ventricular tachycardia. The rate will be 120-200 bpm. Ventricular Tachycardia has two variations, monomorphic and polymorphic. Ventricular Tachycardia Monomorphic Monomorphic ventricular tachycardia occurs when the electrical impulse originates in one of the ventricles. The QRS complex is wide. Rate is above 100 bpm. Ventricular Tachycardia Polymorphic Polymorphic ventricular tachycardia has QRS complexes that very in shape and size. If a polymorphic ventricular tachycardia has a long QT Interval, it could be Torsade de Pointes. |
||||||||
| Ventricular fibrillation | 
Ventricular fibrillation originates in the ventricles and it chaotic. No normal EKG waves are present. No heart rate can be observed. Ventricular fibrillation is an emergency condition requiring immediate action. |
||||||||
| Torsades de pointes | 
Torsade de Pointes is a special form of ventricular tachycardia. The QRS complexes vary in shape and amplitude and appear to wind around the baseline. |
||||||||
| Pacemaker Rhythm | 
Atrial and ventricular pacing can be seen on the electrocardiogram (ECG) as a pacing stimulus (spike) followed by a P wave or QRS complex, respectively. The ECG has the ability to show normal and abnormal pacemaker function. |
||||||||
Congenital Heart Disease |
|||||||||
| Atrial septal defect | Systolic ejection murmur at 2nd left intercostal space with an early to mid-systolic rumble and fixed splitting of the 2nd heart sound (s2)
|
||||||||
| Coarctation of aorta | Higher blood pressures in the arms than in the legs and pulses are bounding in the arms but decreased in the legs.
|
||||||||
| Patent ductus arteriosus | A continuous "machinery murmur" at the upper left sternal border, treat with indomethacin
** remember the patient got a patent for his machine! |
||||||||
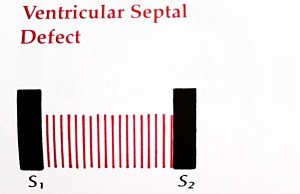
| Ventricular septal defect | VSD is the most common pathologic murmur in childhood, loud, harsh, holosystolic murmur at the lower left sternal border
|
||||||||
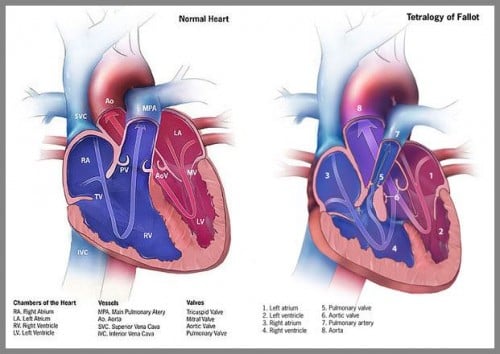
| Tetralogy of Fallot | Crescendo-decrescendo, holosystolic at LSB radiating to the back - cyanosis, clubbing,
Four features, "tet spells", baby with cyanosis and LOC with crying
|
||||||||
| Heart Failure (ReelDx) |
Systolic Left Heart Failure
Diastolic Left Heart Failure
Right heart failure (Right ventricle)
High output cardiac failure:
|
||||||||
Hypertension (PEARLS) |
|||||||||
| Primary hypertension | Down and dirty JNC 8 recommended treatment targets:
Cuff bladder should be 80% of arm circumference
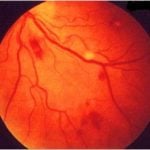
Workup: EKG, U/A, BUN/CR, K+, Retinopathy, CVA/TIA/PAD, CBC, lipids, Ca++ Lifestyle Modification Goals
|
||||||||
| Secondary hypertension | Usually chronic kidney disease or primary aldosteronism (2 most common causes)
Aldosteronism:
Chronic Kidney Disease
|
||||||||
| Hypertensive emergencies | Hypertensive Urgency = persistent asymptomatic SBP > 220 and/or diastolic > 125
Hypertensive Emergency = ↑ BP + target organ damage DBP > 130
Malignant Hypertension = Sustained elevated arterial blood pressure
|
||||||||
Hypotension (PEARLS) |
|||||||||
| Cardiogenic shock | Common causes: acute MI, heart failure, cardiac tamponade
|
||||||||
| Orthostatic hypotension | 20 mmHg drop in systolic BP, 10 mmHg drop in diastolic pressure, 15 BPM increase in pulse when patient 2-5 minutes after change from supine to standing
|
||||||||
Coronary Heart Disease (PEARLS) |
|||||||||
| Acute myocardial infarction | |||||||||
| Non-ST-Segment Elevation MI (NSTEMI) | Patient with acute crushing chest pain with evidence of myocardial necrosis (cardiac markers in blood; troponin I or troponin T and elevated CK) without acute ST-segment elevation or Q waves
Tx: Beta Blockers + NTG + Aspirin and Clopidogrel + Heparin |
||||||||
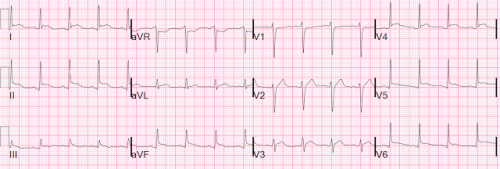
| ST-Segment Elevation Myocardial Infarction (STEMI) | Substernal chest pain radiating to the neck and arm with ST segment elevations > 1mm in > 2 contiguous leads on ECG and evidence of myocardial necrosis (cardiac markers in blood; troponin I or troponin T and elevated CK)
EKG:
Location of heart:
Serial cardiac enzymes:
Tx: Beta Blockers + NTG + Aspirin and Clopidogrel + Heparin + ACEI + reperfusion Aspirin and Clopidogrel given at once. Immediate (within 90 minutes) coronary angiography and primary PCI. Thrombolytic therapy within the first 3 hours if PCI not available. |
||||||||
Angina pectoris |
|||||||||
| Stable angina | Chest pain or discomfort that most often occurs with activity or emotional stress. Predictable, relieved by rest and/or nitroglycerine
Stress test: Reversible wall motion abnormalities/ ST depression >1 mm
|
||||||||
| Unstable angina | Chest pain or discomfort that most often occurs with activity or emotional stress. Previously stable and predictable symptoms of angina that are more frequent, increasing or present at rest
|
||||||||
| Prinzmetal variant angina | Coronary artery vasospasms causing transient ST segment elevations, not associated with clot
|
||||||||
Vascular Disease (PEARLS) |
|||||||||
| Aortic aneurysm/dissection | Aortic Aneurysm
Flank pain, hypotension, pulsatile abdominal mass Screening: Ultrasound, if male >65 and ever a smoker Treatment:
Aortic Dissection Sudden onset tearing chest pain, between scapulas. Diminished pulses Chest radiograph: Widened mediastinum Treatment:
|
||||||||
| Arterial embolism/thrombosis | Pain, pallor, pulselessness, paresthesia, paralysis and poikilothermia, Treat with IV heparin if not limb threatening then call the vascular surgeon | ||||||||
| Giant cell arteritis | Inflammation of large and medium vessels
Jaw claudication and headache, scalp pain elicited by touching the scalp or combing the hair, ESR > 100, diagnosed with Temporal artery biopsy, treat with high dose prednisone – do urgently to prevent blindness (Do not wait for biopsy results) Associated with polymyalgia rheumatica |
||||||||
| Peripheral artery disease | Intermittent claudication, Ankle-brachial-index< 0.9
Treatment:
|
||||||||
| Phlebitis/thrombophlebitis | Etiology: Spontaneous or after trauma, or IV/PICC lines
|
||||||||
| Varicose veins | Dilated tortuous superficial veins, venous stasis ulcers, ankle edema, treat with leg elevation and compression stockings
Lower extremity pain after sitting/standing |
||||||||
| Venous insufficiency | Edema, atrophic shiny skin, brawny induration, stasis dermatitis, brown hyperpigmentation, varicosities, ulcers above medial malleolus
Treatment: Sclerotherapy, vein stripping, compression hose |
||||||||
| Venous thrombosis | Unilateral swelling of lower extremity, D-dimer, venous duplex ultrasound first line imaging, Venography gold standard,
Risk factors:
Treatment: Heparin to Coumadin bridge |
||||||||
Valvular Disorders |
|||||||||
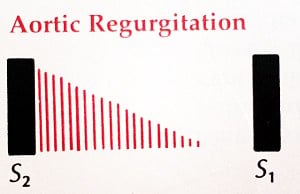
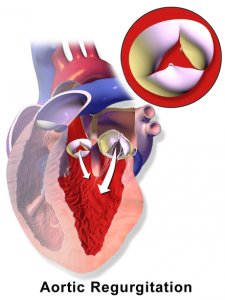
| Aortic regurgitation (Diastolic Murmur) | Soft HIGH PITCHED, BLOWING DIASTOLIC murmur along LSB with patient sitting, leaning forward after exhaling
|
||||||||
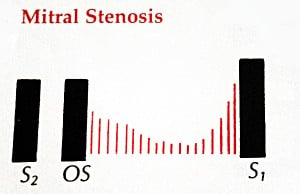
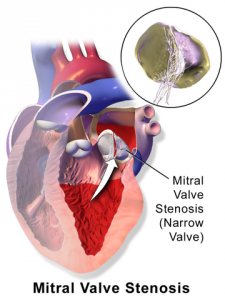
| Mitral stenosis | DIASTOLIC low-pitched DECRESCENDO and rumbling with OPENING SNAP at the APEX
|
||||||||
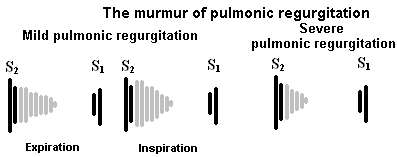
| Pulmonary regurgitation | High pitch, decrescendo murmur at LUSB, increases with inspiration
|
||||||||
| Tricuspid stenosis | MID DIASTOLIC RUMBLING at LLSB with OPENING SNAP
|
||||||||
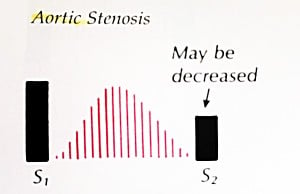
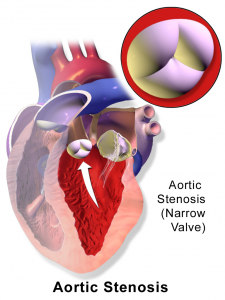
| Aortic stenosis (AS) | Systolic ejection crescendo-decrescendo RUSB
|
||||||||
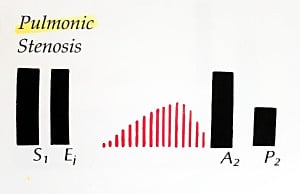
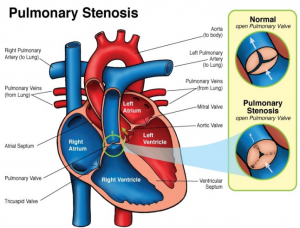
| Pulmonic stenosis | HARSH MIDSYSTOLIC EJECTION CRESCENDO-DECRESCENDO murmur with WIDELY SPLIT S2 at LSB that RADIATES TO THE LEFT SHOULDER & NECK
|
||||||||
| Hypertrophic Cardiomyopathy | Medium-pitched, mid-systolic murmur that decreases with squatting and increases with straining
|
||||||||
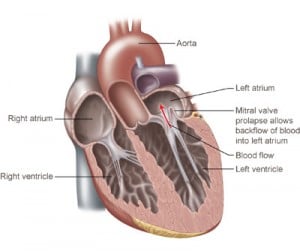
| Mitral valve prolapse | MIDSYSTOLIC EJECTION CLICK at APEX
|
||||||||
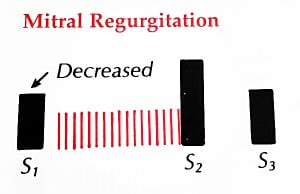
| Mitral regurgitation | BLOWING HOLOSYSTOLIC murmur at APEX with a SPLIT S2
|
||||||||
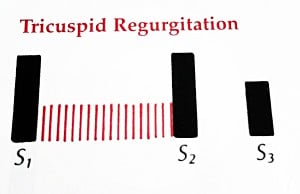
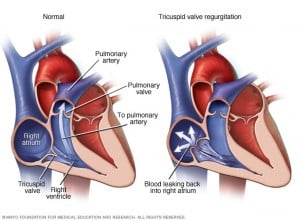
| Tricuspid regurgitation | HIGH PITCHED HOLOSYSTOLIC murmur at mid LSB
|
||||||||
| Ventricular septal defect | HARSH HOLOSYSTOLIC murmur heard best at the LSB with WIDE RADIATION and a fixed, split S2
|
||||||||
Other Forms of Heart Disease (PEARLS) |
|||||||||
| Acute and subacute bacterial endocarditis | Acute bacterial endocarditis: Infection of normal valves with a virulent organism (S. aureus)
Subacute bacterial endocarditis: Indolent infection of abnormal valves with less virulent organisms (S. viridans) Duke's criteria, staph aureus in acute and IV drug users, and strep viridians in subacute Classic signs of infective endocarditis
The murmur: |
||||||||
| Acute pericarditis | Chest pain that is relieved by sitting and/or leaning forward
Pericardial friction rub (listen and learn)
EKG will demonstrate diffuse, ST segment elevations in the precordial leads |
||||||||
| Cardiac tamponade | Fluid between the pericardial sac and the heart
The 3 D's: Distant heart sounds, Distended jugular veins, and Decreased arterial pressure = Beck's triad Beck’s triad:
Pulsus paradoxus is a classic finding for cardiac tamponade drop of BP > 10mm Hg of systolic BP with inspiration
 Pericardial effusion with "water bottle sign" |
||||||||
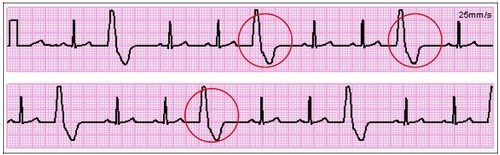
| Pericardial effusion | Same symptoms as acute pericarditis except patient will now have signs of fluid buildup around the heart which include low voltage QRS complexes, electrical alternans, distant heart sounds and an echocardiogram showing a collection of pericardial fluid
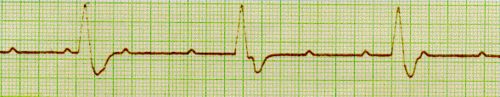
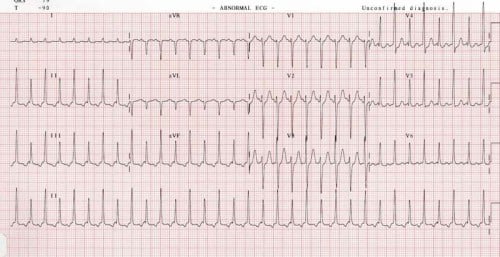 Electrical alternans as seen by changing QRS amplitudes best seen in lead II |
||||||||