Patient with stress incontinence will present as → a 68-year-old woman who presents to your office with leakage of urine when she sneezes, laughs, or coughs. She reports that these symptoms strictly occur during the day and never at night. She denies any subjective fever, dysuria, or hematuria. Pelvic examination is notable for a protrusion from the anterior vagina.
Patient with urge incontinence will present as → a 55-year-old woman comes to your clinic complaining of frequent episodes of sudden, intense urges to urinate that she cannot control, leading to urinary leakage. She reports that these episodes occur both during the day and at night. She denies any dysuria, hematuria, or fever. She has no significant past medical history and takes no medications. Physical examination, including a pelvic exam, is unremarkable. Urinalysis is normal
Patient with overflow incontinence will present as → a 68-year-old man with a history of benign prostatic hyperplasia and diabetes mellitus presents to your clinic complaining of frequent dribbling of urine and a sensation of incomplete bladder emptying. He also reports difficulty initiating urination and a weak urinary stream. Physical examination reveals a distended, non-tender lower abdomen. Post-void residual urine volume is measured at 350 mL.
Patient with functional incontinence will present as → a 78-year-old woman with a history of osteoarthritis and mild cognitive impairment is brought to your clinic by her daughter. The daughter reports that her mother has been experiencing episodes of urinary incontinence, especially when she tries to get to the bathroom. The patient uses a walker and takes time to get out of her chair. She denies any urgency, frequency, or nocturia. Physical examination and laboratory tests, including urinalysis, are unremarkable.
Patient with enuresis will present as → a mother and her 6-year-old son come to the office with a concern that he continues to have nighttime wetting several times a week. He is the second child of three. He is in the first grade and struggling with his performance. He has had no medical problems. There is no history of developmental delay, and he was the product of a normal uncomplicated pregnancy and delivery. Since the birth of the third child, his behavior has been problematic. The examination of other body systems is normal. He does not have laboratory evidence of a urinary tract infection.
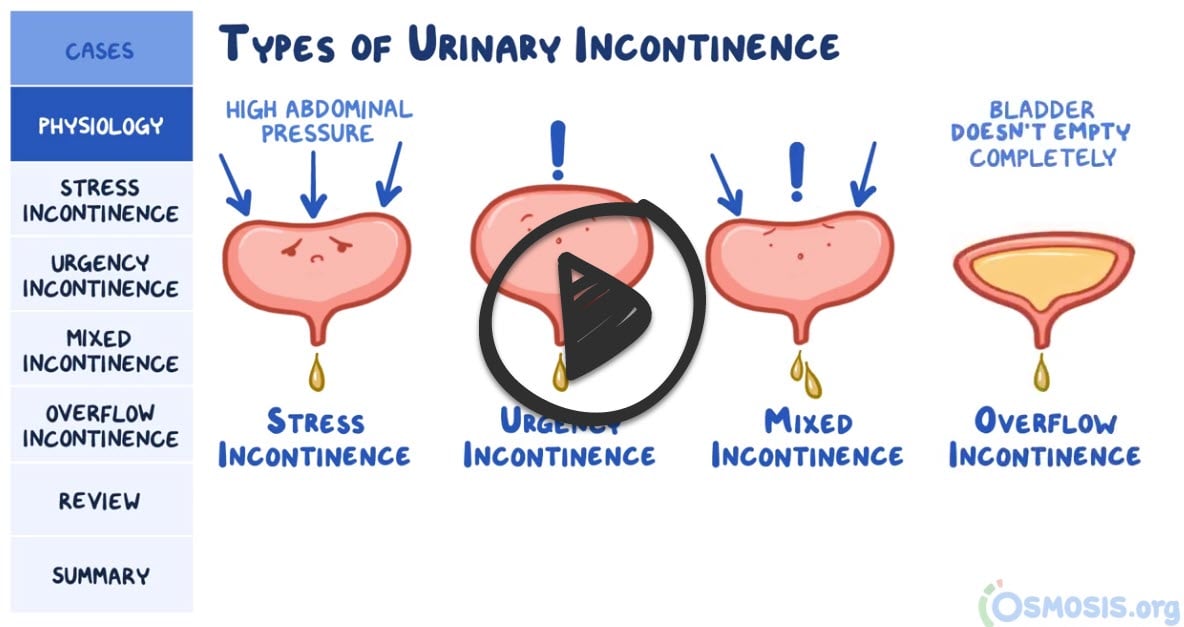
There are five major types of incontinence - affects 30% of elderly women and 15% of elderly men
1. Urge incontinence (detrusor overactivity)
- Most common in elderly and nursing home patients
- Overactive detrusor muscle results in increased frequency and involuntary loss of urine
- Sudden urge to urinate (e.g., patients are unable to make it to the bathroom), a loss of large volumes of urine with small postvoid residual, and nocturnal wetting
- Diagnostic study of choice is a urodynamic study
- The terms “urge incontinence” and “overactive bladder with incontinence“ are often used interchangeably
2. Stress incontinence (weakness of pelvic floor)
- Occurs mostly in women (after multiple deliveries of children)
- Weakness of the pelvic diaphragm (pelvic floor) leads to loss of bladder support (with resultant hypermobility of the bladder neck). This causes the proximal urethra to descend below the pelvic floor so that an increase in intra-abdominal pressure is transmitted mostly to the bladder (instead of an equal transmission to the bladder and urethra)
- Involuntary urine loss (only in spurts) during activities that increase intra-abdominal pressure (cough, laugh, sneeze, exercise); small postvoid volume
- Rule out infection with a urinalysis
3. Overflow incontinence (impaired detrusor contractility) cannot empty bladder - high postvoid volume
- Common in diabetic patients and patients with neurologic disorders
- Inadequate bladder contraction (due to impaired detrusor contractility) or a bladder outlet obstruction leads to urinary retention and subsequent overdistention of the bladder. Bladder pressure increases until it exceeds urethral resistance, and urine leakage occurs
- Causes include neurogenic bladder (diabetic patients, lower motor neuron lesions), medications (anticholinergics, α-agonists, and epidural/spinal anesthetics), obstruction to urine flow (BPH, prostate cancer, urethral strictures, severe constipation with fecal impaction)
- Nocturnal wetting, frequent loss of small amount of urine; large postvoid residual (usually exceeds 100 mL)
4. Functional incontinence - occurs in patients who have normal voiding systems, but who have difficulty reaching the toilet because of physical or mental disabilities
- Symptoms include increased urinary volume and the inability to timely urinate
5. Mixed incontinence (combo of stress and urge) - most common
Nocturnal enuresis is defined as involuntary urination in sleep without urologic or neurologic causes after the age of 5 years, at which time bladder control would normally be expected.
- The prevalence of enuresis decreases with increasing age. Thus, 82% of 2-year-old children, 49% of 3-year-old children, 26% of 4-year-old children, and 15% to 25% of 5-year-old children still wet beds on a regular basis.
Urinalysis to rule out UTI
- Postvoid residual urine volume to identify urinary retention
- Overflow has a high PVR
- Stress and urge have a normal/low PVR
- Urodynamic studies can identify bladder contractions
- Stress - normal bladder contractions
- Urge - increased bladder contractions during the filling phase
- Ultrasonography and cystoscopy can be used to determine anatomic abnormalities
The only mandatory laboratory evaluation for children with enuresis is urinalysis. The following are all important abnormalities that may be associated with enuresis:
- The presence of white blood cells in the urine as a result of a urinary tract infection
- Low urine specific gravity as a result of diabetes insipidus
- Proteinuria
- Hematuria as a result of renal disease
- Glucosuria as a result of diabetes mellitus
- Urine culture, CBC, IVP, and cystometric evaluation should be performed only if specific indications suggest the need. Posterior urethral valves (especially in boys) may be associated with enuresis
1. Urge incontinence (detrusor overactivity) is treated with bladder-training exercises (the goal is to increase the amount of time between voiding)
- If this is unsuccessful, medications include Beta-3 adrenergic agonist drugs (mirabegron and vibegron) and antimuscarinic agents (oxybutynin and solifenacin)
- Mirabegron is preferred over antimuscarinics like oxybutynin or solifenacin due to its lower side effect profile.
2. Stress incontinence (weakness of pelvic floor) is treated with Kegel exercises (multiple contractions of pelvic floor muscles as if patient were interrupting flow of urine) to strengthen pelvic floor musculature
- Vaginal estrogens
- Use of a pessary
- Surgery (there are various options, and a popular option is a mid-urethral sling)
3. Overflow incontinence (impaired detrusor contractility)
Treatment is primarily medical: intermittent self-catheterization is the best management
- cholinergic agents (e.g., bethanechol) to increase bladder contractions
- α-blockers (e.g., terazosin, doxazosin) to decrease sphincter resistance
4. Functional incontinence is treated with scheduled voiding times
5. Mixed - (combo of stress and urge) most common
- Lifestyle modifications and pelvic floor exercises are first-line
- If unresponsive to first-line treatments then therapy is based on the predominant symptoms
Treatment of enuresis is aimed at alleviation of the symptoms of nocturnal enuresis rather than cure of the condition
- Imipramine is no longer recommended for the treatment of enuresis in most children because of the potential for complications
- Desmopressin is useful in achieving dry nights, but patients often revert to pretreatment levels when the medication is discontinued
- A behavior modification program is the treatment of choice, including buzzer or bell and pad, positive reinforcement, charting of progress to increase confidence and self-esteem, urinating before bedtime, avoiding liquids after the evening meal, and avoiding psychological trauma through blame or belittling of the child
 Osmosis Osmosis |
|
 |
Functional incontinence is a form of urinary incontinence that occurs in patients who have normal voiding systems, but who have difficulty reaching the toilet because of physical or mental disabilities. Symptoms include increased urinary volume and the inability to timely urinate. The treatment for functional incontinence includes scheduled voiding times.
Play Video + QuizOverflow incontinence
Overflow incontinence is a form of urinary incontinence that is characterized by an involuntary, continuous loss of small amounts of urine due to a full bladder. Symptoms include increased urinary retention, involuntary urine dribble, and urinary frequency. Treatment options include medication such as bethanechol, catheterization, and sacral neuromodulation.
Stress incontinence
Stress incontinence is described by urine leaking with movement, and patients may state leakage occurs with coughing or sneezing, or with increased intra-abdominal pressure. Stress incontinence develops when there is laxity of the pelvic floor muscles, which leads to urethral sphincter insufficiency.
Play Video + QuizUrge incontinence
Urge incontinence symptoms include a strong urge to void, but they are typically unable to void quickly enough. Nocturia is a common complaint, as is increased urinary frequency, with subsequent small volume voids of urine. This all takes place because of increased detrusor muscle activity, which has numerous etiologies. Treatment includes avoiding caffeine and alcohol. Pharmacologic therapy includes anticholinergics and mirabegron, while other treatment modalities include botox injections and sacral neuromodulation.
Play Video + QuizQuestion 1 |
Refer for a cystoscopy Hint: Conservative therapy for stress incontinence should be attempted prior to any evaluation, such as cystoscopy, that might indicate the need for surgical correction. | |
Recommend Kegel exercises | |
Refer for surgical correction Hint: See A for explanation. | |
Recommend hormone replacement therapy Hint: There is no indication in the history for hormone replacement therapy and no vaginal atrophy was noted on pelvic examination. |
Question 2 |
oxybutynin chloride (Ditropan) Hint: Oxybutynin chloride is used for bladder spasms. It cannot be used for children under 5 years of age and is not indicated in primary enuresis. | |
imipramine (Tofranil) Hint: Imipramine is an older form of treatment that is moderately effective, but many patients relapse when therapy is stopped. This is no longer considered the treatment of choice. | |
trimethoprim-sulfamethoxazole (Bactrim) Hint: TMP-SMX is indicated for urinary tract infections that may cause secondary enuresis, but it is not used in primary enuresis. | |
desmopressin (DDAVP) |
Question 3 |
Desmopressin | |
Phenytoin Hint: Phenytoin is an anticonvulsant and is not used in enuresis. | |
Pramipexole Hint: Pramipexole is a dopamine agonist used in the treatment of restless leg syndrome. | |
Hyoscyamine Hint: Hyoscyamine is an anti-spasmodic used to treat overactive bladder. | |
Oxybutynin Hint: Monotherapy with anticholinergic drugs, such as oxybutynin, is not effective in treating monosymptomatic nocturnal enuresis. However, anticholinergic agents may be useful in children with nocturnal enuresis and daytime incontinence. In such children, anticholinergic therapy may be used in combination with desmopressin to increase bladder capacity during sleep. |
Question 4 |
Oxybutynin ER 5 mg daily Hint: See C for explanation | |
Solifenacin 5 mg daily Hint: See C for explanation | |
Mirabegron 25 mg daily | |
Midurethral sling surgery Hint: Midurethral sling surgery is for stress incontinence. | |
Fluid restriction Hint: Fluid restriction is not routinely needed. |
|
List |
References: Merck Manual · UpToDate






