Patient will present as → a 32-year-old male presents with a painless, firm mass in his right testicle that he discovered 2 weeks ago. Serum tumor markers, including alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (β-hCG), and lactate dehydrogenase (LDH) are elevated. Ultrasonography confirms the presence of a testicular mass. Orchiectomy reveals a mixed germ cell tumor.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
Presents as a firm, painless, nontender testicular mass
- Most common solid tumor in young men ages 15-40 (average age 32 years old)
- 5-year survival is 90% in most cases
- The most common type of testis cancer is a germ-cell tumor
- There are two main types of germ cell tumors: seminoma and non-seminomatous germ cell tumors (NSGCT)
- Both seminoma and NSGCT occur at about the same rate, and men can have seminoma, NSGCT, or a combination of both
- Subtypes of seminoma include:
- Classic seminoma (95%)
- Spermatocytic seminoma
- There are four main types of NSGCT that can appear alone but most often appear as a “mixed” NSGCT, with more than one type present:
- Embryonal carcinoma
- Yolk sac carcinoma
- Choriocarcinoma
- Teratoma
- Subtypes of seminoma include:
- Risk factors include a history of cryptorchidism
There is no evidence that screening asymptomatic men at average risk for testicular cancer with ultrasound, serum tumor markers, or clinical examination reduces mortality from testicular cancer. Men should be informed about the signs and symptoms of testicular cancer, but routine screening is not recommended.
- The USPSTF reaffirms its recommendation against screening adolescent or adult males for testicular cancer by clinician examination or patient self-examination.
- The American Academy of Family Physicians recommends against routine screening for testicular cancer in asymptomatic adolescent and adult males.
- The American Academy of Pediatrics does not include screening for testicular cancer in its recommendations for preventive health care.
- Finally, the American Cancer Society does not recommend testicular self-examination.
Diagnostic studies include
- Scrotal ultrasound
- Radiologic studies to look for metastases (common metastases to the belly, brain, and lung)
- Alpha-fetoprotein (AFP) – (+) in Non-Seminomatous Germ Cell Tumors (NSGCT) not seminomas
- AFP can be elevated in patients with a number of other malignancies, including hepatocellular (liver) carcinoma, cancer of the stomach, pancreas, biliary tract, and lung
- Beta-Human chorionic gonadotropin (beta-hCG) – both seminomas and NSGCT
- beta-hCG can be elevated in a number of other malignancies, including cancers of the liver, lung, pancreas, and stomach
- Lactate dehydrogenase (LDH) – LDH is less specific for testis cancer than HCG or AFP. However, elevated LDH levels are correlated to high tumor burden in seminoma and recurrence in NSGCT
Orchiectomy with or without chemotherapy and radiation, depending on cell type
- Seminomatous tumors are radiosensitive and can be treated with radiation therapy
- Nonseminomatous tumors are radioresistant
- **Alpha-fetoprotein (AFP) can be used to identify early relapse in testicular cancer
 Osmosis Osmosis |
|
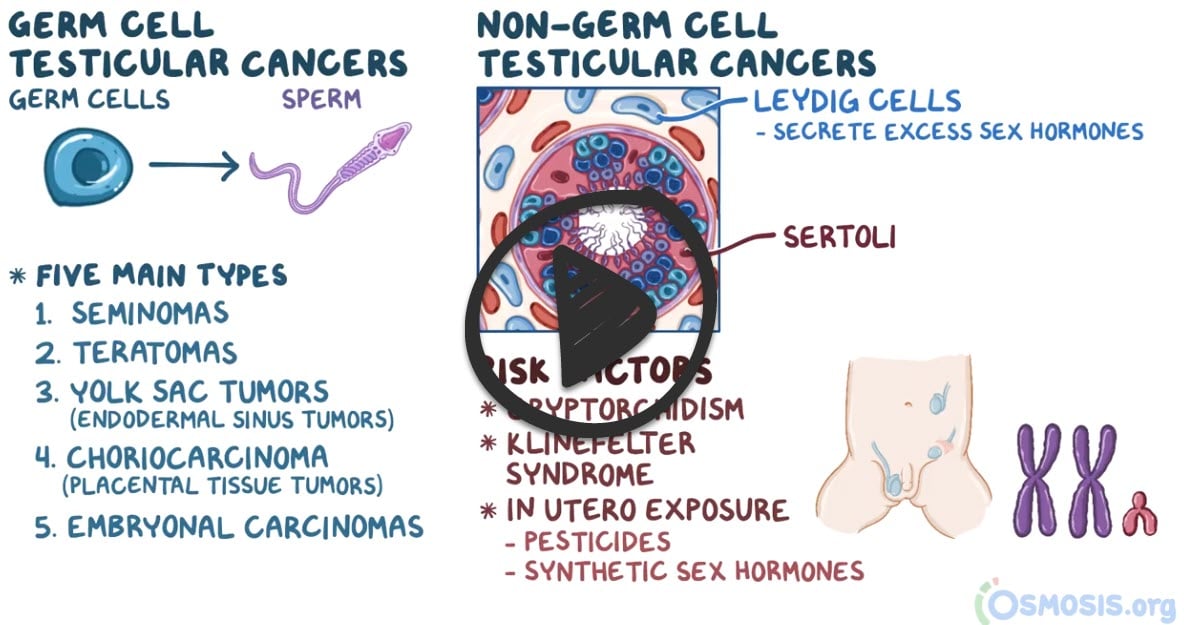 |
 Testicular carcinoma is the most common form of cancer in young males between 15-35 years old. The two main categories of testicular cancer are germ cell tumors (including seminomas and non-seminoma germ cell tumors) and sex cord-stromal tumors (including Leydig and Sertoli cell tumors). Germ cell tumors are most common. Cryptorchidism or undescended testes is a common risk factor of testicular cancer. Clinical manifestations include a painless scrotal mass, testicular swelling, and elevated serum tumor markers. Instruct the patient to perform a testicular self-examination once a month beginning at puberty. Treatment includes surgery, chemotherapy, and radiation. Since testicular carcinoma is one of the most curable types of cancers, early treatment yields good prognosis for long-term survival rates.
Testicular carcinoma is the most common form of cancer in young males between 15-35 years old. The two main categories of testicular cancer are germ cell tumors (including seminomas and non-seminoma germ cell tumors) and sex cord-stromal tumors (including Leydig and Sertoli cell tumors). Germ cell tumors are most common. Cryptorchidism or undescended testes is a common risk factor of testicular cancer. Clinical manifestations include a painless scrotal mass, testicular swelling, and elevated serum tumor markers. Instruct the patient to perform a testicular self-examination once a month beginning at puberty. Treatment includes surgery, chemotherapy, and radiation. Since testicular carcinoma is one of the most curable types of cancers, early treatment yields good prognosis for long-term survival rates.
| Testicular carcinoma assessment | Play Video + Quiz |
| Bleomycin | Play Video + Quiz |
| Etoposide | Play Video + Quiz |
Question 1 |
Watchful waiting Hint: Surveillance is an option in stage I disease of a nonseminoma testicular tumor. | |
Chemotherapy initially Hint: Patients with stage IIC and stage III are treated with chemotherapy. | |
Orchiectomy and radiation | |
Orchiectomy and chemotherapy Hint: Chemotherapy is used for later stage tumors (II/III) and followed by surgery in stage III tumors. |
Question 2 |
Low socioeconomic status Hint: High socioeconomic status, not low, is a risk factor. | |
History of cryptorchidism | |
Multiple episodes of epididymitis Hint: Multiple episodes of epididymitis are unrelated to the development of testicular cancer. | |
Being of African-American ethnicity Hint: The incidence of testicular cancer is much lower in African-American men than in Caucasian men. | |
Frequent bicycling Hint: While it may cause temporary discomfort or issues related to the scrotum, it's not a risk factor for testicular cancer. |
Question 3 |
Serum alpha fetoprotein levels (AFP) Hint: Although tumor markers are useful to follow patients with testicular cancer, they are not used as the initial screen. | |
Serum human chorionic gonadotropin hormone (HCG) Hint: Although tumor markers are useful to follow patients with testicular cancer, they are not used as the initial screen. | |
Computed tomography (CT) scan of the abdomen and pelvis Hint: CT scanning of the pelvis is most commonly used in the evaluation for metastatic disease and not used in the initial screen for testicular cancer. | |
Testicular ultrasound | |
Magnetic resonance imaging (MRI) of the scrotum Hint: Less commonly used than ultrasound for initial evaluation of a testicular mass. |
Question 4 |
Carcinoembryonic antigen (CEA) Hint: Carcinoembryonic antigen can be elevated in multiple conditions including colon cancer, gastritis, peptic ulcer disease, diverticulitis, liver disease, chronic obstructive pulmonary disease, and diabetes. | |
Prostate specific antigen (PSA) Hint: PSA is primarily used as a tumor marker in prostate cancer, not testicular cancer. | |
CA 125 glycoprotein Hint: CA 125 is used as a marker in ovarian cancer and certain other malignancies but is not a primary marker for testicular cancer follow-up. | |
Alpha fetoprotein (AFP) | |
Carbohydrate antigen 19-9 (CA19-9) Hint: CA19-9 is commonly used as a tumour marker for some types of cancer of the pancreas. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture

