Patient will present as → a 63-year-old man with a history of benign prostatic hyperplasia reports 3-days of fever, chills, and pain with urination. He was recently catheterized during admission to the hospital. Physical exam reveals a tender and enlarged prostate on digital rectal exam. Urinalysis reveals pyuria and hematuria.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
- Chlamydia and Gonorrhea in men < 35
- E coli in men > 35
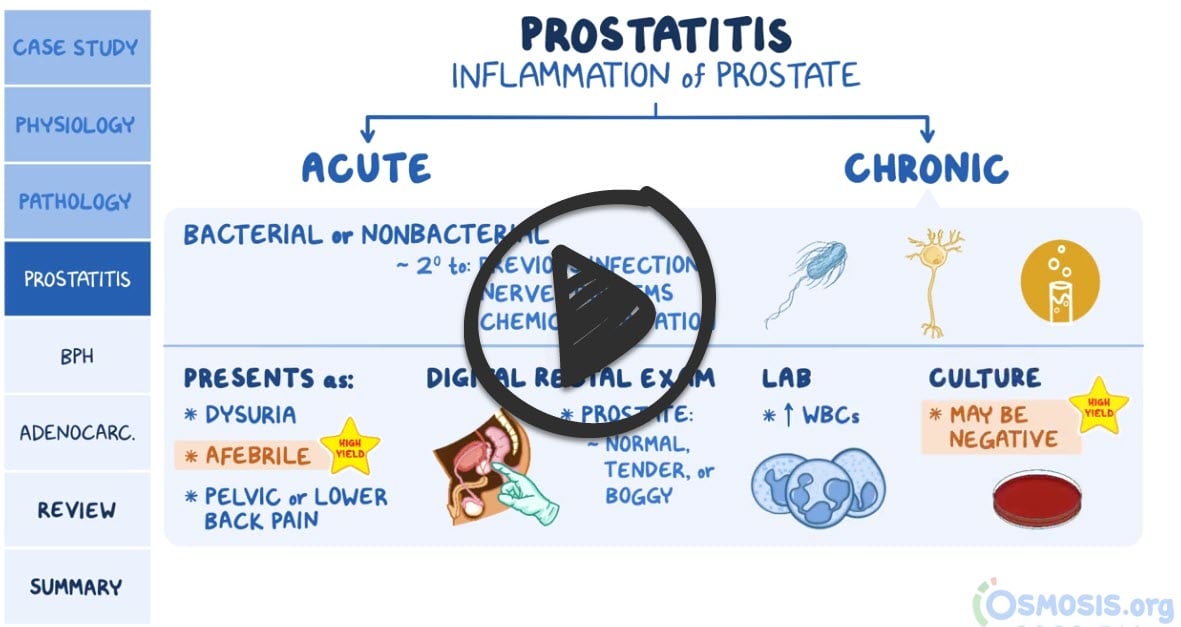
Prostatitis is inflammation of the prostate gland
- Prostatitis is classified into acute, chronic, asymptomatic inflammatory prostatitis, and chronic pelvic pain syndrome
- Causes include an ascending urinary tract infection, spread from the rectum (direct/via lymphatics), hematogenous (rare)
- May follow catheterization, cystoscopy, urethral dilation, prostate resection procedures
Acute bacterial prostatitis: Usually occurs in younger individuals and is a more serious condition
- Fever, chills, malaise
- Urinary symptoms ⇒ Frequency, urgency, dysuria
- Perineal/low back pain
- Digital rectal exam ⇒ Boggy, warm, tender, enlarged prostate
Chronic prostatitis: Can be bacterial/abacterial, and usually occurs in individuals aged 40–70 years; Chronic bacterial is the most common form of prostatitis
- Can be asymptomatic
- Intermittent urinary symptoms
- History of recurrent UTIs
- Perineal/low back pain; suprapubic discomfort
- Digital rectal examination ⇒ enlarged, nontender prostate
**If you suspect acute prostatitis, do not massage the prostate. This can lead to sepsis!
Urinalysis will reveal pyuria (↑ WBC in acute) +/- hematuria
- Urine cultures: positive in acute and negative in chronic prostatitis
- Prostatic fluid/secretions may show leukocytosis (↑ WBCs) with a culture typically positive for E Coli
- Ultrasound/CT scan/cystoscopy: For individuals with significant voiding dysfunction/suspected abscesses/neoplasms
- Blood tests: CBC, blood cultures if clinical findings suggestive of bacteremia
- Blood urea nitrogen and creatinine levels for individuals with urinary retention/obstruction
- Serum prostate-specific antigen (PSA) may be elevated
Case presentation - 24-year-old male complaining of blood in the ejaculate after intercourse with his girlfriend - think prostatitis and treat appropriately
- In this case and in men < 35 cover chlamydia and gonorrhea - ceftriaxone and doxycycline
- In older men > 35, treat with fluoroquinolones or Bactrim for 4-6 weeks to ensure eradication of the infection
- Patients who cannot tolerate oral medication, demonstrate signs of severe sepsis, or have bacteremia should be hospitalized. In such cases, intravenous levofloxacin or ciprofloxacin may be given with or without an aminoglycoside (gentamicin or tobramycin).
- Urinary retention ⇒ Alpha-blocking agents/suprapubic catheterization
"In men who have persistent fever and chills, inability to urinate, or low back pain despite initial treatment transrectal ultrasonography of the prostate gland is warranted and may help to detect prostate calculi or abscess."
- Chronic prostatitis is treated with fluoroquinolones or Bactrim x 6-12 weeks
 Osmosis Osmosis |
|
 |
Prostatitis is an inflammation of the prostate gland that may be caused by a bacterial, viral, or sexually-transmitted infection. Untreated prostatitis may progress to inflammation of the epididymis (epididymitis) or bladder (cystitis). Assessment findings include flu-like symptoms, perianal pain, dysuria, and sexual dysfunction. Oral or IV antibiotics may be administered to stop the infection. Pain may be managed with anti-inflammatory drugs, warm Sitz baths, stool softeners, and alpha-adrenergic blockers. Additional considerations include prostatic massage and increased fluid intake.
Play Video + QuizQuestion 1 |
Penicillin Hint: See D for explanation. | |
Cephalexin (Keflex) Hint: See D for explanation. | |
Nitrofurantoin (Macrobid) Hint: See D for explanation. | |
Levofloxacin (Levaquin) |
Question 2 |
prostatodynia Hint: Prostatodynia is an inflammatory disorder involving voiding dysfunction and pelvic floor musculature dysfunction. There is no bacterial involvement. | |
non-bacterial prostatitis Hint: Non-bacterial prostatitis is similar to chronic bacterial prostatitis, but no bacteria are cultured, and the cause is unknown. | |
acute bacterial prostatitis | |
chronic bacterial prostatitis Hint: Prostate massage can be performed in the absence of fever. Expressed prostatic secretions are cultured to help identify the organism. |
Question 3 |
cystitis Hint: Cystitis is characterized by dysuria without urethral discharge | |
gonococcal urethritis Hint: Initially there is burning on urination and serous or milky discharge in gonococcal urethritis. | |
epididymitis Hint: Epididymitis is characterized by dysuria, unilateral scrotal pain and swelling. | |
prostatitis |
Question 4 |
renal pelvis Hint: Total hematuria, blood throughout the urinary stream, suggests a bladder or upper urinary tract source. | |
bladder neck | |
anterior urethra Hint: Presence of blood at the beginning of the urinary stream suggests an anterior (penile) urethral source. | |
ureter Hint: Hematuria from the kidneys or ureter may be present microscopically or throughout the stream. |
Question 5 |
Ciprofloxacin | |
Ceftriaxone and doxycycline Hint: Ceftriaxone and doxycycline are used in the treatment of acute epididymitis due to sexually transmitted infection. | |
Azithromycin + Ceftriaxone Hint: This is used in the treatment of chlamydia and gonorrhea | |
Nitrofurantoin Hint: Nitrofurantoin is used in the treatment of acute cystitis and not indicated in acute prostatitis. |
Question 6 |
Insert a Foley catheter Hint: Urethral catheterization, or any form of instrumentation is contraindicated in the presence of acute bacterial prostatitis. | |
Initiate diuretic therapy Hint: Diuretic therapy is contraindicated in the treatment of acute urinary retention. | |
Schedule for cystoscopy Hint: See A for explanation. | |
Insert a percutaneous suprapubic tube |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture


