PANCE and PANRE Endocrine System Content Blueprint pituitary disorders
| Acromegaly/gigantism | Patient with acromegaly will present as → a 50-year-old man who comes to the clinic expressing concerns about noticeable changes in his appearance over the last five years. He mentions that he’s had to buy larger shoes and gloves due to swelling of his hands and feet. He also reports increased snoring and interrupted sleep, frequent headaches, and joint pain. On examination, he displays prominent brow ridges, an enlarged nose, thickened lips, and spaces between his teeth. Additionally, he has a deepened, husky voice and exhibits skin tags. An X-ray of the hand reveals enlarged finger bones. Magnetic resonance imaging (MRI) of the brain indicates an enlarged pituitary gland. Lab tests show elevated levels of insulin-like growth factor-1 (IGF-1). Patient with gigantism will present as → a 13-year-old boy brought in by his parents due to rapid growth over the past two years. They mention he’s much taller than his peers, and his shoe size has increased significantly. The parents also express concerns about his persistent headaches and excessive sweating. On examination, the boy displays elongated arms and legs, a protruding jaw, and enlarged hands and feet. His growth charts show he’s above the 99th percentile for height for his age group. A visual field test reveals peripheral vision loss. Laboratory tests indicate elevated levels of growth hormone (GH) and insulin-like growth factor-1 (IGF-1). An MRI of the brain reveals a pituitary adenoma. Etiology: Gigantism and acromegaly are usually caused by a pituitary adenoma that secretes excessive amounts of Growth Hormone; rarely, they are caused by non-pituitary tumors that secrete GHRH
Presentation:
Diagnosis:
Treatment: Pituitary tumor removal |
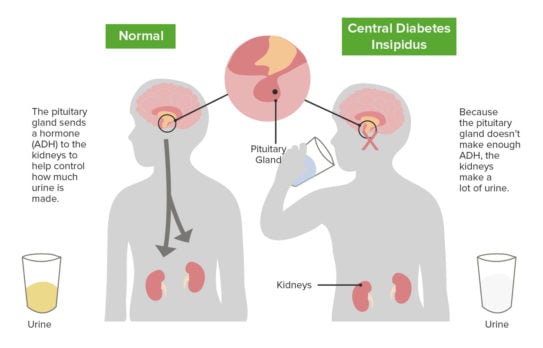
| Diabetes insipidus (ReelDx) | ReelDx Virtual Rounds (Diabetes insipidus)Patient will present as → a 25-year-old male complaining of an unabated thirst that began three weeks ago. He is constantly drinking and goes to the bathroom around five times a night. He has lost five pounds over the last few weeks. The patient is on lithium for bipolar disorder. His BP is 115/70. The patient’s labs are significant for serum Na of 145 mEq/L (normal: 135-145). Urine osmolality is 185 mOsm/kg, and urine specific gravity is 1.004 (normal: 1.012 to 1.030). Diabetes insipidus (DI) is caused by a deficiency of or resistance to vasopressin (ADH), which decreases the kidneys' ability to reabsorb water, resulting in massive polyuria
Diagnosis:
Serum osmolality (concentration) is high (unable to stop the secretion of water into the kidneys so blood becomes more concentrated), and urine osmolality is low because it is so dilute The water deprivation test is the simplest and most reliable method for diagnosing central diabetes insipidus but should be done only while the patient is under constant supervision. Serious dehydration may result
Treatment:
|
| Pituitary dwarfism | Patient will present as → a 3-year-old male who is brought to your office by his mother, who is concerned that he is not growing appropriately. Physical examination is notable for frontal bossing and shortened upper and lower extremities. His axial skeleton appears normal. He is at the 4th percentile for height and 95th percentile for head circumference. He demonstrates normal intelligence and is able to speak in three-word sentences. He first sat up without support at twelve months and started walking at 24 months. Labs reveal decreased GH and decreased IGF 1. Pituitary dwarfism, or growth hormone deficiency, is a condition in which the pituitary gland does not make enough growth hormone. This results in a child's slow growth pattern and unusually small stature (below average height) Growth hormone (GH) deficiency can occur in isolation or in association with generalized hypopituitarism. Causes include congenital (including genetic) disorders and a number of acquired disorders of the hypothalamus and/or pituitary
DX: Diagnosis can be confirmed by low levels of insulin-like growth factor-1 and insulin-like growth factor binding protein-3
Treatment: If dwarfism is due to decreased human growth hormone and not due to a primary skeletal disorder, the child can be treated with human growth hormone treatments to try and stimulate normal growth. Surgery may be necessary to remove a pituitary adenoma if that is the cause of dwarfism |
| Pituitary adenoma and Pituitary neoplastic disease | Patient will present as → a 31-year-old woman who complains of irregular, infrequent menstrual periods. On further questioning, she complains of headaches, fatigue, and breast discharge. She takes ibuprofen only occasionally. The serum prolactin level is 380 μg per L. (prolactinoma) The most common tumors are microadenomas that are functional (hypersecretion of pituitary hormones), nonfunctional or compressive
Diagnosis:
|
| Classification of Pituitary Adenomas | ||
| Tumor Type | Secretory Product(s) | Relative Frequency (%) |
1. Prolactinoma (Galactorrhea)
|
↑ Prolactin | 50% |
2. Somatotroph Adenoma (Acromegaly)
|
↑ Growth Hormone/Prolactin | 10% |
3. Corticotroph Adenoma (Cushing's Syndrome)
|
↑ ACTH | 5% |
4. Thyrotroph Adenoma (Hyperthyroidism)
|
↑ TSH | 1% |
5. Non-Secreting Adenoma
|
(α) alpha -subunit | 34% |
The posterior pituitary is an endocrine gland primarily composed of the nerve terminals of axons extending from the hypothalamus. It is important in the neuroendocrine reflex, which occurs when sensory neurons are stimulated resulting in action potential in hypothalamic cells and exocytosis of hormones from the posterior pituitary. Vasopressin is one of the hormones released from the posterior pituitary. Vasopressin is synthesized in the hypothalamus but stored in the posterior pituitary and released in response to synaptic input from osmoreceptors that detect increased osmolality of blood plasma. This hormone affects the kidney into retaining more water and also can constrict blood vessels. The second hormone released from the posterior pituitary is Oxytocin. It is released via a neuroendocrine reflex in response to stimulation of the nipples during breastfeeding that causes the mammary glands to contract and release milk. Stimulation of the nipples causes action potential generation in the oxytocin cells of the hypothalamus, which travels down to the nerve endings in the posterior pituitary and results in the exocytosis of Oxytocin. It also causes uterine smooth muscle contraction during the second and third stages of labor.
Play Video + QuizAnterior pituitary
The anterior pituitary is an endocrine gland that releases a variety of hormones in response to stimuli from the hypothalamus and other sources. ACTH, adrenocorticotropic hormone, stimulates the adrenal glands into releasing cortisol. FSH and LH both stimulate the gonads (ovaries and testes). FSH (follicle-stimulating hormone) regulates reproductive processes, sexual maturation, development, and growth. LH stimulates the ovaries and testes into producing estrogen and progesterone, and testosterone respectively. Thyroid-stimulating hormone (TSH) stimulates the thyroid gland into producing thyroxine (T4) and triiodothyronine (T3), both of which stimulate metabolism in most tissues. Prolactin is a peptide hormone that stimulates milk production from the mammary glands and can affect levels of sex hormones. The other hormones released, but not shown here, are endorphins, which are released in response to exercise, pain, and excitement and cause a feeling of analgesia (well-being). Finally, growth hormone stimulates cell reproduction, development, and growth.


 Picmonic
Picmonic