Diabetes mellitus medications
To watch this, and all of Joe-Gilboy PA-C's marvelous video lessons you must be a member. Members can login here or join now.
Know your medication - side effects and functions
- Metformin (Glumetza, Glucophage, Fortamet):
- Mechanism: Decreases hepatic glucose production and peripheral glucose utilization, decreases intestinal glucose absorption (these are reasons it leads to weight loss)
- Side effects: Can cause lactic acidosis and needs to be discontinued 24 hours before contrast and resumed 48 hours after with monitoring for creatinine, stop if creatine is > 1.5
- Sulfonylureas - Glyburide (Glynase), Glipizide (Glucotrol, Glucotrol XL), Glimepiride (Amaryl):
- Mechanism: Stimulates pancreatic beta-cell insulin release (insulin secretagogue)
- Side effects: Causes hypoglycemia and weight gain
- Thiazolidinediones - Pioglitazone (Actos) and Rosiglitazone (Avandia):
- Mechanism: Increases insulin sensitivity in peripheral receptor site adipose and muscle has no effect on pancreatic beta cells
- Side effects: Can cause fluid retention and edema. Cardiovascular toxicity with Avandia.
- α-Glucosidase inhibitors - Acarbose (Precose) and Glyset (Miglitol):
- Mechanism: Delays intestinal glucose absorption
- Side effects: May cause increased LFTs and hepatitis, diarrhea, flatulence
- Meglitinides - Repaglinide (Prandin) and Nateglinide (Starlix):
- Mechanism: Stimulates pancreatic beta-cell insulin release
- Side effects: May cause hypoglycemia
- GLP-1 Agonists - Exenatide (Trulicity, Byetta):
- Mechanism: Lowers blood sugar by mimicking incretin - causes insulin secretion and decreased glucagon and delays gastric emptying
- Side effects: May cause hypoglycemia. Caution if gastroparesis
- DDP-4 Inhibitors - Sitagliptin (Januvia):
- Mechanism: Dipeptidyl peptidase inhibition - inhibits degradation of GLP-1 so more circulating GLP-1
- Side effects: May cause pancreatitis and renal failure
- SGLT2 Inhibitor - Canagliflozin (Invokana or Sulisent):
- Mechanism: SGLT2 inhibition lowers renal glucose threshold, which results in increased urinary glucose excretion
- Side effects: hypoglycemia and urinary tract infections
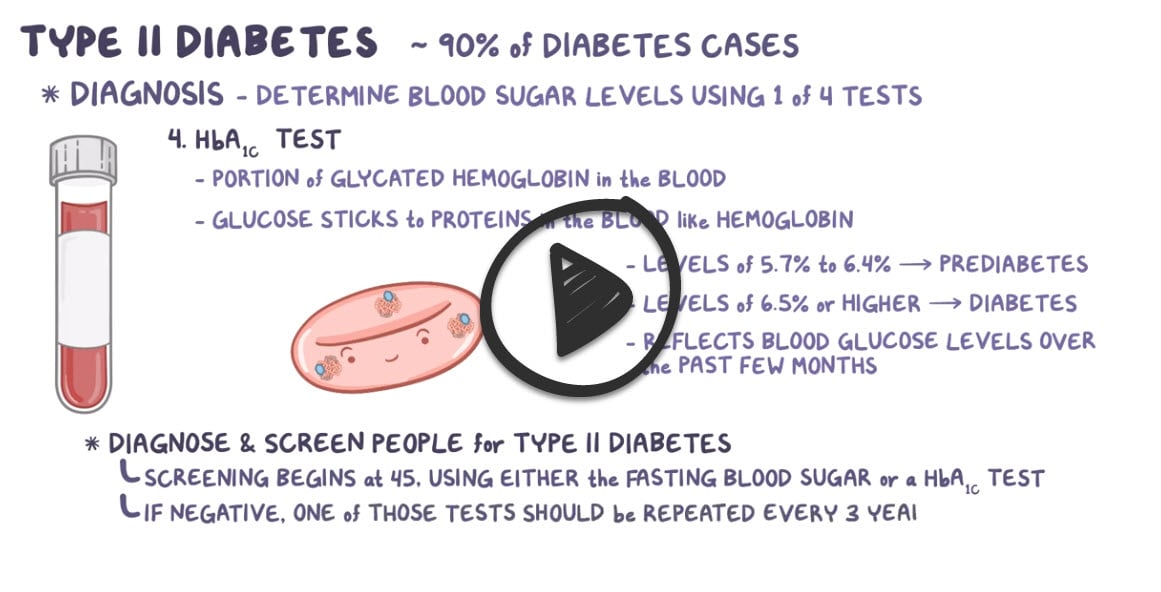
Normal fasting glucose is between 70 and 100
- A1C ≥ 6.5%
- FPG ≥ 126 mg/dL (fasting is defined as no caloric intake for at least 8 hours)
- 2-hour plasma glucose ≥ 200 mg/dL during an OGTT – glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water
- Random plasma glucose ≥ 200 mg/dL in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis
- A1C 5.7 to 6.4%
- FPG 100 to 125 mg/dL
- 2-hour post-load glucose on the 75 g OGTT 140 to 199 mg/dL
If the diagnostic test is consistent with prediabetes, it should be repeated annually
A C-peptide test is often used to help tell the difference between type 1 and type 2 diabetes
- C-peptide is a substance made in the pancreas, along with insulin. C-peptide and insulin are released from the pancreas at the same time and in about equal amounts. So a C-peptide test can show how much insulin your body is making
- With type 1 diabetes, your pancreas makes little to no insulin, and little or no C-peptide = ↓ C-peptide
- With type 2 diabetes, the body makes insulin but doesn't use it well. This can cause ↑ C-peptide
Diet and exercise with lifestyle changes are first-line - carbs 50-60% and protein 15-20%
- Studies demonstrate that just 150 minutes (2.5 hours) per week of moderate to vigorous exercise significantly reduces microvascular complications, including retinopathy, in patients with T2D
Glucose goals and management
- A1C < 7.0 % check every 3 months if not controlled or if therapy has changed/requires adjustment and 2 x per year if controlled
- Preprandial glucose 80-130 mg/dL (60-90 if pregnant)
- Peak postprandial (1 to 2 hours after the beginning of the meal) blood glucose < 180 mg/dL
- Annual dilated eye exams, ACEI if microalbuminuria, annual foot examination
Oral therapies:
| Intervention | Expected decrease in A1C with monotherapy (%) | Advantages | Disadvantages |
| Lifestyle changes to decrease weight and increase activity | 1.0 to 2.0 | Broad benefits | Insufficient for most within the first year owing to inadequate weight loss and weight regain |
| Metformin | 1.0 to 2.0 | Weight neutral | GI side effects, contraindicated with renal insufficiency (eGFR <30 mL/min) |
| Additional therapies | |||
| Insulin (usually with a single daily injection of intermediate- or long-acting insulin initially) | 1.5 to 3.5 | No dose limit, rapidly effective, improved lipid profile | One to four injections daily, monitoring, weight gain, hypoglycemia, analogues are expensive |
| Sulfonylurea (shorter-acting agents preferred) | 1.0 to 2.0 | Rapidly effective | Weight gain, hypoglycemia |
| GLP-1 agonist (daily to weekly injections) | 0.5 to 1.0 | Weight loss and reduced cardiovascular mortality (liraglutide, semaglutide) in patients with established CVD | Requires injection, frequent GI side effects, long-term safety not established, expensive |
| Thiazolidinedione | 0.5 to 1.4 | Improved lipid profile (pioglitazone), potential decrease in MI (pioglitazone) | Fluid retention, HF, weight gain, bone fractures, potential increase in MI (rosiglitazone) and bladder cancer (pioglitazone) |
| Meglitinides | 0.5 to 1.5 | Rapidly effective | Weight gain, three times/day dosing, hypoglycemia |
| SGLT2 inhibitor | 0.5 to 0.7 | Weight loss, reduction in systolic blood pressure, reduced cardiovascular mortality in patients with established | Vulvovaginal candidiasis, urinary tract infections, bone fractures, lower limb amputations, acute kidney injury, DKA, long-term safety not established |
| DPP-4 inhibitor | 0.5 to 0.8 | Weight neutral | Long-term safety not established, expensive, possible increased risk of HF with saxagliptin |
| Alpha-glucosidase inhibitor | 0.5 to 0.8 | Weight neutral | Frequent GI side effects, three times/day dosing |
| Pramlintide | 0.5 to 1.0 | Weight loss | Three injections daily, frequent GI side effects, long-term safety not established, expensive |
| Table source: UpToDate | |||
| Insulins | ||||
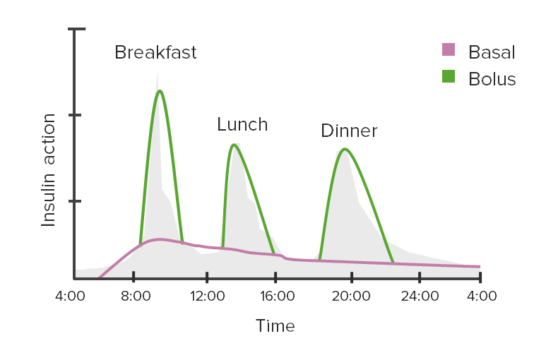
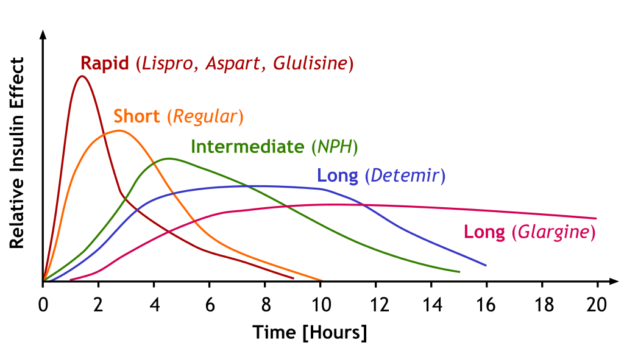 Image by A. Peters, M. Komorniczak. License: CC BY 3.0 |
||||
| Insulin effect | Type of Insulin | Onset of action | Peak of action | Duration of action |
| Fast acting | Lispro | 15–30 minutes | 1–3 hours | 4–6 hours |
| Aspart | ||||
| Glulisine | ||||
| Short-acting | Regular | 30 minutes | 1.5–3.5 hours | 8 hours |
| Intermediate-acting | NPH | 1–2 hours | 4–6 hours | > 12 hours |
| Long-acting | Detemir | 1–2 hours | 3–9 hours | 14–24 hours |
| Glargine | 3–4 hours | No peak | Approximately 24 hours | |
| Degludec | Approximately 1 hour | No peak | > 40 hours | |
Example of insulin regimen:
|
||||
Blood pressure
- JNC 8 treatment targets: Reduce BP to < 140/90 mm Hg for everyone < 60, including those with a kidney disorder or diabetes
- ADA recommends treating BP of <140 and <90 mmHg. Lower treatment targets, i.e., 130/80 mmHg, may be appropriate for individuals at high risk of CVD, if they can be achieved without undue treatment burden.
- ACC/AHA blood pressure targets - target for patients with comorbidities: < 130/80
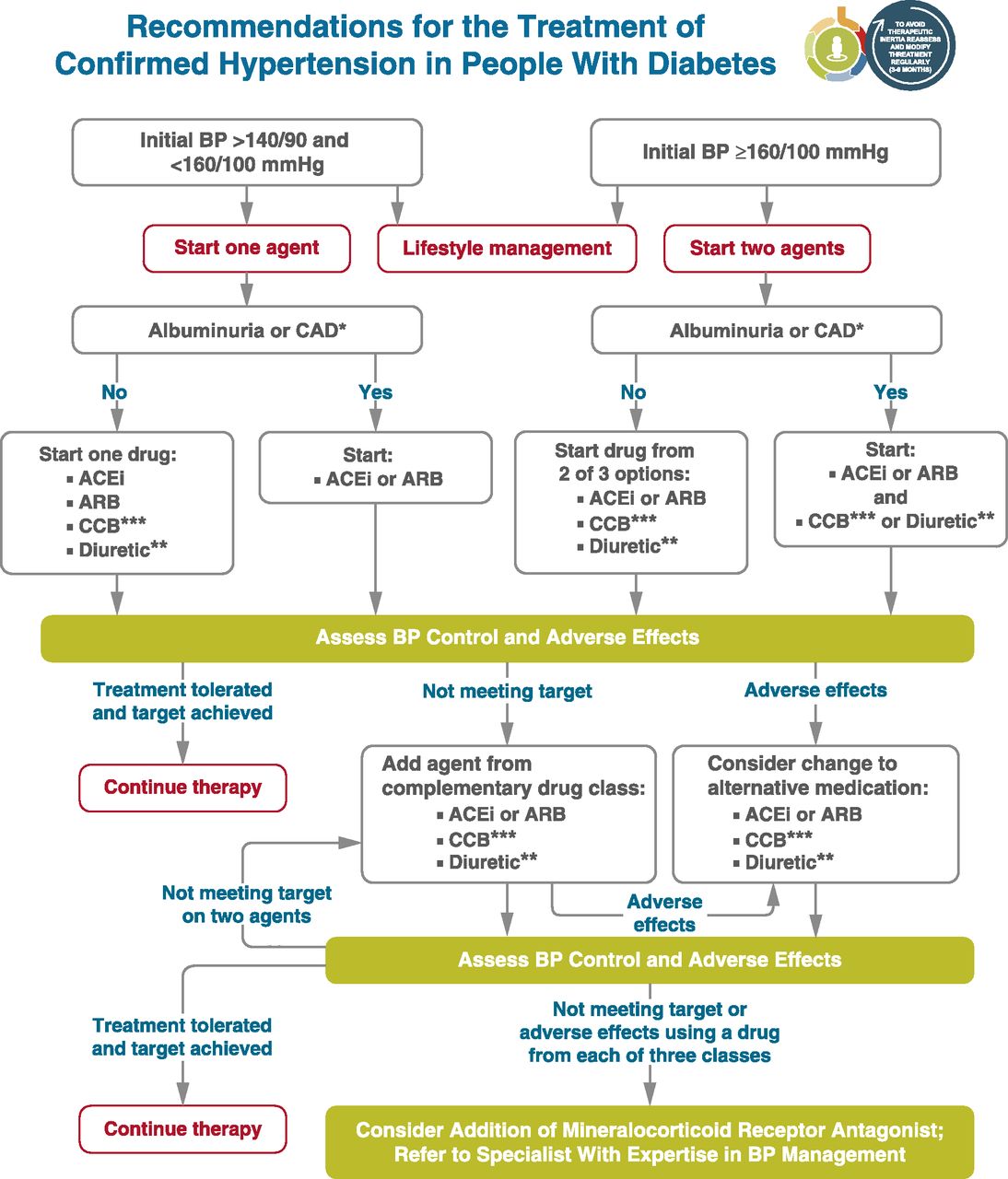 From ADA Standards - Section 10, CV Disease **Thiazide-like diuretics; long-acting agents shown to reduce cardiovascular events, such as chlorthalidone and indapamide, are preferred. ***Dihydropyridine calcium channel blocker (CCB). |
Cholesterol
- New statin guidelines recommend statins in all persons with diabetes mellitus who are 40 to 75 years of age with LDL-C levels of 70 to 189 mg per dL but without clinical ASCVD (see guidelines)
|
High, Moderate, and Low-Intensity Statin Therapy |
||
|---|---|---|
| High Intensity | Moderate Intensity | Low Intensity |
| Daily dosage lowers LDL-C by approximately ≥ 50% on average | Daily dosage lowers LDL-C by approximately 30% to 50% on average | Daily dosage lowers LDL-C by < 30% average |
| Atorvastatin (Lipitor), 40 to 80 mg | Atorvastatin, 10 (20) mg | Simvastatin, 10 mg |
| Rosuvastatin (Crestor), 20 (40) mg | Rosuvastatin, (5) 10 mg | Pravastatin, 10 to 20 mg |
| Simvastatin (Zocor), 20 to 40 mg | Lovastatin, 20 mg | |
| Pravastatin (Pravachol), 40 (80) mg | Fluvastatin, 20 to 40 mg | |
| Lovastatin (Mevacor), 40 mg | Pitavastatin, 1 mg | |
| Fluvastatin XL (Lescol XL), 80 mg | ||
| Fluvastatin, 40 mg twice daily | ||
| Pitavastatin (Livalo), 2 to 4 mg | ||
Aspirin
- Aspirin (75 to 162 mg/day) is recommended for secondary prevention in diabetic patients with a history of MI, vascular bypass, stroke or transient ischemic attack, peripheral vascular disease, claudication, or angina
- For the primary prevention of ASCVD in patients with diabetes at increased cardiovascular risk (10-year risk >10 percent), we suggest aspirin (75 to 162 mg daily)
- Prevention of ASCVD in adults with diabetes at low risk (10-year ASCVD risk <10 percent) is not routinely recommended
Vaccination
- Influenza vaccination yearly, with adults 65 years of age and older administered the high-dose vaccine
- Pneumococcal vaccination with one pneumococcal conjugate vaccine (PCV13) in adults ≥65 years and pneumococcal polysaccharide vaccine (PPSV23) once before and once after age 65. Once the patient is ≥65 years (and ≥1 year after PPSV23), give PCV13.
- Hepatitis B vaccination for unvaccinated adults younger than 60 years of age without evidence of prior infection
- Tetanus and diphtheria vaccinations, based on CDC guidelines
- Herpes zoster, recombinant vaccine, based on CDC guidelines
Monitoring in patients with diabetes mellitus (summary table)
| History and physical examination | ||
| Height, weight, and BMI | Every visit | |
| Smoking cessation counseling | Every visit | For smokers only. |
| Blood pressure | Every visit | Goal systolic pressure 125 to 130 mmHg. |
| Dilated eye examination | Annually | Begin at onset of type 2 diabetes, 3 to 5 years after onset of type 1 diabetes. Examine yearly (or more frequently) if retinopathy is present, every 2 to 3 years if there is no evidence of retinopathy. |
| Comprehensive foot examination | Annually | Every visit if peripheral vascular disease or neuropathy. |
| Dental examination | Annually | Periodontal disease is more severe but not necessarily more prevalent in patients with diabetes. |
| Laboratory studies | ||
| Lipid profile | Initially, as indicated | In people without dyslipidemia and not on cholesterol-lowering therapy, testing may be infrequent. |
| A1C | Every 3 to 6 months | Goal ≤ 7% (may be lower or higher in selected patients). |
| Urinary albumin-to-creatinine ratio | Annually | Begin 3 to 5 years after onset of type 1 diabetes and at diagnosis in patients with type 2 diabetes; protein excretion should also be monitored if persistent albuminuria is present. |
| Serum creatinine | Initially, as indicated | Typically annually; more often in the presence of chronic kidney disease. |
| Vaccinations | ||
| Pneumococcus | ||
|
1 dose, ages 19 to 64 years | Once the patient is ≥ 65 years (and ≥1 year after PCV13 and > 5 years after previous dose of PPSV23), give a second dose of PPSV23. Revaccinate every 10 years. |
|
1 dose at age ≥ 65 years | Once the patient is ≥65 years (and ≥1 year after PPSV23), give PCV13. |
|
1 dose, ages 19 to 64 years or ≥ 65 years if no prior dose. No additional pneumococcal vaccine is needed! | |
| Influenza | Annually | |
| Hepatitis B | 3-dose series | Administer to unvaccinated adults who are ages 19 to 59 years. For older patients, administer based upon risk of acquiring hepatitis B, including the need for assisted blood glucose monitoring and the likelihood of an adequate immune response to vaccination. |
| Provide other routine vaccinations for adults with diabetes according to age-related recommendations. | ||
| Education, self-management review | ||
| Annually | More often at onset of diabetes and when there is a change in regimen. | |
 Osmosis Osmosis |
|
 |
Metformin is part of the Biguanide class of diabetic drugs. It is the first-line medical treatment for diabetes mellitus type 2 and can also be used for PCOS. Its exact mechanism of action is unknown, but this medication leads to decreased gluconeogenesis and increased insulin sensitivity, subsequently equating to lower blood sugar levels. Side effects of this drug include lactic acidosis and GI distress, and Metformin should not be used in patients with renal failure.
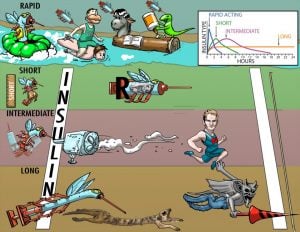
Play Video + QuizInsulins
Insulins for medical use are synthetically created analogs of the human hormone. Some are chemically altered in structure to change the rate of absorption and duration of action within the human body. When classified according to time course, insulin preparations fall into three major groups: short duration, intermediate duration, and long duration.
Glyburide and Glipizide (2nd Generation Sulfonylureas)
Glyburide and glipizide are second-generation sulfonylureas that stimulate the release of insulin from pancreatic islet cells. This action increases the amount of circulating insulin to maintain normal blood glucose levels in the body. These drugs are indicated for patients with type 2 diabetes who have the ability to produce insulin (refer to Picmonic “Insulin”). Second-generation sulfonylureas have replaced first-generation agents due to their increased potency and fewer drug-drug interactions. Hypoglycemia is a major side effect. These drugs should not be used while consuming alcohol and 2nd generation sulfonylureas (except glyburide) should not be used in pregnancy or breastfeeding.
Play Video + QuizGlucagon (GlucaGen)
Glucagon (GlucaGen) is a polypeptide hormone that causes the hepatic conversion of stored glycogen into readily-available glucose. This medication is indicated for hypoglycemia caused by insulin overdose and not related to starvation. It is given when IV glucose is not available. Side effects may include nausea and vomiting. This drug must be reconstituted with a powder supplied by the manufacturer. Once conscious, the patient should be given oral carbohydrates within an hour to avoid rebound hypoglycemia. If the patient shows no improvement, IV 50% glucose may be given for immediate results.
Play Video + QuizExenatide (Byetta)
Exenatide (Byetta) is an injectable hypoglycemic drug indicated for patients with Type 2 diabetes. The medication functions as an incretin mimetic and GLP-1 synthetic analog. Side effects include hypoglycemia, nausea, vomiting, diarrhea, pancreatitis, and renal failure. Since exenatide delays gastric emptying, it should be administered at least 1 hour after giving other medications. Exenatide is considered adjunct therapy and administered with other antidiabetic drugs.
Play Video + QuizChlorpropamide and Tolbutamide (Orinase) (1st Generation Sulfonylureas)
Chlorpropamide and tolbutamide are first-generation sulfonylureas that promote insulin release. This action increases the amount of circulating insulin to maintain normal blood glucose levels in the body. These drugs are indicated for patients with type 2 diabetes who have the ability to produce insulin (refer to Picmonic “Insulin”). However, first-generation sulfonylureas are rarely used due to their lower potency and significant drug-drug interactions. Side effects of these medications include hypoglycemia and cardiovascular toxicity. These drugs should not be used while pregnant, breastfeeding, consuming alcohol, or taking beta-blockers.
Play Video + QuizAcarbose (Precose) and miglitol (Glyset)
Acarbose (Precose) and miglitol (Glyset) are alpha-glucosidase inhibitors used to help control blood glucose levels in diabetic patients. By inhibiting an intestinal enzyme that converts complex carbohydrates into digestible forms, these medications decrease the rate of carbohydrate digestion and absorption. This action decreases the rise of glucose levels caused by eating. These medications are indicated for patients with type 2 diabetes. Side effects include flatulence, cramps, diarrhea, and anemia. Since these drugs may cause liver damage, liver function tests should be monitored frequently. In the event of hypoglycemia, glucose (not sucrose) should be administered.
Play Video + QuizPioglitazone (Thiazolidinediones)
Pioglitazone stimulates receptors in the body to increase cellular response to insulin, thus decreasing insulin resistance. This medication is only effective in the presence of insulin and can only be used in patients with type II diabetes. Side effects of pioglitazone include upper respiratory infection, muscle pain, sinusitis, headache, and heart failure. Patients taking pioglitazone are at increased risk for bladder cancer, and women taking this medication are more prone to bone fractures. Liver enzymes should be routinely monitored while taking pioglitazone due to the risk of liver toxicity.
Play Video + QuizPramlintide (Symlin)
Pramlintide (Symlin) is an injectable hypoglycemic drug indicated for type 1 and 2 diabetes. As a synthetic amylin analog, pramlintide is used to supplement mealtime insulin in diabetic patients unable to maintain glucose control despite insulin therapy. Side effects of pramlintide include nausea and reactions at the injection site. While administering the medication, monitor the patient for symptoms of hypoglycemia. Since it delays the absorption of other medications, avoid giving pramlintide concurrently with other drugs.
Play Video + QuizRepaglinide (Prandin) and nateglinide (Starlix)
Repaglinide (Prandin) and nateglinide (Starlix) are oral hypoglycemic medications classified as meglitinides or “glinides.” By stimulating the pancreatic cells to release more insulin, these medications decrease blood glucose levels. A major side effect of meglitinides is hypoglycemia. Since these drugs have a short half-life, instruct the patient to eat within 30 minutes of administration. Gemfibrozil (Lopid) decreases the metabolism rate of meglitinides and should not be administered to prevent drug accumulation leading to hypoglycemia.
Play Video + QuizSitagliptin (Januvia) and Saxagliptin (Onglyza) (DPP-4 Inhibitors)
Sitagliptin (Januvia) and Saxagliptin (Onglyza) are antidiabetic medications that work by blocking the DPP-4 enzyme, allowing for increased action of incretin hormones and increased release of insulin. These medications are only effective in the presence of insulin and can only be used in patients with type II diabetes. Keep in mind, however, DPP-4 inhibitors are considered third-line medications for the treatment of diabetes and should only be used if first and second-line medications have failed to provide adequate blood glucose control. Side effects include upper respiratory infection, pancreatitis, and hypersensitivity reactions.
Play Video + QuizQuestion 1 |
acarbose Hint: α-Glucosidase inhibitors, such as acarbose (Precose), reduce glucose by delaying carbohydrate absorption | |
glipizide Hint: Glipizide (Glucotrol) and other sulfonylureas work by increased insulin secretion from pancreatic β cells. | |
metformin Hint: Metformin (Glucophage), a biguanide, lowers glucose by decreasing hepatic glucose production and increasing glucose utilization. | |
Pioglitazone |
Question 2 |
glucagon Hint: Glucagon would further increase the blood glucose | |
insulin Hint: Insulin is typically not needed unless the glucose is resistant to fluids | |
bicarbonate Hint: Bicarbonate should not be administered because the blood pH is above 7.0 | |
saline |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture