Patient will present as → a 45-year-old female who comes to your clinic with complaints of a gradually enlarging lump in her neck over the past six months. She mentions occasional difficulty swallowing and a hoarse voice that comes and goes. She also reports feeling more fatigued than usual and sometimes feeling unusually warm. Medical history is significant for her mother, having undergone thyroid surgery in her 50s, though the exact details are unknown. On examination, a firm, non-tender nodule is palpated on the right lobe of the thyroid gland. The patient's reflexes are brisk. An ultrasound of the thyroid reveals a 3 cm hypoechoic thyroid nodule with calcifications, and a thyroid uptake scan shows decreased iodine uptake of the nodule compared to surrounding tissues.
The most common risk factor for thyroid carcinoma is radiation exposure
- Most common in young females 40-60 years old
- You may (not always) feel a palpable thyroid nodule/mass
There are 4 general types of thyroid cancer:
- Papillary carcinoma (80%) is the most common. Remember: PAPILLARY IS POPULAR
- Follicular: (10%) is more common among older patients and in regions of iodine deficiency. It is more malignant than papillary carcinoma, spreading hematogenously with distant metastases
- Medullary: (4%) may be sporadic (usually unilateral); often familial
- Anaplastic: (1%) No effective therapy exists, and the disease is generally fatal. About 80% of patients die within 1 year of diagnosis
Except for anaplastic and metastatic medullary carcinoma, most thyroid cancers are not highly malignant and are seldom fatal
- Most thyroid cancers manifest as asymptomatic nodules. Rarely, lymph node, lung, or bone metastases cause the presenting symptoms of small thyroid cancers
Solitary thyroid nodule:
- A solitary thyroid nodule is common in the general population and affects women more often than men. One in 12 young women has a thyroid nodule
- Nodules must generally be over 1 cm in diameter to be palpated. Most are asymptomatic and are discovered incidentally via physical exam or through imaging. The presence of one palpable nodule increases the risk of additional nodules
- Thyroid adenoma is the most common benign nodule. Only 5% of palpable nodules are malignant
Thyroid cancer risk factors:
- Prior radiation (head or neck)
- Family history of thyroid cancer
- Being > 65 y/o or < 20 y/o
- Having additional symptoms such as voice changes, hoarse voice, difficulty breathing, or difficulty swallowing indicates invasion of adjacent tissues
Physical exam risk factors
- Firm and hard on palpation
- Fixed during swallowing
- Swollen lymph node in the neck region and only on one side
Lab and ultrasound finding risk factors
- Nonfunctional nodules – normal or high TSH and normal thyroid hormone level
- Solid and echogenic, irregular margins, microcalcifications, > 1 cm
If you think you have a mass, you will need to confirm by ultrasound
- Lesions larger than 1 cm should be biopsied
- Smaller lesions and those with benign histology can be followed and reevaluated if they grow
Ultrasound characteristics that put a nodule at high risk of malignancy are:
- Microcalcifications, hypoechogenicity, a solid nodule, irregular nodule margins, chaotic intranodular vasculature, and a nodule that is more tall than wide.
You must identify if the mass is benign or malignant. To do this, you can order a thyroid uptake scan
- A cancerous lesion does not make hormones and will not take up iodine from a radioactive thyroid scan. (COLD NODULE)
- A non-cancerous lesion does make hormones and will take up iodine at either a normal rate or a quicker rate. (HOT NODULE)
Remember: COLD = CANCER
Once you see a cold nodule, you must rule out cancer. To do this, you will need a FINE NEEDLE ASPIRATION
Treatment depends on the type of cancer, and prognosis depends on staging, with a 99% 5-year survival with locally confined, less than 1 cm papillary carcinoma
- Always involves complete or partial removal of the thyroid with chemotherapy and external beam radiation reserved for anaplastic thyroid cancer
Evaluation of a thyroid nodule
Suggested diagnostic and treatment approach for thyroid nodules (AAFP) Click Here
Confirm by Ultrasound
Microcalcifications, hypoechogenicity, a solid nodule, irregular nodule margins, chaotic intranodular vasculature, and a nodule that is more tall than wide.
Review TSH
Is the TSH normal, subnormal, or elevated?
TSH normal or elevated
Meets sonographic criteria for FNA?
Fine needle aspiration
Proceed to FNA If nodule is nonfunctional on uptake scan and meets sonographic criteria for FNA
Monitor
If nodule is nonfunctional on uptake scan and does not meet sonographic criteria for FNA
Thyroid nodules that do not meet sonographic criteria for FNA should be monitored with periodic ultrasonography. The frequency of evaluation (ranging from 6 to 24 months) depends upon the sonographic features of the nodules.
TSH subnormal/low
Proceed to radionuclide thyroid uptake scan
Thyroid uptake scan
Also measure FT4, T3
A cancerous lesion does not make hormone and will not take up iodine from a radioactive thyroid scan. (COLD NODULE)
A non-cancerous lesion does make hormone and will take up iodine at either a normal rate or a quicker rate. (HOT NODULE)
Fine needle aspiration
If nodule is nonfunctional on uptake scan and meets sonographic criteria for FNA
Thyroid nodules that do not meet sonographic criteria for FNA should be monitored with periodic ultrasonography. The frequency of evaluation (ranging from 6 to 24 months) depends upon the sonographic features of the nodules.
FT4 and FT3
FT4 and T3 Normal = subclinical hyperthyroidism ⇒ can be observed in most cases
FT4 and/or T3 high = overt hyperthyroidism ⇒ treat
 Osmosis Osmosis |
|
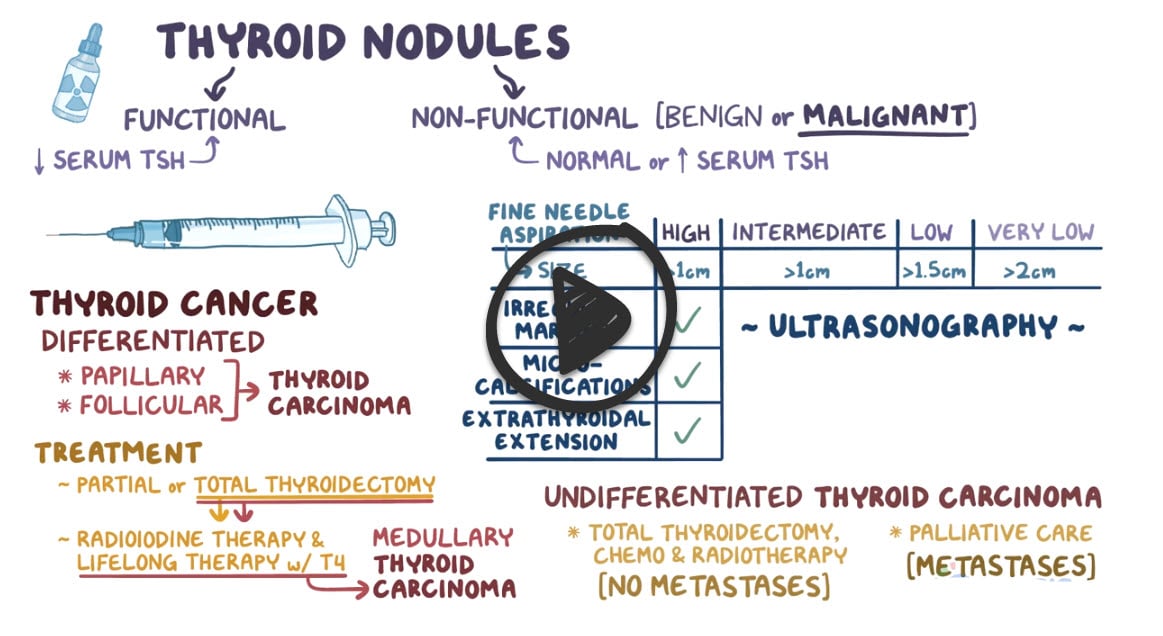 |
Thyroid nodules can be identified on physical exam or incidentally on imaging for another indication. There are various etiologies for thyroid nodules, some benign and some malignant, so it is important to investigate further when they are discovered. Initial work-up includes a serum thyroid-stimulating hormone (TSH) and an ultrasound of the thyroid gland. Depending on the findings, further testing may include fine-needle aspiration (FNA), radioactive iodine uptake (RAIU), and serum triiodothyronine (T3) and thyroxine (T4). Routine monitoring of a thyroid nodule is recommended with ultrasound 6-18 months after diagnosis.
Play Video + QuizThyroid cancer
There are four main types of thyroid cancer, listed in descending order of prevalence are papillary, follicular, medullary, and anaplastic.
1. Papillary Carcinoma
Papillary thyroid carcinoma is the most common, carries the best prognosis, is characterized by lymphatic spread and distinct histological findings like Orphan Annie nuclei and psammoma bodies. Risk factors for papillary carcinoma include head and neck radiation, RET and BRAF gene mutations, as well as Gardner and Cowden’s syndrome.
2. Medullary Carcinoma
Medullary Carcinoma Picmonic, the third most common type of thyroid cancer is divided into sporadic and familial types. This cancer arises from parafollicular C cells, may produce calcitonin and manifest with hypocalcemia or produce ACTH and manifest with Cushing syndrome. It is characterized histologically by amyloid-staining sheets of cells and will exhibit calcitonin release with pentagastrin administration. Two major risk factors for medullary carcinoma are a history of head and neck radiation and a family history of MEN 2A and 2B.
Play Video + Quiz3. Follicular Carcinoma
Follicular thyroid carcinoma, the second most common type, commonly presents as a solitary thyroid nodule with a good prognosis. It is characterized by hematogenous spread, thyroid capsule invasion, and histological findings like uniform follicles. A major risk factor for follicular carcinoma is a history of head and neck radiation, and women are more commonly affected than men.
Play Video + Quiz5. Anaplastic Thyroid Cancer
Anaplastic Thyroid Cancer is the least common, is rapidly progressive, and has a grave prognosis. A common presenting symptom of this tumor is a hoarse voice and diagnostic examination will show the invasion of local structures and a mixed cellular morphology. Major risk factors for anaplastic carcinoma are old age, the presence of multinodular goiter, and a history of previous thyroid disease or malignancy.
Play Video + QuizQuestion 1 |
magnetic resonance imaging (MRI) scan of the thyroid | |
thyroid ultrasound study | |
radioactive iodine uptake scan | |
FNA of the nodule | |
computed tomography (CT) scan of the thyroid |
Question 2 |
serum T4 | |
radioactive iodine uptake thyroid scan | |
FNA of the nodules | |
thyroid ultrasound study | |
CT scan of the thyroid |
Question 3 |
cold nodules are more likely than hot nodules to be benign | |
cold nodules need not be investigated any further | |
cold nodules are more likely than hot nodules to be associated with signs and symptoms of hyperthyroidism | |
cold nodules always require further investigation to differentiate benign from malignant status | |
all nodules, whether hot or cold, require further investigation to differentiate benign from malignant status |
|
List |