GI and Nutrition Content Blueprint Classic and Pathognomonic Patient Presentations and Question Stems For the PANCE and PANRE Board Exam
Below is a list of the most common PANCE and PANRE board review question stems and patient presentations you are likely encounter on your board exam

- These represent the most common/classic patient presentations or what could be considered pathognomonic
- This is a comprehensive list following the exact NCCPA PANCE and PANRE GI and Nutrition content blueprint
- The pulmonology section represents 12% of your board exam
- Make sure to download my FREE content blueprint checklist
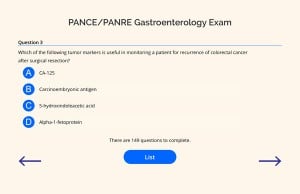
- Members have access to the comprehensive 142 question gastroenterology exam
GI Content Blueprint Case Presentation Flashcards |
|
| Esophagitis | Patient will present with → odynophagia (painful swallowing), dysphagia and retrosternal chest pain |
| Motility disorders | Achalasia - Patient will present with → dysphagia to both liquids and solids, bid/parrot beak on barium swallow
Diffuse esophageal spasms - Patient will present with → dysphagia to solids and liquids with stabbing chest pain worse with hot or cold liquids or food and a corkscrew appearance on barium swallow Neurogenic dysphagia - Patient will present with → patient with myasthenia gravis, ALS or a stroke with dysphagia to solids and liquids with aspiration into the windpipe or regurgitation into the nose Zenker diverticulum - Patient will present with → dysphagia to food and liquid with regurgitation of undigested food several hours after eating along with foul odor of breath Scleroderma - Patient will present with → history of scleroderma and dysphagia to both solids and liquids Esophageal stenosis or stricture - Patient will present with → dysphagia to solids in a patient with a history of GERD |
| Mallory-Weiss tear | Patient will present with → an episode of hematemesis, vomiting, and retching after alcohol intake |
| Esophageal neoplasms | Patient will present with → progressive dysphagia to solid foods along with weight loss, chest pain, hoarseness reflux and hematemesis |
| Strictures | Patient will present with → an intermittent, non-progressive dysphagia for solid foods that occurs while consuming a heavy meal with meat that was “wolfed down,” hence the pseudonym the “steakhouse syndrome.” |
| Varices | Patient will present with → history of cirrhosis along with hematemesis, melena, hematochezia +/- signs of hypovolemia |
| Gastroesophageal reflux disease | Patient will present with → heartburn, generally worse after meals and when lying down and often relieved with antacids. Regurgitation and dysphagia may occur. |
| Gastritis | Patient will present with → dyspepsia and abdominal pain in a patient with predisposing factors (i.e NSAID use) |
| Stomach Neoplasms | Patient will present with → weight loss, early satiety, abdominal pain/fullness and dyspepsia |
| Peptic ulcer disease | Gastric ulcer - Patient will present with → abdominal discomfort that is worse with meals and gets better an hour or so later after eating.
Duodenal ulcer - Patient will present with → abdominal discomfort that improves with meals and gets worse an hour or so later after eating. |
| Pyloric stenosis | Patient will present with → projectile vomiting occurs shortly after feeding in an infant < 3 mo old, palpable “olive-like” mass at the lateral edge right upper quadrant |
| Acute/chronic cholecystitis | Patient will present with → colicky epigastric or right upper quadrant pain in a forty-year-old obese patient that becomes steady and increases in intensity. It often occurs after a high fat meal |
| Cholangitis | Case 1: Patient will present with → fever + jaundice + right upper abdominal pain (Charcot's triad)
Case 2: Patient will present as → a 32-year-old female with a history significant for ulcerative colitis who has been stable and free of problems for over 7 years. She describes worsening symptoms of fatigue, pruritus, anorexia, and indigestion over the past 6 months. Her husband reports that her skin and eyes appear yellow although she adamantly denies alcohol consumption. Labs reveal an elevated alkaline phosphatase, mild elevations in AST and ALT. ERCP fails to show common bile duct obstruction |
| Cholelithiasis | Patient will present with → right upper quadrant pain “biliary colic” begins abruptly, continues in duration, resolves slowly lasting 20 min – hours associated with nausea precipitated by fatty foods and large meals. |
| Acute/chronic hepatitis | Patient will present with → nausea, vomiting, anorexia, aversion to her usual one pack a day tobacco habit, and right upper quadrant abdominal pain. She has been sick for the past 3 days. She does complain of passing dark-colored urine for the past 2 days. She has just returned from a 2-week trip to Mexico. She has had no exposure to blood products, has no history of intravenous drug use, and has no significant risk factors for sexually transmitted disease. On examination, she looks acutely ill. Her pulse is 100 beats/minute, blood pressure 110/70 mm Hg, respirations 18, and temperature 101°F. Her sclerae are icteric, and her liver edge is tender |
| Cirrhosis | Patient will present with → (eg, anorexia, fatigue, weight loss). Late manifestations include portal hypertension, ascites, and, when decompensation occurs, liver failure |
| Liver neoplasms | Patient will present as → previously stable patient with cirrhosis now presents with abdominal pain, weight loss, right upper quadrant mass, and unexplained deterioration |
| Acute/chronic pancreatitis | Patient will present with → severe epigastric pain radiating to the back. The pain typically lessens when the patient leans forward or lies in the fetal position |
| Pancreatic neoplasms | Patient will present with → fatigue and weight loss. The patient describes vague diffuse epigastric pain for 2 months, which started after a couple of weeks of mild diarrhea. He has a 15-lb unintentional weight loss and no appetite. He is not interested in his usual activities. Social history is positive for heavy tobacco and alcohol use. On physical exam, you note "dark urine", painless jaundice and scleral icterus |
| Appendicitis | Patient will present with → right lower quadrant direct and rebound tenderness located at McBurney's point (junction of the middle and outer thirds of the line joining the umbilicus to the anterior superior spine) |
| Celiac disease | Patient will present with → diarrhea, steatorrhea, flatulence, weight loss, weakness and abdominal distension are common. Infants and children may present with failure to thrive |
| Constipation | Patient will present with → bloating, abdominal pain, straining and pain with bowel movements. History of less than 2 bowel movements per week (this is the definition of constipation) |
| Diverticular disease | Diverticulitis will present with → sudden-onset abdominal pain, usually in the left lower quadrant, with or without fever (generally patients don't have rectal bleeding)
Diverticulosis will present with → painless rectal bleeding, particularly in an elderly patient. |
| Inflammatory bowel disease | Ulcerative colitis will present with → bloody puss filled diarrhea, rectal/lower quadrant pain, fever, and urgency
Crohn's disease will present with → abdominal pain, weight loss, diarrhea and oral mucosa aphthous ulcers. Longer standing disease may have severe anemia, polyarthralgia, and fatigue.
|
| Intussusception | Patient will present as → a child with sudden onset of significant, colicky abdominal pain that recurs every 15 to 20 min, often with vomiting. Stool if passed will contain mucus and blood (currant jelly stools). A sausage like mass may be felt on abdominal examination. |
| Irritable bowel syndrome | Patient will present with → frequent bouts of constipation alternating with diarrhea. She frequently experiences abdominal discomfort, which is relieved with bowel movements |
| Ischemic bowel disease | Acute mesenteric ischemia will present with → sudden onset abdominal pain occurring 10 -30 minutes after eating in a patient with a HISTORY OF ATRIAL FIBRILLATION or CHF. It is associated with bleeding per rectum with or without diarrhea. Physical examination findings is usually disproportionate with abdominal pain. It occurs in the elderly and those that are at risk of emboli formation. |
| Lactose intolerance | Patient will present with → abdominal pain, bloating, flatulence, and diarrhea after ingestion of dairy products |
| Colon Cancer | Patient will present with → painless rectal bleeding and a change in bowel habits in a patient 50-80 years of age |
| Small Bowel obstruction | Patient will present with → Abdominal distention and high-pitched, hyperactive bowel sounds, vomiting of partially digested food and loss of bowel movements |
| Polyps | Patient will present with → rectal bleeding, cramps and abdominal pain. Obstruction may occur with a large lesion |
| Toxic megacolon | Patient will present with → history of ulcerative colitis, developed abdominal pain, vomiting, diarrhea, passage of blood and mucus per rectum and fever, markedly distended abdomen with peritonitis and shock. KUB shows markedly dilated colon > 6 cm |
| Anal fissure | Patient will present with → rectal pain and bleeding which occurs with or shortly after defecation, lasts for several hours, and subsides until the next bowel movement. |
| Abscess/fistula | Patient will present with → painful; perianal swelling, redness, and tenderness |
| Fecal impaction | Patient will present with → abdominal pain, belly cramping and bloating, stool leakage, rectal discomfort in an elderly bed-bound patient with impaired mental function and poor fluid/fiber intake |
| Hemorrhoids | Patient with internal hemorrhoids will present with → bright red blood per rectum, pruritus and rectal discomfort
Patients with external hemorrhoids will present with → significant pain, but no bleeding |
| Anorectal cancer | Patient will present with → rectal bleeding with defecation + tenesmus (a feeling of incomplete emptying after a bowel movement)
Bleeding with defecation is the most common initial symptom. Some patients have pain, tenesmus, or a sensation of incomplete evacuation. A mass may be palpable on digital rectal examination. |
| Hernia | Patient will present with → a painless bulge in the inguinal area |
| Infectious and Noninfectious Diarrhea | Patient will present with → three or more liquid or semisolid stools daily for at least 2-3 consecutive days |
| Vitamin and Nutritional Deficiencies | Patient will present with → 4-year-old with severe malnutrition and developmental delay |
| Metabolic Disorders | Patients with undiagnosed phenylketonuria will present with → failure to to attain early developmental milestones, microcephaly, and progressive impairment of cerebral function. Patients may present with seizures, hypopigmentation, and a "musty odor" of sweat and urine. |
| GI and Nutrition Exam | |