60-year-old with a distended abdomen
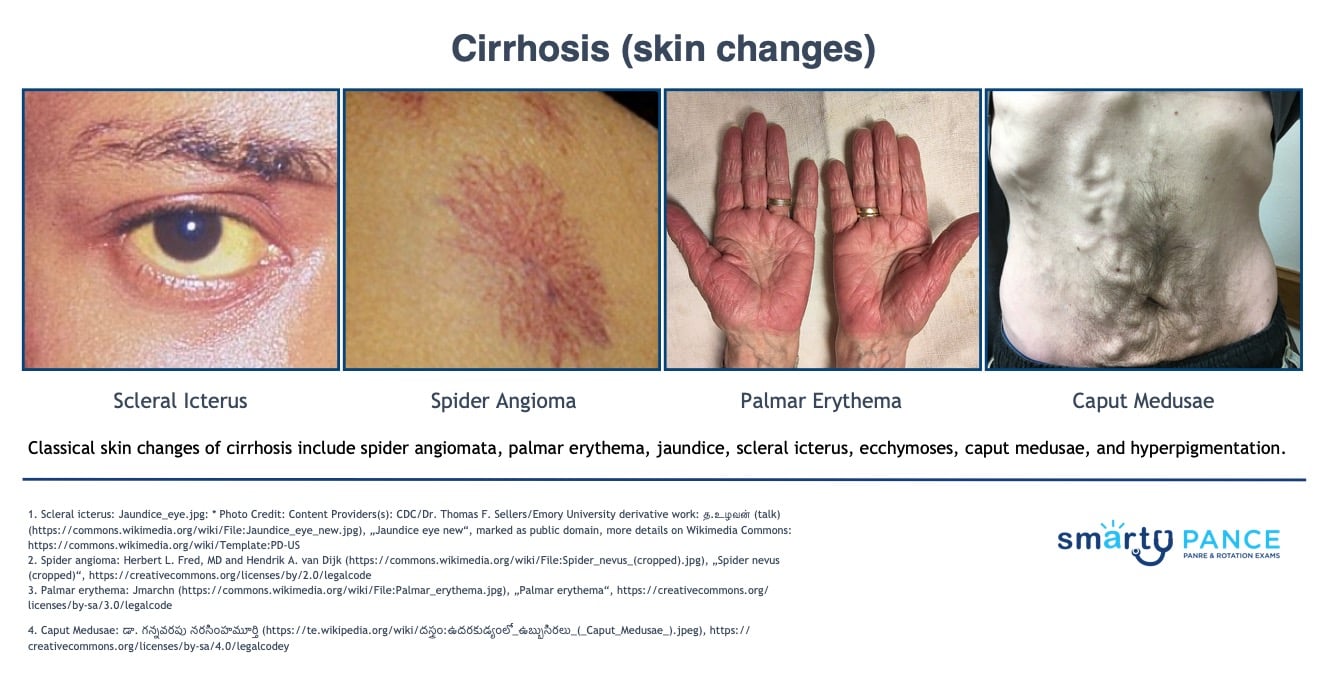
Patient will present as → a 63-year-old white male with a chief complaint of blood in his stool. He is accompanied by his wife, who also reports weight gain, abdominal distension, and swelling of his legs. Physical exam reveals a healthy-appearing male with 3+ bilateral lower extremity edema and distended abdomen with evidence of shifting dullness. You also note several skin changes seen here. The patient is hemoccult positive and has blood on his urine dipstick. He denies tobacco and illicit drug use but admits to drinking 1-2 times per week and has about 6 beers on each occasion.
Cirrhosis is a late stage of hepatic fibrosis that has resulted in a widespread distortion of normal hepatic architecture
- Characterized by regenerative nodules surrounded by dense fibrotic tissue
- The liver is unable to regenerate due to large amounts of scar tissue
Cirrhosis is a leading cause of death worldwide and is the ninth leading cause of death among U.S. adults
The most common cause of cirrhosis is chronic alcohol abuse, but other causes include viral hepatitis B and C, non-alcoholic fatty liver disease, autoimmune hepatitis, and inherited metabolic disorders.
- Alcohol liver disease (25%): history of alcohol abuse
- Chronic Hepatitis C (21-25%): ELISA assay for anti-HCV with PCR for HCV RNA if a confirmatory test is necessary
- Hepatitis C with alcoholic liver disease (15%)
- Hepatitis B + hepatitis D infection (15%): HBsAg and HBeAg and, in some cases, HBV DNA by hybridization or bDNA assay
- Nonalcoholic steatohepatitis/obesity (~10%): History of diabetes mellitus or metabolic syndrome. Diagnosis may be suspected by abnormal liver biochemical tests and hepatic imaging showing fatty infiltration and is confirmed by liver biopsy
- Wilson's disease: ↑ Copper, ↓ Ceruloplasmin + family history
Physical exam may be normal until end-stage disease:
- Hepatomegaly (small, fibrotic liver in end-stage disease)
- Terry’s nails (white nail beds)
- Splenomegaly (if portal hypertension)
- Central obesity
- Abdominal fluid wave, shifting dullness (ascites)
- Gynecomastia
- Esophageal varices
- Pulmonary edema/effusion
Classical skin changes: spider angiomata, palmar erythema, jaundice, scleral icterus, ecchymoses, caput medusae, hyperpigmentation
Hepatic encephalopathy:
- Asterixis (flapping tremor), dysarthria, delirium, coma
Progressive cirrhosis
- Elevated ammonia level; BUN, sodium, and potassium
- α-fetoprotein level at diagnosis to screen for hepatocellular carcinoma (HCC)
- Abdominal ultrasound every 6 months to screen for hepatocellular carcinoma
- All patients with cirrhosis should undergo esophagogastroduodenoscopy (EGD) to exclude esophageal varices
- MRI is the best follow-up test for HCC if α-fetoprotein elevated and/or liver mass found on ultrasound
- Noninvasive modalities, such as elastography, are being researched as an alternative to liver biopsy
- Update necessary immunizations and focus on the treatment of the underlying cause of cirrhosis (hepatitis C, alcohol abuse, etc.)
- Fever and abdominal pain in a patient with cirrhosis think spontaneous bacterial peritonitis
- Hepatocellular carcinoma: Monitor AFP
- Budd Chiari (hepatic vein thrombosis) triad of abdominal pain, ascites, and hepatomegaly
Labs: typically, AST > ALT, ↑ the risk for hepatocellular carcinoma: monitor AFP
- AST/ALT: mildly elevated ⇒ Typically AST > ALT. Enzymes normalize as cirrhosis progresses
- ↑ ALP and ↑ GGT
- Anemia from hemolysis, folate deficiency, and splenomegaly
- Decreased platelet count from portal hypertension with splenomegaly
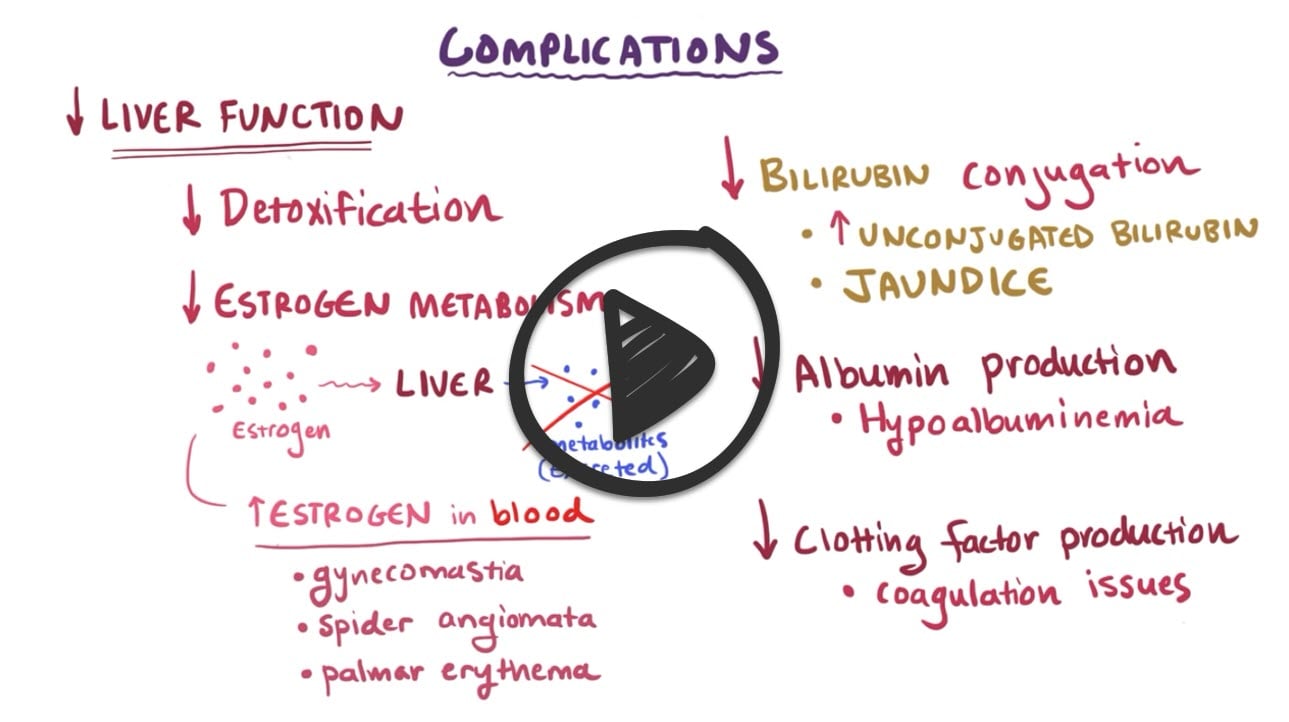
- Decreased bilirubin conjugation by the liver ⇒ ↑ unconjugated bilirubin ⇒ jaundice
- Decreased albumin production by the liver ⇒ Hypoalbuminemia
- Decreased clotting factor production by the liver ⇒ Prolonged prothrombin (PT), international normalized ratio (INR), partial thromboplastin time (PTT). Vitamin K–dependent clotting factors
- Ultrasound: helpful to determine the liver size and evaluate for hepatocellular carcinoma
- Current guidelines recommend performing an abdominal ultrasound every 6 months in patients with cirrhosis to allow for early detection and treatment of HCC. AFP testing can be added to US screening - however, the trade-off is an increase in false positives when using AFP with ultrasound compared to ultrasound alone
- Liver biopsy is invasive and is subject to sampling error, but it remains the gold standard for the diagnosis of cirrhosis
- All patients with cirrhosis should undergo esophagogastroduodenoscopy (EGD) ⇒ Exclude esophageal varices
Child-Pugh Score for Cirrhosis Mortality
- Class A (5–6 points): one-year survival 100%, two-year survival 85%
- Class B (7–9 points): one-year survival 81%, two-year survival 57%
- Class C (10–15 points): one-year survival 45%, two-year survival 35%
Generally, scarring from cirrhosis is irreversible ⇒ Prevent further damage by identifying and treating the underlying cause
- Stop alcohol
- Antiviral treatment for Hepatitis C
- Corticosteroids for autoimmune hepatitis
- Chelation therapy (e.g., penicillamine) for Wilson's disease
- Diuretics, antibiotics, laxatives, enemas, thiamine, steroids, acetylcysteine, pentoxifylline for decompensation
- Nonselective beta-blockers (nadolol and propranolol) for primary prophylaxis against variceal hemorrhage or esophageal variceal ligation (EVL)
- For advanced cirrhosis ⇒ liver transplant may be necessary
- Encephalopathy ⇒ lactulose + neomycin
- Ascites ⇒ sodium restriction, paracentesis
- Pruritus: ⇒ cholestyramine
Spontaneous bacterial peritonitis is suspected in cases of unexplained fever and abdominal pain
 Osmosis Osmosis |
|
 |
Cirrhosis is a chronic liver disease that evolves slowly, has a prolonged course, and occurs as a result of excessive alcohol intake, nonalcoholic fatty liver disease (NFLD), or chronic hepatitis C. As a result of these disorders, cirrhosis stems from degeneration and destruction of liver cells.
Play Video + QuizComplications of cirrhosis
Patients with cirrhosis are at risk of developing several major complications, such as portal hypertension. This can lead to ascites and esophageal varices. Other complications include decreased liver function, which manifests as coagulation defects. Encephalopathy can occur from ammonia buildup, and hepatorenal syndrome, leading to renal failure
Cirrhosis Interventions
Care of the patient with cirrhosis involves relieving the discomfort from ascites, excess fluid volume, skin changes, nutritional deficiencies, and preventing complications associated with hematologic problems, esophageal and gastric varices, and hepatic encephalopathy. Patients should avoid alcohol, NSAIDs, and other medications that impair liver function.
Play Video + QuizQuestion 1 |
Administer intravenous fluids Hint: While hydration is important in any sick patient, it does not specifically address the primary problem in this case, which is hepatic encephalopathy. | |
Administer lactulose orally or via rectal enema | |
Begin a protein-restricted diet Hint: Protein restriction was previously recommended for HE but is no longer advised because malnutrition can exacerbate HE. Adequate protein intake is necessary for liver regeneration and to prevent muscle wasting. | |
Administer haloperidol for his irritability Hint: Although haloperidol might calm the patient, it won't treat the underlying cause of his symptoms, which is the accumulation of toxic substances, like ammonia, in the brain due to liver disease. Moreover, haloperidol is metabolized in the liver and may potentially worsen encephalopathy. | |
Prescribe a benzodiazepine for sleep regulation Hint: Benzodiazepines are contraindicated in patients with hepatic encephalopathy because they are metabolized by the liver and can exacerbate the condition. They also increase the risk of respiratory depression in these patients. |
Question 2 |
sodium restriction | |
water restriction | |
spironolactone | |
furosemide | |
a, c, and d |
Question 3 |
Jaundice | |
Hepatic encephalopathy | |
Ascites | |
Constipation |
Question 4 |
Liver abscess Hint: Patient with liver abscess will have same symptoms and fever. Alcohol ingestion is not a risk factor for abscess. | |
Hepatic encephalopathy Hint: Hepatic encephalopathy is a complication of cirrhosis. Patient would have presented with altered sleep pattern, mental confusion, drowsiness. | |
Liver cirrhosis | |
Acute viral hepatitis Hint: Patient with acute viral hepatitis may present with the same symptoms and hepatomegaly, but not ascites, gynecomastia, spider angioma, distended abdominal veins. |
Question 5 |
cessation of alcohol use | |
beta blockers | |
maintenance of proper nutrition | |
liver transplantation | |
all of the above |
Question 6 |
Alcoholic liver disease Hint: is a common cause of liver cirrhosis in the United States (21%). | |
Chronic hepatitis C infection Hint: is a common cause of liver cirrhosis in the United States (26%). | |
Wilson’s disease | |
Nonalcoholic fatty liver disease Hint: is a common cause of liver cirrhosis in the United States (18%). |
Question 7 |
caput medusae | |
spider angiomata Hint: Spider angioma is an abnormal collection of blood vessels near the surface of the skin. | |
palmar erythema Hint: Palmar erythema is a reddening of the skin on the palmar aspect of the hands, usually over the hypothenar eminence. It may also involve the thenar eminence and fingers. It can also be found on the soles of the feet, when it is termed plantar erythema. | |
scleral icterus Hint: The yellowing of the "white of the eye" is thus more properly termed conjunctival icterus. The term "icterus" itself is sometimes incorrectly used to refer to jaundice that is noted in the sclera of the eyes, however its more common and more correct meaning is entirely synonymous with jaundice. |
|
List |
References: Merck Manual · UpToDate