15-month-old with vomiting, diarrhea, and poor appetite
Patient will present as → an 11-year-old boy who is brought to the clinic for diarrhea and vomiting. He has no fever but complains of intermittent, cramping, and abdominal pain. They just returned from a family picnic, where about two hours ago the child ate potato salad. The mother reports other family members had become ill after the meal as well.
To watch this and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
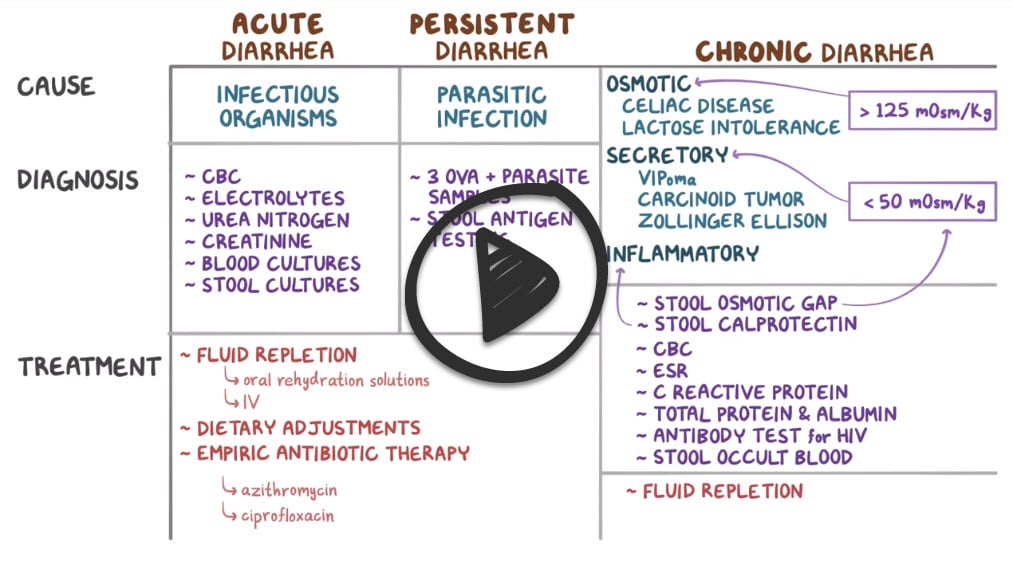
Causes of diarrhea may be infectious, toxic, dietary (excessive laxative use) or other GI disease. Inflammatory diarrhea (bloody diarrhea with fever) indicates an invasive organism or inflammatory bowel disease.
- Traveler's diarrhea: e-coli
- Diarrhea after a picnic and egg salad: Staphylococcus Aureus
- Diarrhea from shellfish: Vibrio cholerae
- Diarrhea from poultry or pork: Salmonella
- Diarrhea in a patient post antibiotics: C. Difficile
- Diarrhea in poorly canned home foods: C. perfringens
- Diarrhea breakout in a daycare center: Rotavirus
- Diarrhea on a cruise ship: Norovirus
- Diarrhea after drinking (not so) fresh mountain stream water: Giardia lamblia - incubates for 1-3 weeks, causes foul-smelling bulky stool, and may wax and wane over weeks before resolving
White blood cells in stool indicate an inflammatory process
- Culture for bacterial agents, microscopy for parasites, or toxin identification (E Coli or C.diff is suspected)
Acute diarrhea (< 4 days) typically does not require testing. Exceptions are patients with signs of dehydration, bloody stool, fever, severe pain, hypotension, or toxic features—particularly those who are very young or very old.
These patients should have a CBC and measurement of electrolytes, BUN, and creatinine.
Stool samples should be collected for microscopy, culture, fecal leukocyte testing, and, if antibiotics have been taken recently,C. difficile toxin assay.
Severe diarrhea requires fluid and electrolyte replacement to correct dehydration, electrolyte imbalance, and acidosis.
Parenteral fluids containing NaCl, KCl, and glucose are generally required. Salts to counteract acidosis (Na lactate, acetate, HCO 3 ) may be indicated if serum HCO 3 is < 15 mEq/L. An oral glucose-electrolyte solution can be given if diarrhea is not severe and nausea and vomiting are minimal. Oral and parenteral fluids are sometimes given simultaneously when water and electrolytes must be replaced in massive amounts (eg, in cholera).
Diarrhea is a symptom. When possible, the underlying disorder should be treated, but symptomatic treatment is often necessary.
Diarrhea may be decreased by
- oral loperamide 2 to 4 mg tid or qid (preferably given 30 min before meals)
- diphenoxylate 2.5 to 5 mg (tablets or liquid) tid or qid
- codeine phosphate 15 to 30 mg bid or tid
- or paregoric (camphorated opium tincture) 5 to 10 mL once/day to qid.
Because antidiarrheals may exacerbate C. difficile colitis or increase the likelihood of hemolytic-uremic syndrome in Shiga toxin-producing Escherichia coli infection, they should not be used in bloody diarrhea of unknown cause. Their use should be restricted to patients with watery diarrhea and no signs of systemic toxicity. However, there is little evidence to justify previous concerns about prolonging the excretion of possible bacterial pathogens with antidiarrheals.
 Osmosis Osmosis |
|
 |
Norovirus is a genus of virus in the calicivirus family, which leads to acute gastroenteritis in the infected. It is the most common cause of viral gastroenteritis in the world, and the disease is typically self-limited.
Question 1 |
Salmonella | |
Staphylococci Hint: Causes diarrhea following ingestion of improperly stored food with high salt content. | |
C. perfringens Hint: Causes diarrhea following ingestion of inadequately cooked meat, poultry, or legumes. | |
Giardia lamblia Hint: Causes diarrhea following ingestion of contaminated water. |
Question 2 |
Salmonella Hint: Is a cause of diarrhea following food poisoning. | |
Rotavirus Hint: Is a common cause of diarrhea in children. Less common in adults. Doesn’t occur as a result of recent use of antibiotics. | |
Clostridium difficile | |
E. coli Hint: Is a cause of diarrhea following food poisoning. |
Question 3 |
Empirical antibiotic therapy. Hint: Not necessary as the diarrhea is likely not infectious/non inflammatory. | |
Prescribe an antidiarrheal agent. | |
Stool culture. Hint: See B for explanation | |
Stool for ova and parasite. Hint: See B for explanation |
Question 4 |
Oral rehydration | |
Intravenous rehydration | |
Stool culture | |
Empirical antibiotics |
Question 5 |
45 mmol Na+, 20 mmol K+, 70 mmol Cl−, 100 mmol citrate, and 110 mmol glucose | |
50 mmol Na+, 30 mmol K+, 80 mmol Cl−, 10 mmol citrate, and 100 mmol glucose | |
90 mmol Na+, 20 mmol K+, 80 mmol Cl−, 10 mmol citrate, and 111 mmol glucose | |
90 mmol Na+, 30 mmol K+, 80 mmol Cl−, 20 mmol citrate, and 111 mmol glucose |
Question 6 |
Salmonella | |
Shigella | |
Campylobacter | |
Escherichia coli | |
Enterococcus |
Question 7 |
Shigella | |
Salmonella | |
enteroinvasive E. coli | |
all of the above |
Question 8 |
infection is transmitted by undercooked ground beef, unpasteurized milk, and other vehicles contaminated with bovine feces Hint: See C for answer | |
outbreaks have been linked to contaminated apple cider, raw vegetables, and drinking water Hint: See C for answer | |
person-to-person transmission is uncommon in outbreaks | |
the dose necessary to cause infection is low Hint: See C for answer | |
hemolytic-uremic syndrome is a serious complication of infection Hint: See C for answer |
Question 9 |
ampicillin | |
clindamycin | |
amoxicillin | |
cephalosporins | |
all of the above |
Question 10 |
attempt oral rehydration therapy Hint: See C for explanation | |
perform a venous cutdown in the ankle Hint: See C for explanation | |
begin an interosseous infusion | |
begin a subcutaneous infusion Hint: See C for explanation |
Question 11 |
urine specific gravity Hint: See D for explanation | |
stool evaluation for blood Hint: See D for explanation | |
stool evaluation for fecal leukocytes Hint: See D for explanation | |
stool cultures | |
serum electrolytes Hint: See D for explanation |
Question 12 |
Vancomycin | |
Diphenoxylate/atropine (Lomotil) Hint: See A for explanation | |
Clindamycin Hint: See A for explanation | |
Ciprofloxacin Hint: See A for explanation |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture