Patient will present as → a 21-year-old male with hematemesis. He is brought by his girlfriend, who reports that he and his buddies have been out drinking every night last week in celebration of his 21st birthday. He reports having vomited each night, but tonight, when he started vomiting, he noticed that there was streaking of blood. Concerned, he decided to come to the emergency department.
To watch this, and all of Joe-Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
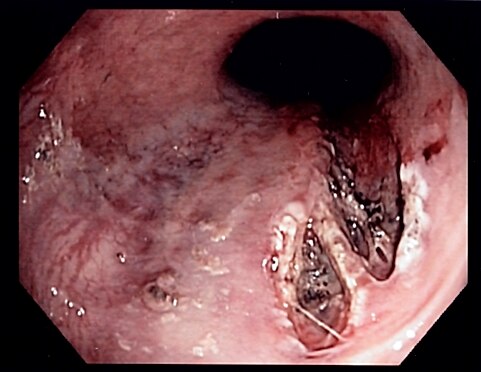
A Mallory-Weiss tear is a linear mucosal tear in the esophagus at the gastroesophageal junction
- Mallory-Weiss tears are the cause of 5-10% of all acute upper GI bleeds
- Patient with a history of alcohol intake and an episode of vomiting with blood
Diagnosed with upper endoscopy showing superficial longitudinal mucosal erosions
- CBC: assess for anemia secondary to bleeding
- Urea and electrolytes: raised urea (RBCs are digested into urea in upper GI bleed)
- Coagulation profile: assess underlying coagulopathy causing bleeding
- LFTs: if deranged, suggests variceal bleed
- CXR: to rule out esophageal perforation or perforated peptic ulcer
- Stool for blood
Generally self-limiting and bleeding stops on its own
1st-line: Upper GI endoscopy: diagnostic and therapeutic with:
- Clipping +/- adrenaline
- Thermal coagulation with adrenaline
- Sclerotherapy with adrenaline
High-dose IV PPI: to reduce rebleeding
Don't give before endoscopy as may mask bleeding
2nd-line: Surgical repair
 Osmosis Osmosis |
|
 |
Mallory-Weiss syndrome describes mucosal lacerations, leading to bleeding at the junction of the stomach and esophagus. This often results from forceful vomiting, which may be a consequence of eating disorders or alcoholism. Diagnosis is made through endoscopy, through which treatment (if needed) can also take place.
Play Video + QuizQuestion 1 |
Boerhaave syndrome Hint: Boerhaave syndrome is a full thickness tear/rupture of the distal esophagus following persistent retching and vomiting with recent excessive alcohol intake. There is usually associated sudden onset severe chest pain, fever, patient may be in shock, and subcutaneous emphysema. | |
Mallory-weiss tear | |
Bleeding esophageal varices Hint: Bleeding esophageal varices occur as a result of decompensating chronic liver disease. | |
Bleeding Peptic ulcer disease (PUD) Hint: Bleeding PUD does occur following vomiting and retching. There may be history chronic NSAID ingestion, epigastric pain associated with meals. Patient may be known to have PUD. |
Question 2 |
Chest X-ray Hint: Chest X-ray plays no role in diagnosing Mallory-weiss tear. | |
Barium swallow Hint: Barium swallow plays no role in diagnosing Mallory-weiss tear. | |
Barium meal Hint: Chest X-ray plays no role in diagnosing Mallory-weiss tear. | |
Esophagogastroscopy |
Question 3 |
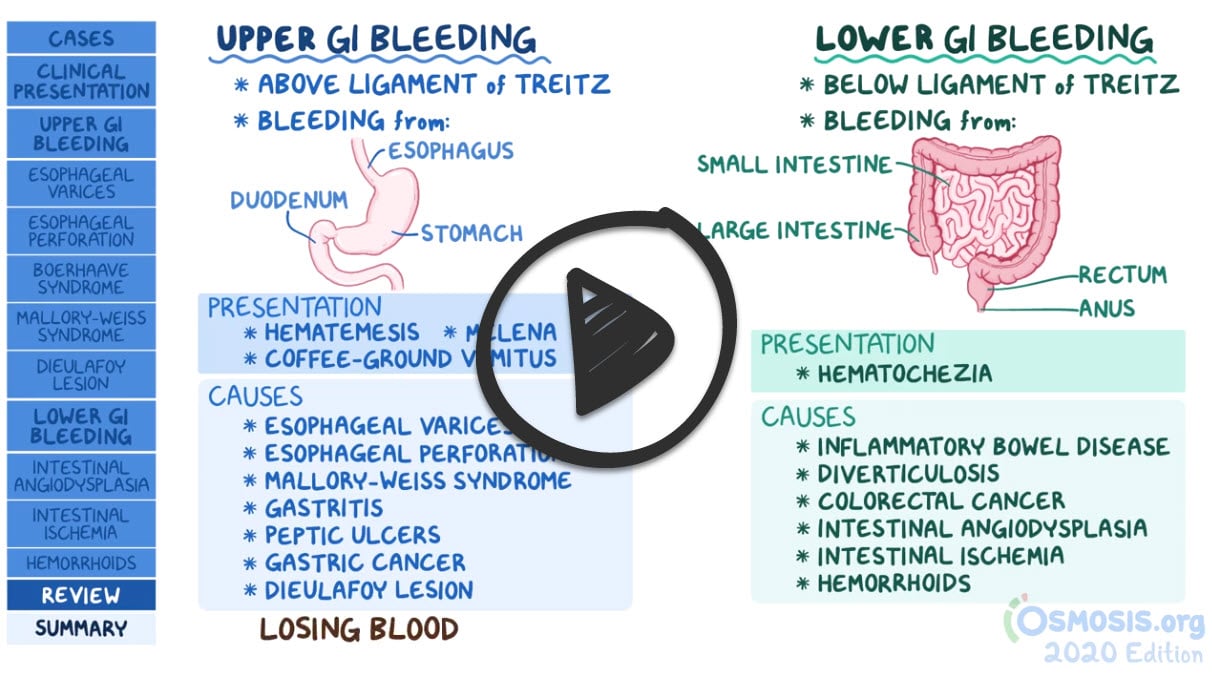
Mallory-Weiss syndrome Hint: Mallory-Weiss syndrome can cause upper gastrointestinal bleeding. | |
Gastritis Hint: Gastritis can cause upper gastrointestinal bleeding. | |
PUD Hint: PUD can cause upper gastrointestinal bleeding. | |
Diverticulosis |
Question 4 |
Sclerosant injection Hint: Sclerosant injection is done endoscopically. | |
Band ligation Hint: Band ligation is done endoscopically. | |
Angiotherapy | |
Hemoclip placement Hint: Hemoclip placement is done endoscopically. |
Question 5 |
Sneezing | |
Blunt abdominal trauma Hint: Blunt abdominal trauma is a known precipitating factor. | |
Hiccupping Hint: Hiccupping is a known precipitating factor. | |
Retching Hint: Retching is a known precipitating factor. |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture