The NCCPA™ Gastroenterology and Nutrition PANCE Content Blueprint covers 6 topics under the category of esophageal disorders
| Esophagitis (ReelDx) | ReelDx Virtual Rounds (Esophagitis)Patient will present as → a 54-year-old female with odynophagia (painful swallowing), dysphagia and retrosternal chest pain Esophagitis is simply inflammation that may damage tissues of the esophagus. It can be divided into two types: 1. Non-infectious
2 Infectious - odynophagia (pain while swallowing food or liquids) is the hallmark sign This occurs mainly in patients with impaired host defenses. Primary agents include Candida albicans, herpes simplex virus, and cytomegalovirus. Symptoms are odynophagia and chest pain
DX: Diagnosis is by endoscopy, biopsy, double contrast esophagram, and culture TX: Treat the underlying condition
|
| Gastroesophageal reflux disease | Patient will present as → a 55-year-old male with complaints of heartburn, belching, and epigastric pain which is aggravated by drinking coffee, eating fatty foods, and lying down. He says it gets better when he takes antacids. Retrosternal pain/burning shortly after eating worse with carbonation, greasy foods, spicy foods, and lying down DX: Patients with typical symptoms of GERD may be given a trial of PPI therapy. Patients who do not improve or have long-standing symptoms or symptoms of complications should be studied:
Treatment: H2 receptor blockers, proton pump inhibitors, diet modification (avoid fatty foods, coffee, alcohol, orange juice, chocolate; avoid large meals before bedtime); sleep with the trunk of body elevated; stop smoking
|
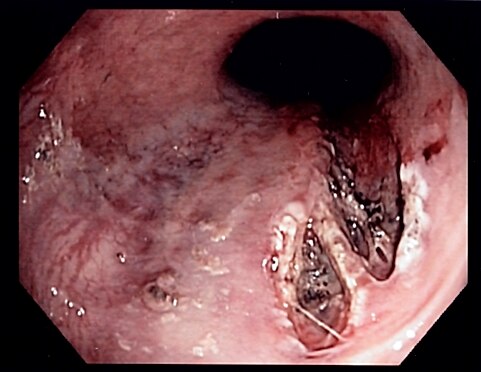
| Mallory Weiss tear | Patient will present as → a 21-year-old male with hematemesis. He is brought by his girlfriend who reports that he and his buddies have been out drinking every night last week in celebration of his 21st birthday. He reports having vomited each night, but tonight, when he started vomiting, he noticed that there was streaking of blood. Concerned, he decided to come to the emergency department. Tear that occurs in the esophageal mucosa at the junction of the esophagus and stomach caused by severe retching and vomiting and results in severe bleeding.
DX: Diagnosed with upper endoscopy showing superficial longitudinal mucosal erosions TX: Supportive. May cauterize or inject epinephrine if needed |
| Motility disorders | Patient presents as → a 46-year-old female complaining of difficulty swallowing solids and liquids. She also reports unintentional weight loss. (achalasia) Achalasia
 Upper gastrointestinal series. Barium swallow. Dilated esophagus with retained column of barium and “bird’s beaking” suggestive of achalasia. Diffuse esophageal spasm Patient presents as → a 26-year-old male is brought to the emergency department (ED) via ambulance with sudden onset of extreme chest pain. The patient states that he had just finished his morning run and was drinking from his water bottle when the pain began. He states that the pain was like “nothing he had experienced before” and radiated to his back, neck, and ears. He called EMS and was given 325mg aspirin, sublingual nitroglycerine, and supplemental oxygen in the field resulting in near resolution of his symptoms. In the ED, his exam is completely unremarkable except for a heart rate of 110 bpm. EKG shows sinus tachycardia, troponin and CK-MB are within normal limits, and stress test is normal. You order an upper GI contrast study which shows a corkscrew esophagus.
Neurogenic dysphagia Patient presents as → a 32-year-old female who reports to your office complaining of nasal regurgitation with the ingestion of fluids. Sure enough, when you hand her a glass of water, and she sips the liquid, it regurgitates out her nose. You make an immediate referral to the neurologist. Three months later, when the patient returns to your office, she explains that she has been diagnosed with multiple sclerosis. Neurogenic dysphagia is a result of the faulty transmission of nerve impulses to the pharyngeal muscles generally caused by an associated neuromuscular disease, such as myasthenia gravis, amyotrophic lateral sclerosis, MS, or stroke
Zenker diverticulum Patient presents as → a 68-year-old female who is being seen at the emergency department after having recurrent coughing spells and regurgitation following meals. Her breath is nearly unbearable upon arrival at the ED. She is also noted to have a palpable, fluctuant neck mass on physical examination. A pharyngeal pouch that develops in the proximal esophageal wall
Scleroderma esophagus Patient presents as → a 42-year-old female complaining of acid reflux and difficulty swallowing both solids and liquids. The patient also complains of sore swollen fingers, joint pains, and a dry cough. She reports that this started a year ago and has not improved. She has a past medical history of vitiligo and primary biliary cholangitis. Physical exam reveals tightened, shiny skin with induration over her face and arms, sclerodactyly, and dry rales in the lungs. There are also telangiectasias on her left cheek.
 Peptic stricture showing narrowing of the esophagus near the junction with the stomach due to chronic gastroesophageal reflux in the setting of scleroderma. Esophageal stenosis An esophageal stricture is a narrowing of the lumen of the esophagus, preventing the passage of food. Typically, it is at the distal end of the tube and is the result of scarring after chronic exposure to gastric juice due to GERD.
|
| Esophageal strictures | Patient will present with → solid food dysphagia in a patient with a history of GERD An esophageal stricture is an abnormal tightening or narrowing of the esophagus, making it more difficult for food to travel down the tube. People with esophageal strictures may have pain or difficulty swallowing
Obstructive Disorders of the Esophagus
An esophageal web is a thin mucosal membrane that grows across the lumen in the mid-upper esophagus and may cause dysphagia. It may be congenital or acquired
A lower esophageal ring (also called a Schatzki ring) is a 2- to 4-mm mucosal stricture that causes a ringlike narrowing of the distal esophagus at the squamocolumnar junction that often causes dysphagia.
Esophageal tumors (benign esophageal tumors or esophageal cancer) can also cause dysphagia Diagnosed by upper endoscopy to determine the underlying cause, exclude malignancy, and perform therapy (dilation) if needed
Treat with endoscopic dilation |
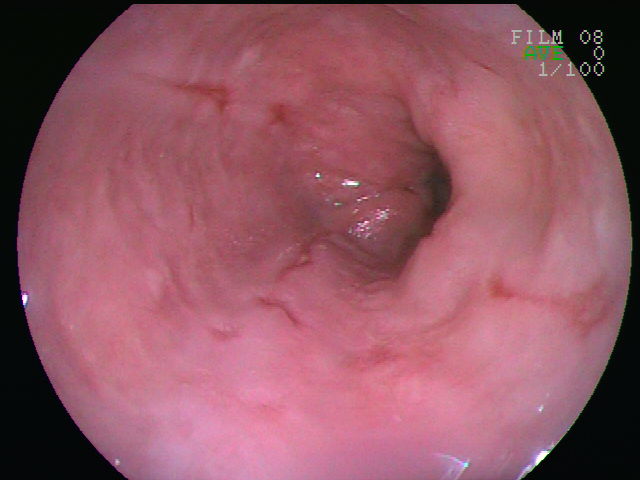
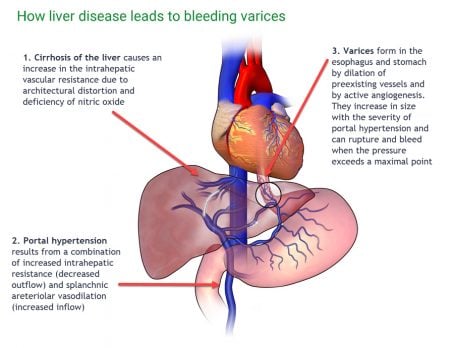
| Esophageal varices (ReelDx) | ReelDx Virtual Rounds (Esophageal varices)Patient will present as → a 64-year-old man with a history of alcoholism, tobacco use, and hypertension presents to the general surgery clinic, where he was referred for further evaluation of blood in his stool. He reports occasional abdominal pain relieved transiently with meals and one episode of painful vomiting. Recently, his stools have been black. Spider angiomas but no palmar erythema or hepatosplenomegaly are observed on the exam. Dilated veins in the distal esophagus or proximal stomach caused by elevated pressure in the portal venous system, typically from cirrhosis
DX: Perform emergent upper GI endoscopy (once the patient is stabilized) in all patients with GI bleed ⇒ diagnostic and can be therapeutic
Screening is indicated when cirrhosis or portal hypertension is diagnosed
Treatment: Therapeutic endoscopy – endoscopic banding and IV octreotide
|