Gastric ulcer: Patient will present with → abdominal discomfort that is worse with meals and gets better an hour or so later after eating.
Duodenal ulcer: Patient will present as → a 62-year-old female with complaints of epigastric pain and belching, which improves when she eats food but gets worse a few hours after her meal. She said he has noticed a change in the color of her stool.
PUD is an ulcer of the upper GI tract mucosa involving the proximal duodenum (duodenal ulcer~90%) and distal stomach (gastric ulcer~10%)
Duodenal ulcer (food classically decreases pain think Duodenum = Decreased pain with food)
- Duodenal ulcers are more than twice as common as gastric ulcers
- Duodenal ulcers are most commonly caused by H. pylori (95%)
- Pts typically present with epigastric pain that is better postprandial
- Usually located in the anterior duodenum ⇒ when present in the posterior duodenum can lead to bleeding from the gastroduodenal artery or cause acute pancreatitis
- Rarely, it can be caused by Zollinger-Ellison syndrome (this is a gastrinoma; a tumor of the pancreas that causes the stomach to produce too much gastrin with subsequent acid secretion leading to ulcer formation. Diagnosed with gastrin levels >200 pg/mL)
Gastric ulcer (food classically causes pain)
- Gastric ulcers are most commonly caused by H. pylori. It can also be caused by NSAIDs, acid reflux, smoking
- Pain is described as gnawing or burning and usually radiates to the back
- Patients typically present with epigastric pain that is worse with food (postprandial)
- It is most commonly found at the lesser curvature of the antrum
PUD is the MC cause of non-hemorrhagic GI bleed, typically presenting as hematemesis (either red blood or coffee-ground emesis), or melena (black, tarry stool
Upper endoscopy is the most accurate diagnostic test for peptic ulcer disease
- Biopsy for H. pylori should be obtained in all patients undergoing upper endoscopy for PUD unless contraindicated
- Biopsy of ulcers for benign-appearing ulcers is not recommended ⇒ all ulcers with malignant features should be biopsied
- Ruptured ulcer - elevated serum amylase and free air under the diaphragm seen on upright film make the diagnosis
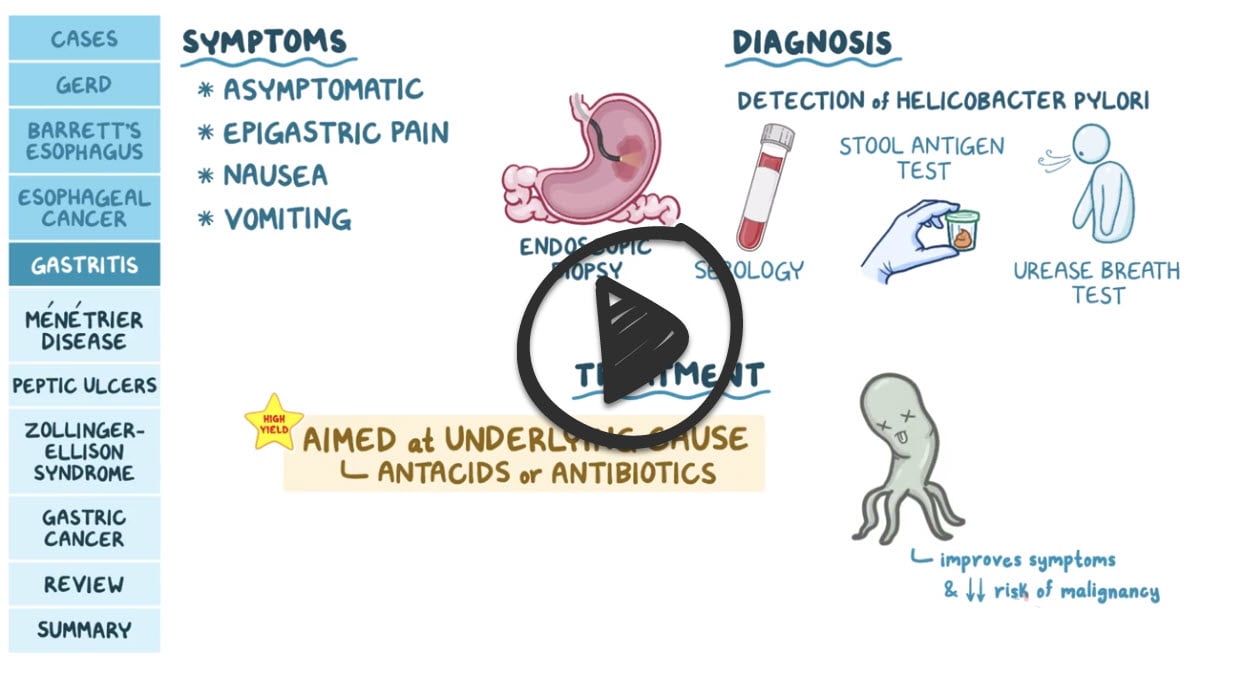
- Antibody Testing (serology) detects IgG antibodies in serum, whole blood, or urine. Avoid use in patients previously treated for H. pylori. It does not necessarily delineate between active and previous infection
- Urea Breath Test (UBT). Can be used to test for active infection and evaluate for eradication
- Fecal Antigen Test. Can be used to test for active infection and evaluate for eradication
- False negatives possible with recent use of PPIs, antibiotics, or bismuth
All patients with peptic ulcers should receive antisecretory therapy with a proton pump inhibitor (PPI) (e.g., omeprazole 20 to 40 mg daily or equivalent) for 4-8 weeks
- Patients with evidence of H. pylori on biopsy should receive eradication therapy
- Triple therapy: PPI + Amoxicillin 1g PO BID or Metronidazole 250 mg QID + Clarithromycin 500 mg PO BID (think baseball "CAP" = Clarithromycin + Amoxicillin + PPI)
- Quadruple therapy: PPI + Bismuth subsalicylate 524 mg 4 times a day + Metronidazole 250 mg 4 times a day + Tetracycline 500 mg 4 times a day
- Best initial therapy in areas where the clarithromycin resistance rate is > 15%
- In patients with active bleeding, a negative biopsy result does not exclude H. pylori, and a breath test or a stool antigen test for H. pylori should be performed to confirm a negative result
- In patients who receive treatment for H. pylori, eradication should be confirmed four or more weeks after the completion of therapy
Discontinue nonsteroidal anti-inflammatory drugs (NSAIDs)
- Patients with NSAID-associated ulcers should be treated with a PPI for a minimum of eight weeks
- PPI therapy for four to eight weeks in patients with H. pylori-negative ulcers that are not associated with NSAID use
- Zollinger-Ellison syndrome: PPI and resect the tumor
- Patients with duodenal ulcers who have been treated do not need further endoscopy unless symptoms persist at four weeks or recur
In the event of rupture - immediate surgical intervention is required for treatment.
 Osmosis Osmosis |
|
 |
 Peptic ulcers are caused by an erosion of the mucosal wall of the gastrointestinal tract. These ulcers develop when excess hydrochloric acid and digestive enzymes (pepsin) disrupt the gastric mucosal barrier, causing breakdown. A bacteria called Helicobacter pylori (H. pylori) may also contribute to peptic ulcer formation; however, not everyone who is infected with this bacteria will develop an ulcer. Patients with this condition may present with abdominal pain, heartburn, GI distress, black, tarry stools, and weight loss.
Peptic ulcers are caused by an erosion of the mucosal wall of the gastrointestinal tract. These ulcers develop when excess hydrochloric acid and digestive enzymes (pepsin) disrupt the gastric mucosal barrier, causing breakdown. A bacteria called Helicobacter pylori (H. pylori) may also contribute to peptic ulcer formation; however, not everyone who is infected with this bacteria will develop an ulcer. Patients with this condition may present with abdominal pain, heartburn, GI distress, black, tarry stools, and weight loss.
| Peptic Ulcer Disease Assessment | Play Video + Quiz |
| Peptic Ulcer Disease Interventions | Play Video + Quiz |
Zollinger-Ellison syndrome (ZES)
 Zollinger-Ellison syndrome (ZES) is caused by gastrin-secreting tumors, known as gastrinomas. The sequelae of this disease are the result of excess gastric acid production, which leads to abdominal pain, heartburn, diarrhea and ulcers in patients. These ulcers present most commonly in the proximal duodenum, and less commonly in the distal duodenum and jejunum. Furthermore, these are usually solitary ulcers. Patients may present with gastrointestinal bleeding as well. Abdominal pain and heartburn occur secondary to gastroesophageal reflux disease (GERD), which develops in roughly 50% of patients with Zollinger-Ellison syndrome. The gastrinomas of this disease can be sporadic and can occur without any other disease present. However, an important correlation of this disease is that 25% of cases are associated with multiple endocrine neoplasia type 1 (MEN 1).
Zollinger-Ellison syndrome (ZES) is caused by gastrin-secreting tumors, known as gastrinomas. The sequelae of this disease are the result of excess gastric acid production, which leads to abdominal pain, heartburn, diarrhea and ulcers in patients. These ulcers present most commonly in the proximal duodenum, and less commonly in the distal duodenum and jejunum. Furthermore, these are usually solitary ulcers. Patients may present with gastrointestinal bleeding as well. Abdominal pain and heartburn occur secondary to gastroesophageal reflux disease (GERD), which develops in roughly 50% of patients with Zollinger-Ellison syndrome. The gastrinomas of this disease can be sporadic and can occur without any other disease present. However, an important correlation of this disease is that 25% of cases are associated with multiple endocrine neoplasia type 1 (MEN 1).
| Zollinger-Ellison Syndrome Disease | Play Video + Quiz |
| Zollinger-Ellison Syndrome Diagnosis and Treatment | Play Video + Quiz |
Helicobacter Pylori
Helicobacter pylori is a gram-negative bacillus with multiple flagella that causes gastritis and peptic ulcer disease (PUD). H. pylori is the most common cause of gastric and duodenal ulcers. It survives in the stomach’s acidic environment by producing urease, which converts urea to ammonia and makes the stomach more alkaline. It disrupts the stomach’s mucous layer which leaves the underlying tissue susceptible to damage and also elicits an inflammatory reaction resulting in chronic gastritis. As a result, long term complications include gastric adenocarcinoma and MALT lymphoma. Detection of H. pylori infection is made by IgG serology, stool antigen assay, urease positive breath test or an endoscopic biopsy. Treatment is a combination of two antibiotics, typically clarithromycin and either amoxicillin or metronidazole, as well as a proton-pump inhibitor (PPI).
| Helicobacter Pylori | Play Video + Quiz |
Peptic Ulcer Disease Treatments
 Proton pump inhibitors are a class of drugs that act directly on the H+/K+/ATPase pump to prevent secretion of acid. They are indicated for GERD, peptic ulcer disease, treatment of gastritis and for gastrinomas, such as Zollinger-Ellison syndrome. These drugs are easy to remember, as they share a common suffix, “prazole,” exemplified by the medication omeprazole. Common side effects of these medications include hip fracture, as this drug class decreases calcium absorption, as well as pneumonia, due to bacterial overgrowth in a less acidic environment.
Proton pump inhibitors are a class of drugs that act directly on the H+/K+/ATPase pump to prevent secretion of acid. They are indicated for GERD, peptic ulcer disease, treatment of gastritis and for gastrinomas, such as Zollinger-Ellison syndrome. These drugs are easy to remember, as they share a common suffix, “prazole,” exemplified by the medication omeprazole. Common side effects of these medications include hip fracture, as this drug class decreases calcium absorption, as well as pneumonia, due to bacterial overgrowth in a less acidic environment.
| Proton Pump Inhibitors (PPIs) | Play Video + Quiz |
| Sucralfate (Carafate) | Play Video + Quiz |
| Cimetidine and Ranitidine (H2 Receptor Blockers) | Play Video + Quiz |
| H2 Blocker Side Effects | Play Video + Quiz |
Question 1 |
duodenal ulcer | |
gastric ulcer Hint: Gastric ulcer causes abdominal discomfort that is worse with meals and gets better an hour or so later after eating. | |
acute cholecystitis Hint: RUQ pain and + Murphy's sign |
Question 2 |
Duodenal ulcer | |
Gastic Ulcer | |
Acute pancreatitis Hint: Acute pancreatitis can cause epigastric pain which is usually sudden in onset and gradually intensifies in severity until reaching a constant ache. Patient would usually present at the emergency looking toxic especially when severe. |
Question 3 |
Amoxicillin | |
Clarithromycin | |
A proton pump inhibitor | |
Bismuth |
Question 4 |
Esophagitis Hint: Pain from esophagitis is usually retrosternal. Most patients complain of heartburn due to acid reflux. There is no periodicity and association with food. | |
Acute pancreatitis Hint: Acute pancreatitis can cause epigastric pain which is usually sudden in onset and gradually intensifies in severity until reaching a constant ache. Patient would usually present at the emergency looking toxic especially when severe. There is no association with chronic NSAID use. | |
Peptic ulcer disease | |
Gastroesophageal reflux disease Hint: GERD presents with heartburn which has no periodicity, and regurgitation. |
Question 5 |
Upper gastrointestinal endoscopy | |
Double-contrast barium enema Hint: Double-contrast barium enema is not as sensitive as endoscopy for establishing a diagnosis of small ulcers (<0.5cm). It also does not allow for obtaining a biopsy. | |
Chest radiograph Hint: Chest radiograph may be useful to detect free abdominal air when perforation is suspected. It cannot diagnose PUD. | |
None of the above |
Question 6 |
superior acid suppression | |
faster healing rates | |
safe for use in hepatically impaired patients | |
faster symptom relief | |
lower and less frequent dosing requirement |
Question 7 |
stool antigen test | |
urea breath test | |
enzyme-linked immunosorbent assay (ELISA) serology | |
Steiner stain of gastric biopsy specimen |
|
List |
References: Merck Manual · UpToDate