Hepatitis management starts with prevention!
Patient will present as → a 38-year-old female who has just returned from a 2-week trip to Mexico. She complains of nausea, vomiting, loss of appetite, and right upper quadrant abdominal pain. She has been sick for the past 3 days. She complains of passing dark-colored urine for the past 2 days. She has had no exposure to blood products, has no history of intravenous drug use, and has no significant risk factors for sexually transmitted disease. On examination, she looks acutely ill. Her pulse is 100 beats/minute, blood pressure 110/70 mm Hg, respirations 18, and temperature 101°F. Her sclerae are icteric, and her liver edge is tender.
To watch this and all of Joe Gilboy PA-C's video lessons you must be a member. Members can log in here or join now.
There are five types of Viral Hepatitis
1. Hepatitis A (25-year-old patient in the clinical case presentation)
- Fecal-oral transmission
- Look for recent travel to Asia
- Hepatomegaly + jaundice
- Fatigue malaise, nausea, vomiting, anorexia, fever, and right upper quadrant pain
- Jaundice typically peaks within two weeks
- Contagious until 1 week of jaundice
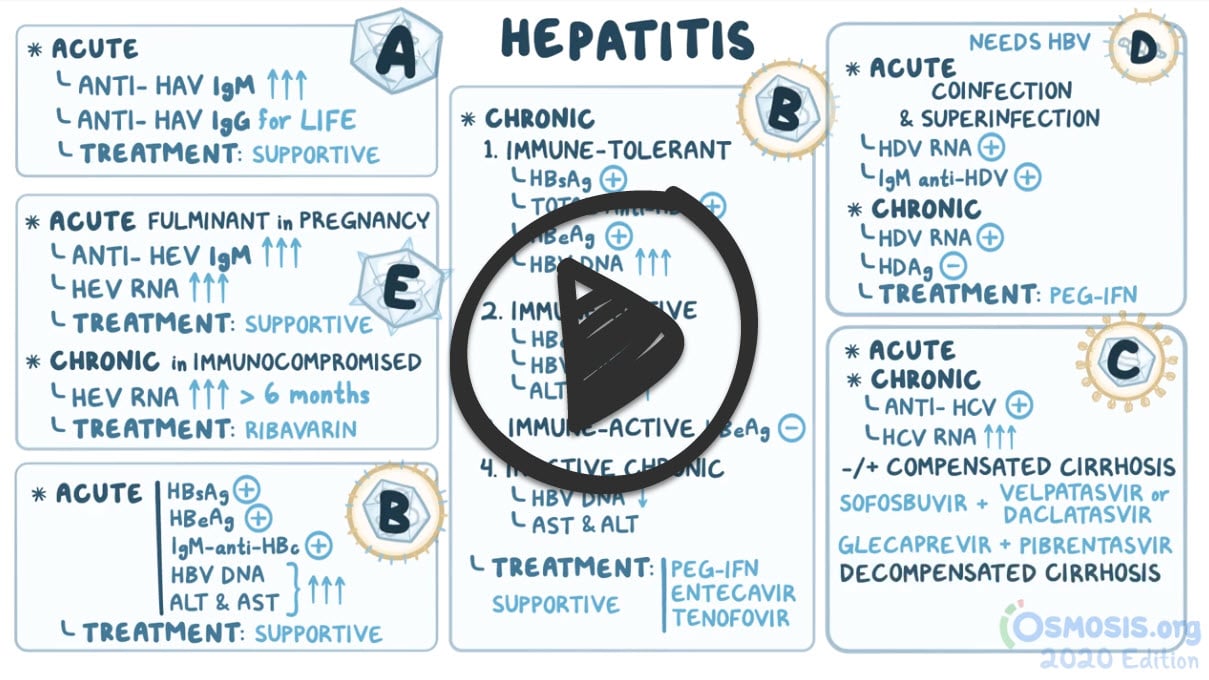
- Diagnosis is serum IgM anti-HAV
- Once exposed they have a life-long immunity
- for family member give IV-IGg
2. Hepatitis B
Patient will present as → a 35-year-old male with bright yellow discoloration of his skin. He states that this started yesterday and has been getting progressively worse. Upon obtaining further history you learn that this patient has recently lost 10 pounds over the past month and has had urine that he believes is darker. The patient is currently sexually active with women and does not use protection. On physical exam, you note the patient has prominent scleral icterus.
- Transmission from needles, sex, mom to child, close contact
- Flu-like symptoms + jaundice
- May lead to cirrhosis and liver failure
- If anti-HBs (HepBSAb) is POSITIVE then you have some type of immunity
- If HBsAg is POSITIVE then infection is present
- Anti-HBc IgM acute, Anti-HBc IgG (resolved or chronic)
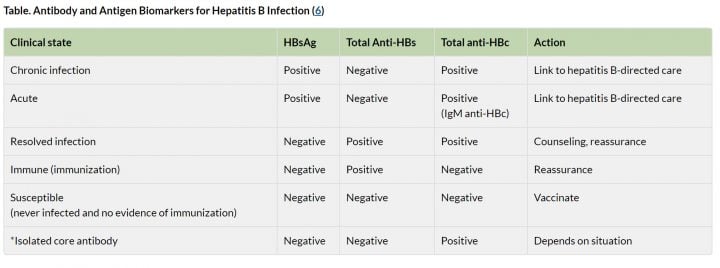
See "Diagnostic Studies" tab for full breakdown of Hep B serology
3. Hepatitis C
Patient will present as → a 55-year-old man who is referred to your clinic after abnormal blood workup noted at a Red Cross blood donation site. The man reports having donated blood 30 years ago without any serologic abnormalities. The patient appears healthy and denies any history of blood transfusion or IV drug use. On further questioning, the man reports having been stuck by a needle while working as a phlebotomist 20 years ago which he never reported. Lab results reveal positive anti-HCV antibodies. Subsequent HCV genotyping and HCV RNA levels for this patient reveals genotype 1 and RNA levels of 100,000,000 IU/mL.
- Acute symptoms look like the flu with RUQ pain similar to hepatitis A
- Transmission by needles, blood contact (IV drug use is most common route of infection)
- 85% of patients with acute infection develop chronic disease
- Increased risk for hepatocellular carcinoma
- Screen with testing for anti-HCV antibodies
- Diagnosis with HCV RNA quant
- Direct acting antiretrovirals target complex of enzymes needed for HCV RNA synthesis (sofosbuvir, grazoprevir, daclatasvir)
4. Hepatitis D
- Only occurs with Hepatitis B and causes more severe hepatitis and faster progression to cirrhosis
- Transmission via clotting factors and drug users
5. Hepatitis E
- Fecal-oral transmission (similar to Hep A) associated with waterborne outbreaks, self-limiting infection
- Hepatitis E + mother = high infant mortality (20-30%)
- Diagnose with IgM anti-HEV
Hepatitis B Serology
| Anti-HBc IgM | Anti-HBc IgG | HBsAG | Anti-HBs | Interpretation |
| + | - | + | - | Acute HBV |
| - | - | + | - | Early acute HBV |
| - | + | - | + | Resolved acute HBV |
| - | - | - | + | HBV vaccine/Immunity |
| - | - | - | - | No infection or immunity |
| - | + | + | - | Chronic HBV |
Key points:
- If anti-HBs (HepBSAb) is POSITIVE then you have some type of immunity
- If HBsAg is POSITIVE then infection is present
- Look at IgM or IgG to decide if it is acute or chronic/resolved
Hepatitis C Serology
The USPSTF recommends screening for hepatitis C in adults aged 18-79 years.
- One-time testing in all adults and periodic testing in people at continued risk of new HCV infection (IV drug users)
- There is limited evidence to determine how often to screen persons at increased risk
| HCV RNA | Anti-HCV | |
| Acute Hepatitis C | + | ± |
| Resolved Hepatitis C | - | ± |
| Chronic Hepatitis C | + | + |
Hepatitis A Serology
| IgM HAV Ab | IgG HAV Ab | |
| Acute Hepatitis A | + | |
| Past exposure | - | + |
Hepatitis A Treatment
Self-limiting - symptomatic treatment, usually recovers in weeks
- Post-exposure prophylaxis for close contacts: HAV immune globulin
- Vaccination (given at 12 months)
Hepatitis C Treatment
All patients with virologic evidence of chronic HCV infection (ie, detectable HCV viral level over a six-month period) should be considered for treatment. Treatment depends on the genotype and presence of cirrhosis
- Without cirrhosis: Sofosbuvir (Sovaldi) coupled with either velpatasvir or daclatasvir for 12 weeks or by using Glecaprevir and pibrentasvir for 8 weeks.
- With compensated cirrhosis: Sofosbuvir and velpatasvir can be used for 12 weeks or Glecaprevir and Pibrentasvir can be given for 12 weeks or Sofosbuvir and daclatasvir can be given for 24 weeks.
- With decompensated cirrhosis, sofosbuvir plus velpatasvir for 24 weeks or sofosbuvir plus daclatasvir for 12 weeks can be used and some cases may require liver transplantation.
Hepatitis B Treatment
- Acute treatment is supportive
- Chronic treatment of patients with (+) HBsAg and (+) HBV DNA - if ↑ ALT, inflammation on liver biopsy or (+) HBeAg is alpha-interferon 2b, lamivudine, adefovir
- Give Hep B Vaccine at 0,1 and 6 months
Hepatitis D Treatment
- Treatment includes PEG-IFN for 12 months
Hepatitis E Treatment
- Acute treatment is supportive
- With chronic hepatitis E, HEV-RNA is detected in the stool or serum for more than 6 months and ribavirin can be used
 Osmosis Osmosis |
|
 |
Hepatitis C virus (HCV) is an enveloped SS+ linear RNA virus that is part of the Flavivirus family and is a major cause of liver disease worldwide. In the United States, most cases are due to intravenous drug abuse. In the past, HCV was often related to post-transfusion hepatitis caused by transmission of HCV in contaminated blood products. However, the incidence of post transfusion hepatitis has dramatically decreased as a result of increased screening procedures. In contrast to HBV infection, progression to chronic disease occurs in the majority of HCV infected individuals. Chronic inflammation of the liver can lead to cirrhosis and hepatocellular carcinoma. Due to the high incidence of chronic progression, HCV is the most common cause of infectious chronic liver disease in the United States and also the most common indication for liver transplantation. HCV infection is also associated with type 1 MPGN and porphyria cutanea tarda disease.
Play Video + QuizHepatitis A Virus
Hepatitis A is an infectious acute disease of the liver caused by the hepatitis A virus (HAV). The hepatitis A virus is a member of the picornavirus family and an enterovirus spread via the fecal-oral route with an average incubation period of 4 weeks. The incidence of hepatitis A is much higher in developing countries and regions with poor hygiene. In these areas, the illness is often contracted in early childhood and rarely causes clinical signs and symptoms. In industrialized countries, the infection is often contracted by susceptible adults who get infected by the virus during trips to countries with high incidence of disease. In most individuals, HAV infection causes a self-limited disease that does not result in chronic infection. Patients that are not asymptomatic have symptoms of jaundice, fever, and vomiting. Acute liver failure from HAV is rare.
Hepatitis B Virus (HBV)
Hepatitis B Virus (HBV) is in the Hepadnavirus family and is an enveloped DNA virus with a partially double-stranded circular genome. This virus can produce several disease types including acute hepatitis with recovery and clearance of the virus, a nonprogressive chronic hepatitis, progressive chronic disease resulting in cirrhosis, and fulminant hepatitis with massive liver necrosis. Patients can also be asymptomatic carriers. HBV induced chronic liver disease is also an important precursor for the development of hepatocellular carcinoma of the liver. In the United States, acute HBV infections typically affect adults and the majority of individuals have mild or no symptoms. Some experience nonspecific constitutional symptoms such as fever, anorexia, RUQ pain, or jaundice and is usually self-limited. In areas of high prevalence of HBV, perinatal transmission is common. When infants are affected via perinatal transmission, the rate of becoming a chronic carrier is significantly increased, with approximately 90% of newborns with HBV becoming a chronic carrier as compared to 10% of adults who become chronic carriers. HBV is commonly associated with several other diseases including membranous glomerulonephritis, polyarteritis nodosa, and a serum sickness-like syndrome.
Play Video + QuizQuestion 1 |
Cholecystitis | |
Ascending cholangitis | |
Hepatocellular carcinoma | |
Hepatitis B | |
Hepatitis A |
Question 2 |
Hepatitis E | |
Hepatitis C | |
Hepatitis D | |
Hepatitis A |
Question 3 |
Hepatitis D Hint: Hepatitis D is transmitted via blood. | |
Hepatitis A | |
Hepatitis C Hint: Hepatitis C is transmitted via blood and blood products through Intravenous drug misuse, unscreened blood products, needle stick injury, vertical transmission etc | |
Hepatitis B Hint: Hepatitis B can be transmitted via blood and blood products through Close living quarters/playground play as a toddler, vertical transmission, infected unscreened blood, needle stick injury etc. |
Question 4 |
Acute hepatitis B infection Hint: In Acute hepatitis B infection, hepatitis B surface antigen (present for < than 6 months) and no antibody will be seen. IgM antibody to hepatitis B core antigen will be raised. | |
Chronic active hepatitis B infection Hint: In chronic active hepatitis B infection, hepatitis B surface antigen (present > than 6 months) and no antibody will be seen. IgG antibody to hepatitis B core antigen will be raised. | |
Previous hepatitis B vaccination Hint: In previous hepatitis B vaccination, only antibody to hepatitis B surface antigen will be seen. | |
Previous hepatitis B infection |
Question 5 |
Hepatitis D | |
Hepatitis E | |
Hepatitis A | |
Hepatitis B | |
Hepatitis C |
Question 6 |
Early acute HBV Hint: HBsAg | |
Resolved acute HBV | |
Acute HBV Hint: Anti-HBc IgM and HBsAG | |
HBV vaccine/immunity Hint: Anti-HBs | |
Chronic HBV Hint: HBSAg + Anti HBC-IgG |
Question 7 |
Hepatitis A | |
Hepatitis D | |
Hepatitis C | |
Hepatitis B |
Question 8 |
hepatitis A Hint: Hepatitis A does not progress to chronic active hepatitis | |
hepatitis B Hint: Hepatitis B progresses to chronic active hepatitis and subsequently to cirrhosis in up to 10% to 15% of cases. | |
hepatitis C | |
alcoholism Hint: see answer for explanation |
Question 9 |
Entecavir Hint: Entecavir is very effective and reduces HBV DNA quickly, and there is little viral resistance. Serum HBV DNA becomes negative in 67% (HBeAg-positive patients) and 90% (HBeAg-negative patients) by 48 weeks. It should not be used in patients with lamivudine-induced mutants. | |
Tenofovir Hint: Tenofovir is also very effective, has a similar potency to entecavir, and as yet no resistance mutants have been described. It is used for HIV patients with HBV infection. It can also be used in patients with lamivudine mutations. | |
Lamivudine Hint: Lamivudine is well tolerated. However, by 4 years, 80% develop viral resistance due to YMDD mutant (tyrosine (Y), methionine (M), aspartate (D)), which itself causes hepatitis. Lamivudine monotherapy is no longer recommended. | |
Acyclovir |
Question 10 |
Sicca syndrome | |
Lichen planus | |
Lymphadenopathy | |
Arthralgia |
Question 11 |
HCV RNA assays | |
Hepatitis C antibody test | |
Recombinant immunoblot assay | |
Liver biopsy |
|
List |
References: Merck Manual · UpToDate


 Lecture
Lecture